Counselling in Orbit Clinic
Orbit, Oculoplasty and Oncology includes disorders and diseases of all the structures surrounding the eye. The disorders are varied and so are the manifestations. These disorders may be infective, inflammatory, traumatic, developmental, neoplastic or age related.
Types of diseases
Lacrimal Drainage Disorders
Lacrimal drainage disorders include conditions like obstruction of the tear drainage passage, which may occur in children or adults, and inflammation of the lacrimal sac, which includes acute and chronic dacryocystitis (Fig. 9.1).

Symptoms
The main symptom of obstruction anywhere along the lacrimal passage is watering from the eye. There may be associated infection and discharge (mucous or pus) as in chronic dacryocystitis. Acute infections (acute dacryocystitis) are accompanied by severe pain and swelling in the lacrimal sac area (Fig. 9.2).

Investigations
- Syringing
- Complete hemogram including blood grouping and typing, bleeding time and clotting time
- Blood pressure
- Blood sugar
- HIV testing
Treatment
The treatment depends on the condition
- Acute dacryocystitis: Systemic painkillers and anti-inflammatory drugs with systemic and local antibiotics are given to control the pain and infection. If lacrimal abscess forms, the pus may have to be surgically cleaned out (incision and drainage).After the pain and swelling resolves, the patient usually requires surgery like DCR or DCT.
- Chronic dacryocystitis: The treatment consists of sac surgery, namely, Dacryocystorhinostomy (DCR) or Dacryocystectomy (DCT).
DCR
The sac is incised and passage for tear flow into the nose is created by removing a part of the bone. In adults it is usually done under local anesthesia. DCR may be done from the outside (between the eye and the side of the nose) or from within the nasal cavity.
Role of the counsellor in adults requiring sac surgeries
The counsellor should explain to the patient that the lacrimal sac is infected and needs to be treated surgically. In most patients, DCR is done, and a new passage for flow of tears is created. In old and unfit patients, or if there is a corneal ulcer or a mature cataract, the sac is simply removed (DCT). The patient usually does not have any watering after DCR but in some cases it may persist after DCT as the infected sac is removed and no alternative passage is created for tear flow.
Congenital naso-lacrimal duct obstruction
The initial treatment consists of Criggler lacrimal massage supplemented with antibiotic eye-drops. In most children, the passage opens up with proper Criggler massage. If it does not, probing is done. If the first probing fails, it may be repeated once after observing (with massage and antibiotics) for a few months (usually 6 months). If the second probing also fails, surgery (DCR) is done, usually after the child is 3 – 4 years old.
Probing
Probing is a very safe and simple procedure wherein a thin metal rod is used to try and open up the lacrimal passage by removing the obstruction. This is done under general anesthesia with full aseptic precautions, after the baby is at least 6 – 9 months old. In most children the obstruction is caused by soft tissue which can be opened up with the probe. However, it may also be caused by bone, in which case the probe will not be able to push through it and surgery will be required later.
Role of the counsellor in congenital naso lacrimal duct obstruction
The counsellor should explain to the child’s parents that obstruction of the naso-lacrimal duct is not a major problem. It does not harm the child’s vision at all, and in most cases it resolves with Criggler lacrimal massage by the end of the 1st year. The proper method of massage should be patiently demonstrated.
If probing has been advised, the counsellor should explain that it is not a surgery but a very simple procedure in which the doctor uses a fine rod to open the tear-flow passage. It is done under general anaesthesia. If the obstruction is minor or soft it can be easily opened up. If it does not open up, the procedure can be repeated after 6 months. Meanwhile massage over the lacrimal sac area should be continued.
Frequently asked questions
1. What is the cause for the watering and discharge?
Watering is caused by flow of tears being obstructed somewhere along the passage. The discharge is because of infection in the sac.
2. How can it be treated?
The only way to treat it is by surgically opening up the sac.
3. Is surgery necessary?
Yes, surgery is essential and will have to be done sooner or later. However, if any other intraocular surgery like cataract or retina surgery is planned, the sac surgery has to be done first as soon as possible.
