Designing Medical Records Forms and Folders
Introduction
All hospitals have the responsibility to develop medical record forms as per their requirements. Thoughtful designs of the forms will become part of the medical record, that will provide a more readable, useful, and less bulky document. Forms can accomplish several purposes: they can reduce writing time and standardisation of information results from their use. Well designed forms are also easier to fill up.
The first and most important step in form designing is to determine the purpose of the form. Is the form really necessary? What benefits will be derived from introduction of the form into the record? The purposes of the form will in turn determine the information to be included on it. Unnecessary information must not be included.
Principles of forms designing
In the development of a new form, it is advisable to have only a small supply of forms prepared for trial use, because experience frequently indicates a need for revisions. Since cost is also a factor in continually revising and printing small quantities of forms, photocopying might be the method of choice. Forms should be kept simple and the variety must be few in number to provide flexibility and reduce bulky record. All discontinued forms should be removed from the stockroom or supply area and destroyed.
Before a new form is developed or an existing form is revised, the following steps can be used to compile the necessary facts and to determine what, if any, improvements should be made.
The principles for designing a standard forms
- A uniform size of paper should be used. Although standard size (8 ½ -inch - by 11-inch) paper is most commonly used, 8-½ -inch- by -5 ½ -inch papers could be used to reduce waste.
- A uniform binding should be maintained, either on top or side.
- A uniform margin that is based on the binding edge should be maintained.
- For top binding, information on forms that are to be printed on both sides should be correctly placed on both sides for proper assembly in the chart. For side binding the two sides should be placed head-to-head.
- Line spaces should be assigned on the basis of whether the forms are to be typewritten, handwritten, or both.
- Good quality paper should be used. If both sides are to be printed, the paper must be heavy enough to prevent the ink from showing through.
- Colored forms should be selected carefully because problems can occur in photocopying or microfilming colored sheets. White paper with color-coded borders will prove more effective for quick identification of different forms in the hard-copy record.
- When feasible, using a rubber stamp on an existing form can eliminate the need for special form that is not used regularly
The printer can ordinarily give advice on the physical aspects of printed forms - the kind and size of types, margins, paper color and weight, ink, and size of the form. Remember that standard - size forms are always less expensive, facilitate filing, preclude loss, which is often the case with irregular paper sizes. Keep in mind also that different colors of paper and ink will affect photocopying and microfilming in different ways.
Duplicating methods
Several persons or departments often need similar patient data. In such situations it is well to consider the possibility of a multipart form or a method to produce multiple copies. Multipart forms should be used whenever possible to
- Save time and labor;
- Avoid errors
- Promote rapid intra hospital communication of essential data; and
- Meet the need for extra copies.
The various methods of producing copies or duplicates are:
The effectiveness of legible carbon copies is limited to two or three copies. Carbon copies may be of three types:
- Loose carbon inserted between forms. The inserting and removing of carbon paper makes this method time-consuming. In addition, care must be taken to ensure that the information on all copies is lined up exactly or entries will appear above or below the space indicated.
- Snap-out or interleaved forms with one-time carbon previously inserted by the printer. Snap-out forms are widely used for reports of operations, discharge summaries, and dictated reports when copies are needed.
- Forms with carbonized backing are particularly effective for carbonizing specific portions of forms. However, the black carbonized portion rubs off and is more difficult to handle. This may be a disadvantage to consider.
- Stencils or master copies - this method is used to produce more copies than is possible with the above methods. Care must be taken to avoid methods which result in copies that will fade or in which legibility is poor.
- Photocopy equipment - this method is used to produce exact copies. Eliminating the need for a stencil saves time and labor.
Out Patient Records
Hospitals, which have an organised out-patient department, may maintain as many as twenty or more speciality clinics for out-patients. The records that are compiled in this setting should be compatible in size and format to those used for outpatients and inpatients in the facility. Each patient registered as an outpatient should have an initial history and physical examination, which should be brought up to date at regular intervals. Every clinic visit should be noted, including date, clinical finding, treatment, and names of those examining or caring for the patient.
