Counselling in Retina Clinic
Anatomy of retina
It is the innermost layer of the eye. The light impulses that fall on the retina are transmitted to the brain, which interprets the image. The central part of the retina is called macula which is essential for good central vision (Fig. 5.1).

Common diseases of retina
- Diabetic retinopathy
- Retinal detachment
- Age related macular degeneration
- Retinitis pigmentosa
Diabetic Retinopathy
Diabetic mellitus
Diabetes mellitus is a systemic disease in which there is a high blood glucose level. There are two types:
- Types I – Insulin dependent diabetic mellitus
- Types II – Non insulin dependent diabetic mellitus
Type II DM is the most common disease
The contributing factors are
- Inappropriate diet – high fatty diet
- Lack of exercise
- Obesity
- Heredity
Diabetic retinopathy introduction
Regardless of the type of diabetes, many diabetics develop retinal disease called diabetic retinopathy. The tiny, delicate retinal blood vessels become weak and start leaking. This causes structural changes in the retina and leads to loss of vision
Diabetic retinopathy is symptomless in the early stages. It is gradual in onset and is related to the duration of diabetes. Uncontrolled blood glucose levels, high blood pressure and high cholesterol levels influence the progression of diabetic retinopathy. Since only an ophthalmologist can detect early signs of diabetic retinopathy, all diabetics should have their eyes examined at least once every year. There are two main stages of diabetic retinopathy.
Non proliferative diabetic retinopathy
In this stage there are no new vessels in the retina. The blood vessels may leak causing swelling of macula thereby reducing vision.
Proliferative diabetic retinopathy
When new and weak blood vessels grow, they bleed into the vitreous causing vitreous haemorrhage. This can result in sudden and severe visual loss. In advanced stages, the vitreous may form a band and pull the retina off its place causing retinal detachment.
Investigation
Fundus Fluorescein Angiography
Role of counsellor in FFA
- The counsellor makes the patient aware of the need for investigation and its features:
- This investigation is done to find the location of involvement and the severity of the disease.
- The test is done with a dye called fluorescein which is injected into the vein and the retina is photographed with a special camera when the dye passes through the blood vessels in the retina.
- The test has to be done on an empty stomach or at least 3 hours after the last meal.
- FFA is only an investigation. It does not cure the disease. The doctor will decide on treatment after seeing the FFA report.
- The counsellor also makes sure the patient does not have any systemic problems like asthma, kidney problems or cardiac illness which may require physician’s opinion prior to the test.
- The counsellor tells the patients that if they experience any discomfort (including nausea or difficulty in breathing) during or after the procedure, they should report it to the doctor or nurse. Immediate treatment for allergy to the drug may be needed rarely.
Treatment
Medical treatment
Strict control of diabetes is a must to stop the progression of diabetic retinopathy. High blood pressure and cholesterol should also be controlled. Periodic check up with physician and ophthalmologist is mandatory.
Laser treatment
Lasers are formed by an intense and highly energetic beam of light. They can slow down or stop the progression of diabetic retinopathy and stabilise vision.
Laser treatment is usually performed as an outpatient procedure. The patient is given topical anaesthesia to prevent any discomfort.
Role of counsellor
- The counsellor explains the nature of the disease and the need for laser treatment
- She should be able to make the patient comfortable about the procedure by telling its features:
- The laser is an intense beam of light which will be used to treat the disease. It is not harmful to the eye and is the only mode of treatment for the current problem
- It is a completely painless procedure which can be done with topical anesthesia
- It may have to be repeated in another sitting or after some months depending upon the response of the disease to treatment
- The counsellor also makes it clear that the laser will only prevent further loss of vision and will not improve vision
Surgical treatment
In some patients with advance stage of diabetic retinopathy (like vitreous haemorrhage or retinal detachment) surgery may be needed to treat the disease.
Role of counsellor in explaining surgery
- The counsellor should tell the patient that the disease is at an advanced stage and will require surgery.
- She should tell the patient that if surgery is done at this stage then there may still be further progression of the disease and loss of vision. At the end visual recovery may not be possible.