4. What happens if we don’t treat it?
If left untreated, watering and discharge will persist. Also, it can precipitate infections and there is a chance of repeated episodes of pain and swelling near the eye.
5. Which is better: external or laser DCR?
Both have their advantages and disadvantages. External DCR takes longer time and involves sutures and a visible scar. Also, a pack is placed inside the nose for a day or so, which might cause some discomfort. In laser DCR the surgery time is only a few minutes and there is no scar or sutures or external wound, and no pack is left in the nose. It is done under topical anaesthesia, whereas an injection or GA is required for external DCR. However, laser DCR is a relatively new method and the results are not really very good, therefore, there is a chance that resurgery may be required. The results of external DCR are very good.
6. Does the tube placed during DCR cause any side effects?
The tube is made of safe material and does not cause irritation or any other side effects.
7. When should the sutures/tube be removed?
The sutures are removed after a week or 10 days, and the tube is left in place for a few months as advised by the doctor. Normally, it is removed after 3 to 6 months.
8. Will there be a scar?
Yes, external DCR does result in a small scar by the side of the nose. However, this usually fades with time and is not very noticeable after the wound has healed.
9. Is probing a surgery or a procedure?
Probing is not an operation but a small procedure wherein the doctor passes a thin rod into the lacrimal passage and tries to open it up. It only takes a few minutes and the child can go back home the same day. But GA has to be given.
10. Is there any risk to the child during GA?
Although some degree of risk is always there for every procedure, probing requires only short GA and the anesthetist will be present with the child throughout the procedure. The child will be well looked after and there is no cause for concern.
11. Probing was already done once. Why is it being repeated?
As probing is only an attempt to open up the passage which is congenitally blocked there is no guarantee that it will succeed in the first try. If the block is a soft tissue, it can be easily opened up, but sometimes the passage is blocked by hard tissue or even bone. In such cases the blocking tissue can be loosened or softened with one probing and then it may be removed with the second attempt. In case the block is caused by bone it can only be opened up by surgery later (DCR).
Lid Malpositions
‘Lid malpositions’ means abnormal position of the eyelid which include ptosis, entropion and ectropion.
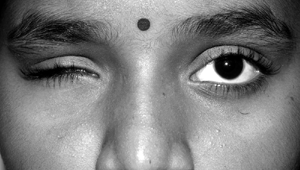
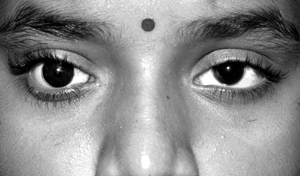
Ptosis means drooping of the upper lid. It may be congenital (present at birth) or acquired (develops later). Surgery is the only treatment for this condition. When the lid margin turns inwards, it is known as entropion, and when it turns outwards it is known as ectropion.
Role of counsellor
Parents of young children with drooping lids which are covering the pupil should be informed that if surgery is not done soon, vision in the affected eye may decrease. The lid can be lifted up surgically but this by itself does not restore any vision which may have been lost due to amblyopia. The operated eye will more or less look like the normal eye but may not be a perfect match.
Frequently asked questions
1. What is the cause of ptosis?
The exact cause of ptosis in children is not known. It is some developmental abnormality which occurs before the child is born. In old people it may be caused by loosening of the skin and tissues around the eyes. At any age it may be caused by some injury to the eye.
2. What is the treatment of ptosis?
Ptosis can only be cured by surgery.
3. Is surgery urgently required?
In small children if the central black part of the eye is covered by the eyelid, surgery should be done as soon as possible to avoid risk of amblyopia. In other patients, it can be done whenever the patient wants. In case the patient also has cataract which requires surgery, ptosis surgery is done after cataract surgery.
4. Will the operated lid absolutely match the other lid following surgery?
The operated eye will more or less match the other eye in appearance, but may not be an exact copy. Initially the movements of the operated eyelid will not match the other one, but this will improve with time.
5. Is it a major or minor procedure?
Ptosis surgery is a minor procedure wherein the drooping lid is lifted up. The eye is not touched during the operation.
6. Can both eyes be operated at the same time?
Yes.
7. Post operatively – the child’s eye remains partially open especially at night. Will it cause damage to the eye? Is it permanent? What is the cause?