Out- patient records are compiled in the outpatient department and should conform in size and form to the records used for hospitalised patients. On the subsequent clinic visits, noting as to findings and treatment should be made on the continuation note sheets. If the patient is admitted to the hospital, his outpatient record should be filed with the inpatient record as a unit, reflecting continuous medical care. These records should be checked as closely as those for hospitalized patients for accuracy in dates, time, spelling, and hospital numbers.
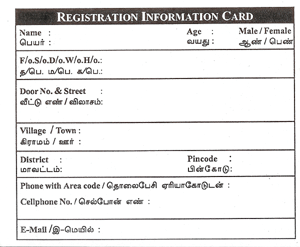
Information card
The primary purpose of information card is to collect the basic identifying information of patient. Identification data is ordinarily obtained at the time of patient registration. Therefore the patient medical file must include complete and correct identification data including: the hospital number, the patient’s name, and gender, date of birth (age), address, telephone number, cell phone number, e-mail address and relative’s name (Fig. 4.1).
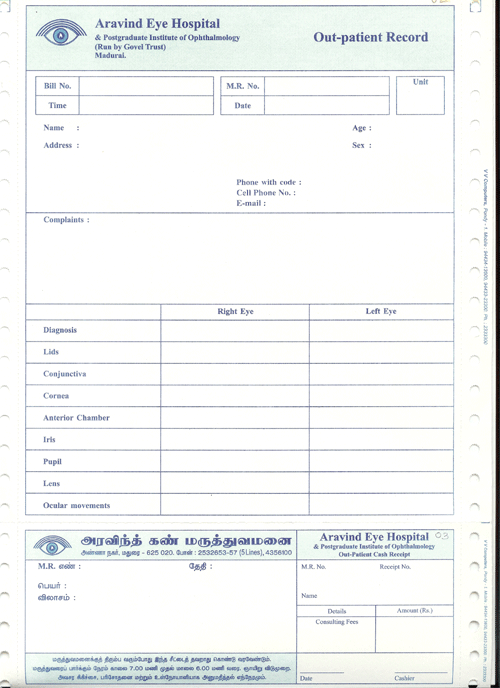
Outpatient main record
The out-patient record consists of outpatient (OP) main card and continuation sheet. The OP main card is basically used as a first record of document (Fig.4.2). This contains the identifying information of a patient with contact phone and cell phone numbers and e-mail address. The purpose of this sheet is to assist the doctors in getting the history and complaints of the patient thereby establishing a diagnosis on which to base the care and treatment of the patient. The essential facts should be given in a concise and progressive manner.
In addition basic tests like urine sugar, blood sugar and other physical tests like blood pressure of the patient are also recorded. Proper International Classification of Diseases (ICD) code should be recorded by the doctors in the space provided for the purpose after finalising the diagnosis of the patient. When the outpatient main card is fulfilled, additional sheets can be added to continue the progress and treatment of the patient. This continuation sheet is added to the record according to the need.
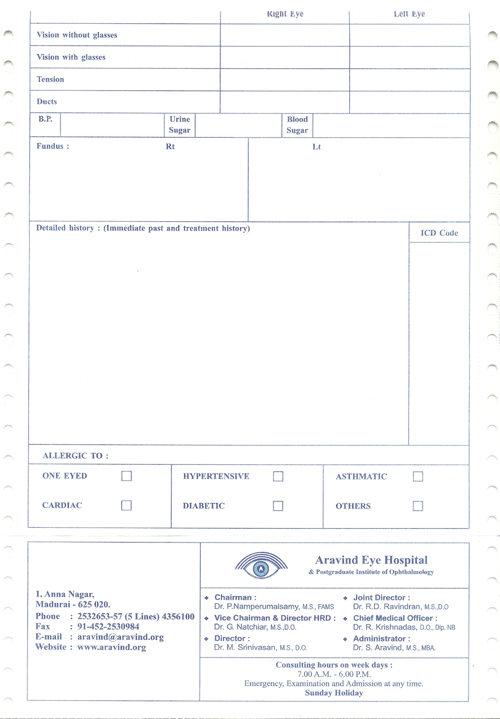
Identity card
The basic purpose of an identification card is to identify the patient and his medical record by number. When registering a new patient, a medical record number is given to the patient. This medical record number becomes the identification number of a patient. This card is also used as a receipt for the consulting fees collected during the first registration. This card is given to patient as an identity for subsequent visits to the hospital (Fig.4.3).