Role of counsellor in diabetic retinopathy
- The counsellor should tell the diabetic patient the characteristics of the disease:
- Diabetes is a chronic disease which can affect various parts of the body including the eye.
- The duration of diabetes is more important than the level of blood sugar in causing retinopathy
- Even if you are in regular control of your blood sugar, diabetes will still affect your eye. But strict control of blood sugar postpones the onset of diabetic retinopathy and controls its progression.
- Diabetic retinopathy can affect your eyes without any symptoms and can only be detected by a careful dilated fundus examination by an ophthalmologist.
- The vision lost due to diabetic retinopathy cannot be regained. Any treatment done is only to prevent further loss of vision.
- The counsellor must convince the patient about the importance of regular follow up and treatment in each of the following situations:
CASE I
A recently diagnosed, young diabetic patient who has not yet developed diabetic retinopathy.
The counsellor
- Must explain to the patient that duration of diabeties influences the development of diabetic retinopathy and hence forth the patient should have regular eye check up (atleast once in a year).
- Must emphasise the need for strict diabetic control, because poor glucose control and long duration of diabetes will lead to early development and faster progression of diabetic retinopathy.
- Should also advise the patient to have regular check up with the physician so that he/she may not develop kidney problems. Other additional problems like high blood pressure, high cholesterol should be diagnosed and treated adequately.
CASE II
40 years old patient with history of diabetes for the past 6 years, diagnosed to have diabetic retinopathy
The counsellor in this case
- Must emphasise the need for strict control of diabetes
- Must tell the patient about the other problems like high blood pressure, cholesterol, anemia which can cause further retinal damage and hence emphasise the need for regular check up with the physician.
- Should counsel the patient regarding the various investigation and treatment modalities like FFA, laser treatment and how it would help in preventing further progression.
- Must be able to eliminate the patients fears about laser treatment and make the patient accept treatment and the follow up.
CASE III
An elderly patient with advanced diabetic retinopathy.
The counsellor
- Should be able to explain the various treatment modalities like laser, surgery
- Should convey the need for saving the residual vision and preventing blindness
- Must explain the need for maintaining strict blood sugar control, normal BP, normal cholesterol levels, so that further retinal damage can be prevented
- Must convince the patient about the need for frequent follow ups with the physician and the ophthalmologist
- The patient should feel comfortable and develop a positive attitude towards the treatment. This would ensure the patients’ compliance with the treatment.
The counsellor must be able to convince the patient regarding
- Regular and repeated follow up with the ophthalmologist at intervals determined by the doctor
- Regular follow up with the physician to control diabetes and associated systemic problems
- Self monitoring of blood sugar levels and maintaining strict diabetic control
Retinal detachment
Introduction
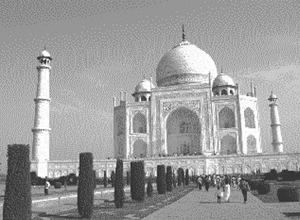
It is a condition in which the retina gets separated from its place. It can cause sudden and painless drastic loss of vision. It can be of different types and due to various causes (Fig. 5.2).
Symptoms of Retinal Detachment: (RD)
1. Flashes of light
Patient can see flashes of light especially during eye movement, blinking, this is due to pull on the detached retina.
2. Floaters
Small black spots, cobweb-like or large black rings may be seen by the patient.
3. Visual field defect
It is perceived by the patient as a black curtain before his eye.
4. Sudden loss of vision
This can be due to retinal detachment involving the macula.
The prognosis is very poor if the macula is involved.



Treatment
Treatment of RD is essentially surgical and should be done immediately once diagnosed.
Surgery
Surgery for retinal detachment involves three major steps.
Scleral buckling
A band or sponge made of silicone material is sutured firmly to the sclera to close the hole in the retina.
Vitrectomy
Removal of the vitreous humour is done to relieve bands which may pull the retina and to enable the surgeon to repair the retina.
Silicone oil injection or C3F8 gas injection
After vitrectomy the empty vitreous cavity has to be filled with silicone oil or with C3F8 gas. Patient must undergo another surgery for removal of silicon oil after 3-4months. Only after silicone oil removal patient can see better.
