Counselling in a Paediatric Ophthalmology and Strabismus Clinic
It is a branch of ophthalmology concerned with eye diseases and vision care in children from birth until 15 years of age.
Types of Diseases
Refractive errors – causes, symptoms & treatment
It is a common eye problem. It is the second most common cause of preventable blindness. The symptoms may be missed as children are unaware of their problem. It is generally reported by the school teacher by observing the child’s behavior in the classroom (Fig 7.1).
4-5% of all children have some refractive error. Many children fail to have an ophthalmic consultation as parents may be ignorant of the problem or hesitant out of fear that glasses, if worn at a young age may become permanent.
Myopia
Definition
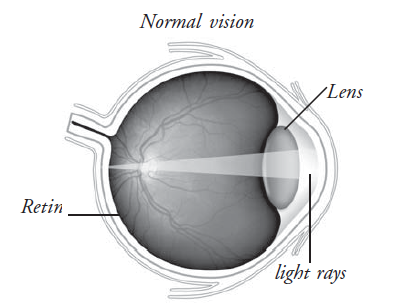
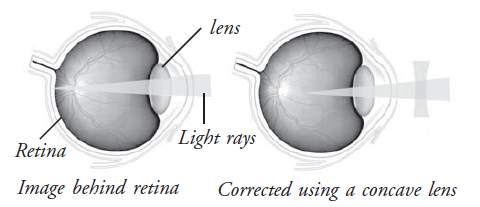
Normally, light entering the eye gets focused on the retina. When the light gets focused in front of the retina, it is called myopia. It is also called near sightedness (Fig 7.2).

Symptoms
- Child is unable to see letters on the blackboard
- Child keeps books very close to eyes while reading
- Child sits too close to the television
- Child squeezes eyes while trying to see distant objects
Treatment
- Use of spectacles (minus lenses)- to provide clear vision, thus enabling the child to see distant objects clearly
- Contact lens, can be used after the age of 15-16 years.
Hypermetropia
Definition
It is a condition where light entering the eyes come to a focus behind the retina. It is also known as far sightedness and is less common than myopia (Fig 7.3).
Symptoms
- Child has difficulty in reading, both at distance and near
- Eyestrain and headache while trying to read
- Squint
Treatment
- Use of spectacle (plus lenses) - to provide clear vision
- Contact lens- could be tried in some cases after the age of 15-16 years.
Astigmatism
Definition
It is an eye condition where the light entering the eye does not come to a point focus on retina. Some light rays get focused behind and some in front. Hence the person cannot see a sharp and clear image.
Symptoms
- Blurred vision for distance and / or near
- Squeezing of eyes while trying to see fine objects or letters
- Frequent headache
Treatment
- Use of glasses
- Contact lens
Role of counsellor
- Explain the parents about the visual defect (Myopia/ Hypermetropia/ Astigmatism in detail using an eye model.
- Encourage child to wear glasses regularly
- Explain that wearing glasses will improve child’s vision, and hence child’s concentration and academic performance too.
- Advise yearly checkup
- Advise maintenance of glasses (Cleaning & handling)
- Advise examination of family members (Specially in myopia)
- To report immediately if child has complaints of floaters, flashes or sudden diminution of vision
- Explain that refractive error will keep on changing, hence regular follow-up is necessary
- Explain that any kind of diet and medicines will not change the refractive error
- To request school teacher to ensure that child uses glasses regularly
- Encourage and motivate child and parents and tell them not to get discouraged by other’s comments.
The counsellor should spend adequate time with the child and family to emphasise and reinforce the importance of wearing glasses. She should modify her style of counselling, using visual aids and analogues to convince both the child and the parents.
Frequently Asked Questions
1. Should my child wear glasses all the time?
Yes, it is very important that your child wears glasses all the time, for constant clear vision except while sleeping or during sports like swimming. Contact lenses can be worn if child is old enough and interested in outdoor sports.
2. Will the power keep on increasing? Is it likely to decrease later on? What can be done to keep the power stable?
It is difficult to say exactly about the change of the glass power in the future. Due to constant growth of the eyeball, the power tends to change (usually increase), till about 18-20 years of age. Hence it is important that you come for a regular annual checkup. Nothing can be done to keep your glass power stable.
3. Did my child get refractive error because she sat too close to the T.V?
Watching TV does not affect the eye power. Infact, as distant vision was blurred your child had to sit close to the TV to see better.
4. Is there any eye exercise /diet that can cure this problem?
Good nutrition will definitely keep the eyes healthy, but there is no relation of diet to refractive error. People say that eye exercises improve vision but there is no scientific proof. It may help in doing away with low refractive errors.