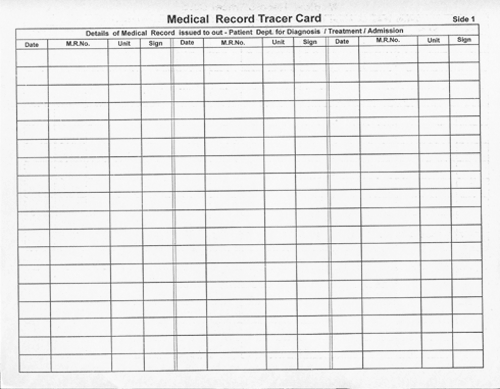
Tracer card
The name “Tracer Card” itself implies that when ever a medical record is not found in its place, the tracer card is the only source of information to the medical records assistant to track the exact location of the medical record taken. The tracer card contains three columns (Fig.4.4). The first column denotes the date, second column denotes the number of the record and third column denotes the signature of the retriever.
Tracer card can be used in different colors to differentiate between records retrieved for patient visit and, records retrieved for study or research purpose. After the medical record is replaced in its original location, Tracer card can be pulled out.
In-patient admission record
The Inpatient or admission record also known as the face sheet, is usually the top or first form of the medical record. The upper portion contains information of an identifying nature, while the lower section contains the admission information and the pre-operative instructions to be carried out for the inpatient. The information contained in the identification portion of the face sheet may vary in different hospitals. However, it should include enough information so that the patient can be positively identified.
This would include full name of the patient, address, phone number, place age, sex, marital status, and the name and address of the relative with phone number for emergency contact. Proper ICD code should be recorded by the doctors in the space provided for the purpose after finalising the diagnosis of the inpatient (Fig.4.5).
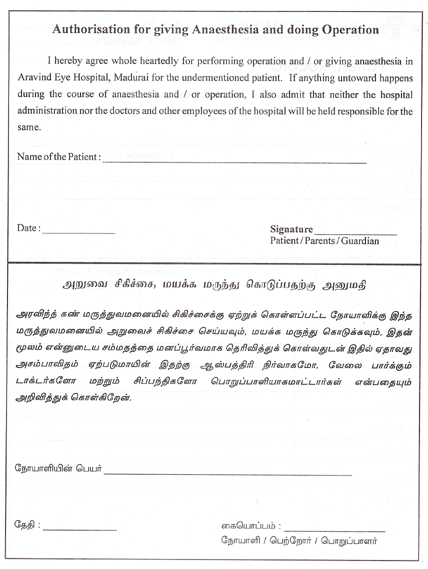
Consent form for surgical / medical procedures
The back of the admission record or face sheet is often used for the admission consent form (Fig.4.6) which is signed upon during the patient’s admission to the hospital as part of the admission procedure. This provides a record of consent to routine services, diagnostic procedures, and medical or surgical treatment.
The admitting assistant must inform the patient specifically that he is being asked to sign a consent form and the need for the form should be explained to him. Special consent for specific medical or surgical treatment are also required. But, in a single speciality hospital, the routine consent can be merged with the operation consent which can be also collected during the admission of the patient. It is also advisable that such forms should be countersigned by the relatives of the patient as a witness to the signing of the patient.
Speciality surgery record
Speciality surgery records are attached along with the other in-patient records according to the speciality department to which the patient gets admitted. For example:
- Retina surgery Record
- Cataract / IOL surgery Record
- Pediatric ophthalmology Intra operative Record
- Strabismus Surgery Record
- Glaucoma Surgery Record
- Orbit and Oculoplasty Surgery Record
- General Anesthesia Record
Color coding of record folders
Color coding refers to the use of color on folders to aid in the prevention of misfiling and in the location of misfiled records. Color bars in various positions around the edges of folders (known as blocking) create distinct patterns of color in various sections of the file. A break in the color pattern in a file section signals a misfiled record.