Because the lid has to be shortened to lift it up, the eye remains open at night especially just after the surgery. Damage to the eye can be prevented by using the prescribed ointment at night. It gradually improves with time.
8. Can the lid droop again following surgery?
Yes, sometimes the shortened tissue may become loose again in which case it can simply be tightened again in a small procedure.
9. How soon after surgery can the patient resume normal activities?
As soon as the swelling subsides the patient can start normal activities like reading and watching TV. However it is better not to send the child to school till the sutures are removed, which may take about 2 weeks.
10. Can the patient read/watch TV after surgery?
Yes, there is no harm in that, but the patient should not strain the eyes or rub the eyes.
Orbital Tumours
Orbit is a pyramidal bony cavity in the skull about 2 inches deep that provides protection to the entire eyeball except the front surface. It houses the eyeball, its muscles, blood supply, nerve supply, and fat.
An abnormal, uncontrolled growth of cells in any body tissue results in a mass of cells, this is called a tumour. Tumours when present in the orbit are called orbital tumours. They may develop from the orbital structures or may also invade the orbit from the sinuses, brain, or nasal cavity which surrounds the orbit. It may also spread (metastasize) from other areas of the body. Orbital tumors can affect adults and children. Tumours may be benign or malignant. Fortunately, most are benign.
Benign Tumour: A tumour made of normally functioning cells which maintain tissue boundaries is called benign. Their treatment is simple and usually curative (Fig. 9.3).

Malignant tumour: A malignant tumour or cancer is one which is made of cells that have the potential to invade & destroy surrounding structures. Cancer cells can spread to other body parts and start new tumours there. Their treatment is dependent on the size and stage of proliferation and is generally multi dimensional and may not be curative (Fig. 9.4).

Symptoms
The common presenting symptoms of an orbital tumour include
- Protrusion of the eyeball (proptosis)
- Pain
- Loss of vision
- Double vision
- Redness
- Swelling of the eyelids
- An obvious mass
If tumour spreads from surrounding structures then there may be headache, nose discharge, breathing difficulty, swelling in the surrounding tissues before involvement of the eye.
In children, parents may first notice a droopy eyelid or slight protrusion of the eye.
Investigations
Orbital tumours are most frequently diagnosed with an ultrasound, a CT scan or MRI. If one or more of these tests look suspicious, a biopsy may be performed before removal of the tumour in toto. Supplementary blood tests and other invasive tests like lumbar puncture and bone marrow testing may also be required.
Biopsy is the procedure of removing a part of the tumour and testing it to know whether it is benign or cancerous. Such tests require a few days’ time because the sample has to be processed and stained, sometimes with various special stains to reach at a final diagnosis before planning for further treatment.
Treatment
Treatment of orbital tumors varies depending on the size, location, and type. Some orbital tumors require no treatment, while others are best treated medically or with the use of radiation therapy, or chemotherapy. Still others may need to be totally removed by either an orbital surgeon or a neurosurgeon, depending on the particular case. After removal, additional treatment such as radiation or chemotherapy may be required.
Enucleation: It is the surgical removal of the diseased or damaged eyeball. In this procedure the muscles outside the eyeball and the other orbital structures are left intact.
Exenteration: It is the surgical removal of the diseased eyeball along with the orbital structures. It is performed for tumours of the eyeball which have spread outside the eye or for recurrent tumours (eyes that had undergone prior surgical removal).
Chemotherapy: It is a part of cancer management. Medicines which are active against the cancer cells are called chemotherapeutic agents or anti-cancer drugs.
Side effects of chemotherapy
As anti-cancer drugs are effective against all rapidly dividing cells, they also kill normal body cells which are rapidly divining such as, hair follicle, lining cells of the bowel, immune cells etc. Therefore, they result in hair loss, bowel disturbances, frequent infections due to low resistance of the body to infective microbes.
These drugs are given in a cyclic fashion, repeated once in three weeks to allow time for the normal cells to regenerate.
Radiotherapy (RT)
It is a part of the armamentarium used to fight against cancer cells. Here high-energy rays such as X-rays, rays, neutrons, and other sources are used to kill cancer cells and reduce the tumour. Such radiation may come from an outside source (External beam RT) or the source may be placed close to the tumour (Brachytherapy).