5. How long should glasses be worn?
Generally glasses have to be worn life long.
6. Is there any surgical cure for this?
After the age of 20, when the glass power becomes stable a laser treatment called LASIK may be done, so that your child need not wear glasses.
7. How frequently should I come for a checkup?
An annual checkup is sufficient for most cases of refractive error.
8. Is this condition hereditary? Did the child get it because one of the parents wears spectacles?
Sometimes it can be hereditary. It is more likely to occur if one or both parents use high power glasses.
Amblyopia – causes, symptoms & treatment
Definition
It is a condition where the vision in one or both eye is reduced in the absence of any structural abnormality or diseases. It is also called “Lazy eye”.
Causes
- Squint
- Difference in the refractive error between the 2 eyes
- Any problem in the cornea and lens which prevent light from reaching the retina
- Complete ptosis (drooping of the upper eye lid)
- Very high refractive error (power) in both eyes
Treatment
Making the child use the amblyopic eye to improve the vision
This can be achieved by
- Use of spectacles if the child has a refractive error
- Removal of opacity in the visual axis (cornea, lens)
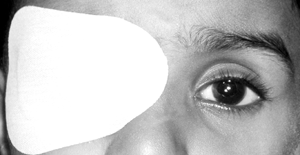
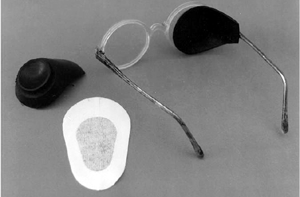
- Patching /occlusion therapy – patch the normal eye, thus forcing the child to use the lazy eye. (Fig 7.4 and 7.4a)
Role of the counsellor
- Explain to the parents the cause of amblyopia in their child
- Tell the parents the importance and proper method of patching
- Patching can be cumbersome and irritating for both the child and the parents. Hence the counsellor should emphasize the need for regular patching.
- She should explain to the parents that improvement in vision is a slow and gradual process, hence the need for long term occlusion therapy with good compliance and regular follow up.
- Explain the importance of regular follow up
- To see the response to patching
- To check the power change
- Ask the parents to inform the teacher or send a letter to the school teacher about the need for the child to patch the good eye.
- Tell the teacher to report the child’s performance
- Enquire performance of child during follow up and encourage the child to continue patching and using glasses during each follow up visit.
- Contact patients (by letter/telephone) who do not come for follow up.
- Some parents require to be cautioned against patching for a duration longer than prescribed as this may lead to conversion of the good eye into a ‘lazy eye’.
Frequently asked questions
1. Why has my child developed amblyopia though the eye seems to look normal?
Your child has a refractive error/ deviation of one eye. Hence she/he has only been using the good eye to see things. Therefore this eye has become lazy.
2. How long should I patch the eye?
The duration of patching would depend on her/his level of vision
- As the vision is very less (worse than 6/36) the good eye should be patched atleast 6 hours/day
- As the vision is slightly less (better than 6/36) the good eye must be patched 4 hrs/day. The child should do some near work like reading books, drawing or using coloured toys when the good eye is patched.
3. Child is not cooperative with patching .What can be done?
Patching is a very unpleasant thing, hence it is natural that the child would be uncooperative initially. But it is very essential that the good eye is patched as advised. It can be started by patching for a short time first and then gradually increasing the duration of patching. It needs to be emphasised to the parent that the vision in the poor eye is likely to improve only with the patching. The parent can be told that this is akin to exercising the bad eye and it is entirely the parent’s responsibility to ensure that this is done.
4. How frequently should the child be reviewed?
It should be according to the doctor’s advice: Babies should be reviewed more frequently (than older children). If patching is done for alternating squint then the follow-up is every 2 months, otherwise it is every 3-4 months. Older children can be reviewed once every 6 months. At every follow-up the vision is checked to see for any improvement. The duration can be gradually increased as the vision improves.
5. Till what time and age should patching be continued?
The critical period for development of amblyopia is first 8 years of life. Hence it will be more successful if started at a younger age. Patching is continued as long as vision is improving. Once the vision improves to the maximum possible level, patching is tapered gradually and then stopped. Patching is discontinued if vision does not improve in two to three 6 monthly visits. Patching is never stopped abruptly but always tapered. A patching trial can be given in older children, under a guarded prognosis, as the chances for visual improvement are less.
6. How should the eye be patched?
Readymade patches are available. Sticker like patches can be stuck over the eye directly. Patches made of cloth have to be stuck by a sticking tape. If the child is wearing glasses, the patch should be stuck over the eye and not over the glasses.