If the silicone oil is not removed with in 3-4 months, patient can develop cataract, and or glaucoma and may occasionally experience double vision.
In case of C3F8, there is no need for removal as it is a gas, hence a second surgery is not needed. The gas gets absorbed over 1½ months. During this period, patient might experience floaters, seeing bubble etc, which will gradually resolve. The patient must be explained to avoid air travel.
Role of counsellor in advising surgery
- The counsellor should emphasize the need for early treatment because the visual prognosis following retinal detachment surgery is very good if the surgery is done immediately and if the macula is not involved.
- A guarded prognosis should always be given in RD surgery as the outcome may be unpredictable.
- The need to maintain bed rest and correct sleeping position after surgery needs to be emphasised to the patient.
- The counsellor should inform the patient of poor prognosis if there is delay in surgery or the outcome if surgery is not done.
- The patient should be told that they will require a second surgery to remove silicone oil if it is injected in the eye. Silicone oil itself may cause cataract which will require surgery for cataract extraction and IOL implantation.
- He/she should alert the patient regarding the early symptoms of retinal detachment and the possibility that it may occur in the other eye.
Age Related Macular Degeneration (ARMD)
ARMD is a condition is which there is progressive loss or decrease in the quality of central vision. It usually affects elderly people.
There are two types of ARMD
1. Dry ARMD
This is the most common type. There is progressive and gradual decline in vision. There is no ideal treatment for ARMD.
2. Wet ARMD
This is less common but causes more severe loss of vision than dry ARMD. New vessels form beneath the retina called choroidal neovascular membrane (CNVM) and may bleed causing vision loss.
Symptoms
- Loss of central vision
- Seeing black spot in the centre of their visual field
- Distortion of images
Treatment
Dry ARMD: As of now, there is no treatment for dry ARMD but regular follow-up is needed to see if the disease becomes worse or converts to the wet type.
Wet ARMD : Laser treatment can be done to prevent further damage to the retina and progression of vision loss. There are also many new treatment modalities which are being tried to treat the disease.
Role of counsellor
- The counsellor should explain the poor prognosis and progressive nature of the disease. The patient should realise that though there is no treatment at present for dry ARMD he needs regular follow-up to see the progression of the disease.
- Cases of wet ARMD which can be treated should be counseled to undergo treatment to prevent further loss of vision. The patient should understand that the vision lost due to the disease cannot be recovered by laser.
- For patients who are blinded by ARMD, the counsellor should advise visual rehabilitation (ref. low vision counselling)
Retinitis pigmentosa
Retinitis pigmentosa is a heriditary disease, characterized by night blindness and constricted visual fields.
Symptoms
- Difficulty in seeing in dim light
- Constriction of visual fields i.e., Loss of peripheral field of vision and eventually tubular vision
Treatment
There is no treatment for RP as of now. The patient can be explained about low vision aids and life style modifications.
Role of counsellor
- The counsellor should sympathise with the patient about the lack of any treatment for this disease
- Should advice about visual rehabilitation like low vision aids
E.g : Use of bright torch while going outdoors in the evening. Working in good illumination - Should also advise the patient some life style modification e.g. avoiding driving and choosing an occupation which they can perform with the prevailing vision.
- Genetic counselling
- The counsellor must also inform the patient about the hereditary nature of the disease, and possibility of a similar problem in his/her siblings and children.
- The counsellor must convey to the patient about the increased chance of his/her children developing the disease, if he/she has a consanguineous marriage.
Frequently asked questions
1. I am 35 years old, the doctor told me that I have diabetes and mild retinal changes due to diabetes, can I completely cure myself?
Adequate control will help in preventing further damage to the retina. It may not completely reverse the existing damage. The retinal damage is directly related to the duration of diabetes therefore regular follow up and strict blood sugar control, is very important.
2. I am 77 year old. I have diabetes for the past 3 months. Will it affect my eyes?
Strict blood sugar control is a must. The patient should have regular follow up with the physician and ophthalmologist.
3. How should I prevent diabetic retinopathy?
Diabetic retinopathy is preventable with strict control of diabetes. Other systemic conditions like hypertension (high blood pressure) and high blood cholesterol must also be adequately controlled. Hence, regular check up with physician and ophthalmologist is mandatory.