It is usually given over a period of time divided into equal doses, to reduce the side effects and damage to the normal tissues.
Side effects of radiotherapy
They are similar to chemotherapy, but radiotherapy mainly has local side effects. It causes skin changes, conjunctivitis, and dry eyes due to reduced tear secretion, cataract formation, and damage to retina or optic nerve (nerve of the eye).
Role of counsellor
The counsellor’s job, as far as a patient with a tumour is concerned, is very delicate, much more so in case of tumours in children. Her approach should combine compassion and firmness. She should convince the patient in a sympathetic manner that the treatment which has been adviced by the doctor is absolutely necessary. In case of tumours / suspected malignancy, the patient cannot afford to waste any time. However, she should understand that if destructive surgery has been advised, the family would probably be in shock and would need some time to accept this. It should be patiently explained that this is the only option available and is being done to prevent further harm to the patient. Removal of the eye means vision in that eye will not be restored by any other method. However, an artificial eye can be placed later which will at least provide the appearance of a normal eye. In case of tumours with familial occurrence (like retinoblastoma), the patients should be clearly instructed to bring the sibling for examination & genetic counselling should be done.
Frequently asked questions
1. Is removal of the eye necessary?
Removal of the eye is only adviced by the doctor when there is no way of saving it, or when the tumour in the eye poses a danger to the life of the patient. Therefore, if removal of the eye has been adviced, it is better to do so as early as possible.
2. Will surgical removal be the final treatment or will something further be required?
If the tumour has not spread much, removing the eye is enough. However, if the tumour has extended beyond 1 eye then further treatment like injections (chemotherapy) or application of high-energy rays (radiotherapy) will be required. The doctor will be able to tell definitely only after removing and examining the eye.
3. Is there any way of restoring vision after removal of the eye?
There is no way of restoring vision once the eye has been removed. However, we can fit an artificial eye later which will give the appearance of a normal eye.
4. When can the artificial eye be fitted?
It is usually fitted once the wound heals and the swelling subsides. This takes about 6 weeks.
5. Will removing one eye affect the other eye?
Removing one eye will not affect the other eye as such, but it will have to be carefully examined periodically to rule out the presence of a similar tumour. As the patient will have only one eye, it is better to come for a check up at least once a year, or soon if there is any symptom like discomfort or visual disturbance.
6. Can it recur after treatment?
Yes, there is a chance for recurrence of a tumour even after complete treatment. Because of this, the patient must come for regular follow-up as advised by the doctor.
7. Is there any danger to the other family members?
Especially in tumours of childhood (like retinoblastoma), all the siblings and even the parents should be examined.
8. What does radiotherapy and chemotherapy involve?
In radiotherapy, high-energy rays are applied to specific areas to destroy the tumour cells. In chemotherapy, specific medicines which target the tumour cells are injected intravenously. The patient will have to stay in the hospital for two to three days and then report as adviced by the doctor. Several doses of radiotherapy/ chemotherapy may be required. They also have several side effects like nausea and vomiting, loss of weight and severe hair loss, so much so that the patient may become totally bald. These periods of physical and mental stress should be supplemented by good moral support from the family members, as well as a healthy and nutritious diet. The family members should always present a cheerful face and a positive attitude to the patient, who may become very prone to dejection and depression during this time.
9. Why has the tumour occurred even though the parents are not even remotely related by blood?
A. Even though 90% of such tumours are caused by consanguinity or relation by blood, the cause of the other 10% is not clearly known. This tumour, unfortunately, may belong to that 10 %.
10. Our other child has two good eyes. How will this child accept to become one-eyed?
Children adapt very fast, especially if the adults around them behave as if everything is normal. Please understand that this diseased eye has to be removed before it causes harm to the child’s life. Do not ever let the child see you depressed about his being one-eyed, and do not speak of him as being less than normal. Once this tumour is taken care of, there is no reason why he should not lead a full, healthy life.