Cataract – causes, symptoms and treatment
Definition
Cataract is a condition where the lens of the eye becomes opaque and reduces the amount of light entering inside the eye, thus blurring vision. Normally the lens is transparent like a piece of glass. Generally it is a disease of old age but it can also occur at birth or in first few years of life. Incidence is 3 in 10,000 live births. It can involve one or both eyes (Fig 7.5 and Fig. 7.5a)


Causes
- Intrauterine infections
- Chromosomal disorders - there is abnormality of eyes and other body parts due to a problem in the genes
- Hereditary - If parents also had a cataract in childhood
- Metabolic disorder - due to absence of or abnormal presence of enzymes or chemicals which control different functions of the body. These are associated with disorder of other systems too.
- Trauma/injury to the eye.
- Idiopathic (causes not known)
Symptoms
Parents/grandparents may notice
- White spot in one or both eyes of the child
- Child does not look at toys/light
- Older children may complain of defective vision
Treatment
Early surgery is indicated to prevent amblyopia
- Removal of lens matter is done if cataract is present in both eyes and child is less than 2years of age
- Removal of the natural lens and placement of an IOL if cataract is unilateral (in one eye only) and if child is older than 2 year
Role of counsellor
The counsellor should explain
- What a cataract is and how it affects vision using eye model?
- Encourage early surgery
- Convince the parents that surgery is a safe procedure and the only treatment for cataract
- The importance of early cataract surgery
- To improve vision
- To prevent the development of lazy eye
- How the surgery will be done under general anaesthesia, convince the parents that the child will be unconscious and will have no pain during the surgery?
- If surgery will be done with or without IOL
- The different types of IOL and their advantages
- What drops or ointment should be used following surgery. Also demonstrate the proper method of instilling drops as well as the precautions to be taken like washing hands.
- Genetic counselling – if child has bilateral cataract
- Need for follow up
- To see if the eye is doing well
- To detect PCO (which may again cause amblyopia)
- To check vision and change in glass power
- The need to use glasses after surgery.
Frequently asked questions
1. Will the vision improve to 100% after doing the cataract surgery?
This will depend on the density/severity of the cataract and the age of child. If the cataract is not much and the child has been operated at an early age chances of improvement of vision are more provided the rest of the eye is normal.
2. Will the vision improve immediately after surgery?
This would depend on the cause of cataract, its density and age of the child at the time of surgery. Vision may not improve immediately. The child might have to use glasses and then patch the good eye to force him/her to use the operated eye. The child will have to be checked frequently as the power of eye, and thus the power of glasses keeps changing.
3. Is it safe to undergo surgery for cataract at a very young age or it is it better to wait?
Cataract surgery can be done as early as 6 weeks. It is safe provided the health of the child is good. It is done under general anesthesia where the patient is unconscious. There will of course be some risks associated with general anaesthesia just like any other surgery.
4. Why can’t an IOL be used in my child like the others?
There are certain situations where an IOL cannot be put in the eye like
- If the eye is too small
- There is cataract in both eyes and child is less than 2 years
- The eye has inflammation (uveitis) for a long time
- In children less than 2 years with bilateral cataract, cataract removal alone is done in the first sitting. This is so because the eye is small at birth and undergoes rapid increase in size during the first two years of life. Hence it is difficult to calculate the IOL power accurately. An IOL can be implanted at a later date once the growth of the eye stabilises.
The eye is inflammed (uveitis) for a long time- If there is inflammation inside the eye for a very long time; putting an IOL may further worsen the inflammation, as an IOL is a foreign body after all. This might cause further problems like increase of the pressure inside the eye and reduction in vision, which is difficult to control.
5. Is it necessary to use glasses after surgery?
All children have to use glasses after surgery. Following cataract surgery, if an IOL is not placed, the child will have to wear thick glasses. If an IOL is placed in the eye the child may still need to use glasses for near vision.
6. What should be done after the surgery?
Eye drops and eye ointment must be used for a minimum of one month as advised by the doctor. Child should not go to school or to play. The child should come back for a followup
Retinoblastoma – causes, symptoms & treatment
Definition
Retinoblastoma is a tumor /cancer of the retina. It occurs in children, generally less than 3 years of age. It is the commonest eye tumor in children. Incidence is 1 in 20,000.

Cause
The tumor is caused due to changes in a gene. This gene alteration (mutation) may develop in a child whose family has never had eye cancer, but sometimes several family members may have this gene change. It can affect one or both eyes. If not treated it spreads behind the eye to the nerve of the eye, brain and other body parts.