4. If I undergo fundus fluorescein angiography (FFA) will I be able to see better or will I be cured of diabetic retinopathy?
FFA is an investigation. It helps to identify and confirm the retinal damage that has already occurred. It is not a treatment procedure.
5. Will I be able to regain complete vision after undergoing laser treatment?
Laser treatment for diabetic retinopathy helps in preventing the progression of diabetic retinal damage. Sometimes the vision may also improve to a slightly better level. If treatment is not done, there is a high chance of losing the existing vision.
6. Do I have to undergo laser treatment repeatedly?
Depending on the response to the first laser treatment the doctor will decide about repeating the laser treatment. Secondly, if this retinal problem recurs again, repeat laser may be required.
7. Are there any side effects of laser treatment?
No. Laser treatment is a very safe procedure. It can be done in the outpatient department itself.
8. Will I experience pain during laser treatment?
No. Laser treatment is done under topical anesthesia. Occasionally, few patients may experience mild pain which lasts for 3-4 hours. This can be relieved with eye drops to decrease the pain.
9. Can I bathe, and go for work, following laser treatment?
Yes. You can perform all day to day activities.
10. My spectacle power is -8D. The doctor told me that there is retinal hole and I have to undergo laser treatment? It is necessary?
Yes. Laser treatment helps in closing the hole. It prevents the formation of Retinal Detachment.
11. Do I have to come for check up regularly if I undergo laser treatment?
Yes. The patient should have regular check up at least once in a year to detect formation of any hole/tear/thinning/retinal detachment and undergo treatment.
12. I have advised to have an injection inside my eye. Where will they inject? Will I have any problem because of that?
Intra-vitreal injections are given inside the eye through the white of the eye. It is done under local topical anesthesia; the patient will not experience pain and will be comfortable during the procedure.
13. Will my vision improve after intra vitreal injection?
1. Intra-vitreal injection is done mainly to prevent any further damage to the retina.
2. Sometimes, it also helps in improving the present vision.
14. Following RD surgery, Will I regain my vision fully?
If the retinal detachment was present for long duration or if the centre of retina has been involved, complete visual recovery cannot be guaranteed. But, there is a chance of improvement of vision gradually.
15. Will I have any adverse effect because of silicone oil in my eye?
In the presence of silicone oil, few patients might experience double vision. The vision improves after silicone oil removal after 3-4months.
16. What will happen if silicone oil is left as such in the eye?
There is high chance of cataract formation. The eye pressure can increase leading to nerve damage and pain.
17. Can I have gas injection only? I do not want silicone oil injection because, I have to undergo resurgery to remove it?
The decision to use silicone oil or gas injection is made by the surgeon during the surgery based on the retinal status.
18. If I do not undergo surgery, will I have any problem?
Yes. The retinal detachment will progress. You may lose your vision completely, because of the retinal detachment. You can also develop cataract. You may also experience pain due to uveitis or glaucoma. Eventually the eye might shrink (Phthisis bulbi)
Key points to remember
- Diabetic retinopathy is caused by chronic diabetes and manifests as diabetic retinopathy. Minor changes will not be symptomatic so it is essential to come for yearly review in order to prevent blindness due to diabetic retinopathy.
- Retinal detachment is separation of retina from its place and treatment is surgical.
- Retinitis Pigmentosa is a genetic condition, patient will benefit with low vision aids, and genetic counselling is required.
- ARMD is a progressive degenerative condition occurring in elderly associated with poor visual prognosis. It is of two types dry & wet – former requires no treatment, but needs regular follow-up to judge its progression, and latter require laser treatment to prevent further loss of vision.
Student exercise
I. Write short answers
- List out the risk factors of diabetic retinopathy.
- What is the difference between counselling a patient aged 40 years and 60 years diagnosed with diabetic retinopathy and their vision recorded 6/6?
- Write down the importance of follow-up of diabetic retinopathy patient.
- How to counsel the patient with ARMD?
- What is the role of counsellor in counselling a RP patient?
- The patient with diabetic retinopathy had undergone three sittings of laser treatment, how will you encourage the patient to come for next sitting for laser by counselling?