11. How frequently do we have to bring him for check-up here?
He will need checkup every 3 months till the age of 3 years, and every 6 months till the age of 6 years. Yearly checkup will suffice thereafter, till about the age of 15 years. The dates for follow up will be given to you at each visit; please ensure that you bring the child for follow up as advised.
12. Now that this child has this tumour, can we have another child? What are the chances of the other child also getting this same tumour?
We will have to ask the doctor. If you want, we can discuss this with him / her now. They might need to do some tests also like charting family tree and taking blood samples for genetic testing.
Ocular Prosthesis
Following removal of the eyeball (Fig. 9.5), (after enucleation or evisceration) or following shrinkage of a blind eye (phthisis bulbi) vision cannot be restored to that eye by any means. However, acceptable cosmesis can be restored by fitting an artificial eye (Fig. 9.5a).
Types of prosthesis
There are basically two types of prosthesis
- Stock eye or ready-made eye
- Custom-made prosthesis
Stock eye: This is the commonly available ‘plastic eye’. It costs less, is available in different sizes and colours, and provides a rough match for the normal eye..
Custom-made prosthesis: This is made to exactly match the normal eye in colour, shape and size. Scratches and mild damage can be repaired by polishing about once a year. The prosthesis lasts for about 10 years.
Role of counsellor
The counsellor should explain that the ocular prosthesis will only improve the person’s appearance but will not provide vision. The custom made prosthesis will match the other eye almost exactly. Some degree of movements will be there.
Frequently asked questions
1. How soon surgeries after surgery can the prosthesis can be fitted?
Prosthesis is usually fitted once the wound heals and the swelling subsides. This takes about 6 weeks.
2. Will it match the other eye?
The stock eye, which is ready-made, provides only a rough match for the other eye. But if the patient can stay for 2 days in the hospital we can prepare a custom-made prosthesis which will exactly match the other eye in appearance and shape. This also does not need to be replaced for a long time. However, it costs more than the stock eye.
3. Will it move like the other eye?
Although the plastic eye does not move exactly like the normal eye, some degree of movement will be there, especially with the custom - made eye.
4. Does it have to be removed while sleeping?
No, it does not have to be removed while sleeping.
5. Does it have to be cleaned?
Yes. The stock eye should be cleaned once in a week and the custom - made eye should be cleaned once in a month. Normal tap water can be used for cleaning both.
6. Does it have to be changed?
The stock eye needs to be replaced every year and the custom - made eye lasts for 10 years or even longer. It can be polished once a year to remove any scratches.
Key points to remember
Lacrimal drainage disorders
- Obstruction of lacrimal drainage system produces watering
- In adults, this obstruction is relieved by surgery (DCR/DCT)
- In DCR, the sac is removed and an alternative passage for tear flow is created.
- In DCT, the infected sac is removed
- Most cases of CNLDO resolve with lacrimal massage. If massage does not relieve the obstruction, probing is done. If 2 probing fails, DCR is done.
Ptosis
- Ptosis may affect one or both eyes and may be congenital or acquired
- If the pupil is covered by the lid, the vision may get damaged
- Ptosis surgery does not restore vision loss due to amblyopia (except in very young children)
- The treatment of ptosis is surgery
Tumour
- Any suspicious lesion should be investigated without delay
- In tumours with familiar occurrence, the importance of examining the siblings should be explained, even if their (the siblings) eyes are apparently normal.
- The counsellor should stress on the importance of coming for follow-up as adviced.
- The side effects of chemotheraphy/Radiotherapy should be clearly explained.
- The approach to the patient should be compassionate
Ocular prosthesis
- There are basically two types of prosthesis: Stock eye and customised prosthesis
- Customised prosthesis provides better cosmesis, lasts longer and requires less maintenance than the stock eye.
- Stock eye needs to be changed every year. The custom-made prosthesis needs to be polished once in a year and lasts for about 10years
Student exercise
I. Write short answers
- How will you counsel a patient who has been adviced DCR?
- What will you tell the parents of a child with severe ptosis in one eye?
- How will you convince the parents of patient with retinoblastoma to let the child undergo enucleation?
- How will you explain to the parents of a child why probing failed? How will you justify repeat probing?
- What will you explain to a patient who has been adviced chemotherapy?