Color coding is most effective when used in conjunction with terminal digit and middle digit filing, although it is said that workable color-coding systems can be used for straight numerical filing.
Color folders
Based on the type of speciality department the color folders are also attached as a folder cover with the case sheet. This folders are in different colours. For example:
- Retina Folder (Light Blue)
- Cornea (Light Green)
- Cataract & IOL (Yellow)
- Orbit (Thick Green)
- Pediatric (Thick Reddish Brown)
- Uvea (Light Biscuit Brown)
- Glaucoma (Pink)
- General (Grey)
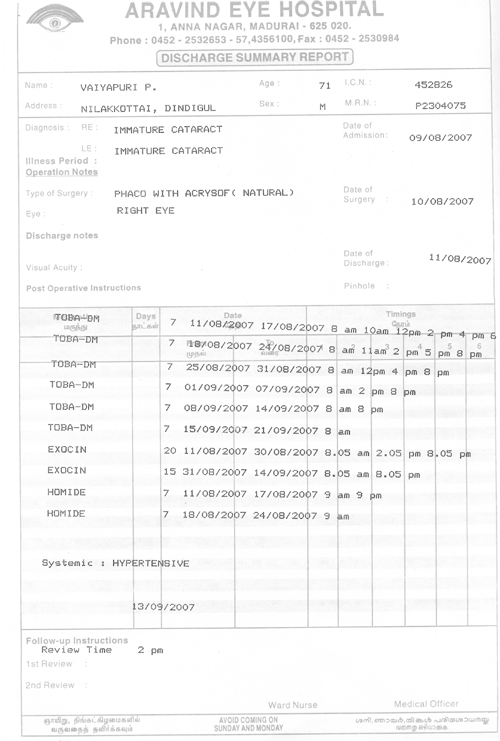
Discharge summary sheet
When patients are discharged, discharge summary (Fig.4.7) is given along with the final receipt. The discharge summary is a concise recapitulation of the reasons for hospitalisation, significant findings, procedures performed, course of hospitalisation, and condition of patient on discharge, and instructions given to the patient or family relating to physical activity, medications, diet, and follow-up care. The discharge summary sheet varies by colors and information according to the speciality. The following summary sheets are given as samples used against the speciality mentioned below:
- Cataract/IOL discharge summary sheet
- Retina summary Book
- Paediatric Cataract summary Book
Summary
A medical record must be maintained on every person who has been admitted to the hospital as an inpatient, outpatient or as an emergency patient. The medical record documents the medical and surgical history of the patient. Each hospital has the responsibility to develop medical record forms to fit its needs. Responsibility for designing medical record forms is delegated to the hospital forms committee. Although a variety of styles of medical record forms are used in hospitals throughout the country, certain basic essentials must be included if the hospital is to maintain accreditation standards. Medical record forms will not by themselves guarantee accurate and adequate medical records. However, if forms provide for the recording of essential data, and if the physician carefully records the information requested, accurate and adequate medical records will result.
Key points to remember
- A medical record must be maintained on all the patients who have been admitted in the hospital either as an Inpatient, as an emergency patient or visit the hospital as an out patient.
- In the development of a new form, it is advisable to have only a small supply of forms prepared for trial use.
- All discontinued forms should be removed from the stockroom or supply area and destroyed.
- Remember that standard–size forms are always less expensive, facilitate filing preclude loss, which is often the case with irregular paper sizes.
- When feasible, using a rubber stamp on an existing form can eliminate the need for special form that is not used regularly.
- Since cost is also a factor in continually revising and printing small quantities of forms, photocopying might be the reproduction method of choice.
Students Exercise
Answer the following
- Explain the four purposes for maintaining Outpatient Records in a hospital?
- Summarize the information contents of each of the following medical record forms:
- Information card.
- Consent form for surgical / medical procedures.
- Surgery record.
- Discharge summary book.
- State the first and most important step in designing a standard forms.
- Explain the basic principles in the development of good medical record forms.