Symptoms
- Symptoms are generally detected by parents
- Vast majority present to the doctor by 2 years of age
- Children with bilateral tumor present earlier (by 1 age). However children can present upto 6 years of age
- White reflex of the pupil - this is the commonest symptom with which a child presents to an eye doctor
- Squint - the affected eye may be deviated in or out
- Redness - the eye may be red due to inflammation like condition within the eye
- Large eye - due to increase in the pressure of eye.
Investigations / Test
- Detailed ocular examination after dilating the pupil, and using special equipment. This may have to be done under a short general anaesthesia, to know the location and size of the cancer.
- Ultrasonography – Done to assess the tumor size and to see other specific features of the tumor (calcium deposits in the tumor.)
- CT scan / MRI– to see if the tumor has involved the nerve of the eye, areas outside the eye and the brain.
- Bone marrow aspiration and lumbar puncture- these tests are done to know if the tumor has spread to the rest of the body
Treatment
Depends on the size and location of tumor and to what extent it has spread beyond the eye.
- Photocoagulation – A laser is used to destroy the tumor
- Cryotherapy - Low temperatures are used to kill the cancer cells
- Chemotherapy – Various drugs are injected through a vein, given orally, or injected into the fluid surrounding the brain and spinal cord to slow down the growth or kill the cancer cells.
- Radiation therapy – X rays are used to kill the abnormal cells
Role of counsellor
- The counsellor should explain about the nature of the tumor in the child’s eye.
- Should explain that the tumor will increase in size and spread beyond the eye if not treated at the proper time. Should warn that it may appear in other eye.
- Should inform the parents at what stage the tumor is when the patient presents to the doctor.
- Counsellor should empathize with the family
- Should explain the need of enucleation (if advised by the doctor)
- Tell the importance and need of Radiotherapy and chemotherapy in cases where the tumor has spread beyond the eye.
- Genetic counselling is very important as the disease can be hereditary
- Counsellor should explain to the parents about the probability of other siblings having the same problem
- Stress on the need for regular follow-up
Frequently asked questions
1. Is it necessary to remove the entire eye having the tumor?
At this stage, the tumor is confined to the eye and has not spread beyond it. The affected eye also does not have any vision, so functionally it is not useful. It is not possible to remove only the tumor and preserve the globe. Hence it is essential to remove the eye to prevent the tumor from spreading outside.
2. How will the child look after removing the eye?
We can implant an artificial eye in place of the real eye, so that cosmetically it looks better. However, this prosthetic eye will not move as freely as the normal eye. Also there will be no vision in the prosthetic eye.
3. Will the tumor/ Cancer be completely cured after enucleation?
After enucleation the removed eye and its nerve will be examined by experts to see if the tumor has spread beyond the eyeball. If the tumor is confined to the eye, the chances of complete cure are high. However, you must come for repeated and regular examination for few years. If the tumor has spread beyond the eye then additional treatment in the form of radiotherapy or chemotherapy would be needed.The other eye can also be affected.
4. Until what age can a child develop retinoblastoma?
Most retinoblastoma are diagnosed before the age of 3 years. A child is not likely to develop the tumor after 7 years of age.
5. Will my 2nd child also develop similar tumor?
Since retinoblastoma could be hereditary an eye examination of the parents, history of an eye tumor and blood tests of the family members (for seeing the presence of the abnormal gene) is done. If a parent is determined to have the abnormal gene then the chances of 2nd child having retinoblastoma is 50%. If neither parent has the mutation, the chances come down to 3-5%.
Strabismus – causes, symptoms & treatment
Definition
Strabismus is defined as misalignment of eyes. It is caused by a lack of coordination between the two eyes. Hence the eyes look in different directions and do not focus on the same object (Fig 7.7).

Causes
- Hereditary
- Problems with the muscle or nerves that control eye movements
- Due to poor vision – Eg., Refractive error, cataract
- Injuries
Symptoms
- Eye are misaligned; one eye is turned out or in
- The misalignment may be constant or intermittent
- The eye may be turned in, out, up or down
- There may be associated shaky or wobbly movements of eyes
- The eyes may not move together
- Occasionally the child may complaint of double vision, if the squint occurs suddenly. Adults may complain of double vision if squint develops late in life.
Consequence of squint
- The vision in the deviated eye decreases. This is called amblyopia or lazy eye. It occurs because the brain ignores the image/information sent to it by the deviated eye.
- Since both eyes are not used together at the same time, the child loses the sense of depth perception
Treatment
Depends on the cause
- Use of correct spectacles - if the vision is low and child has a refractive error. Glasses alone may align the eyes in certain cases
- Treatment of the lazy eye - by using glasses and patching the good eye
- Cataract removal - if cataract is the cause
- Surgery - the eye muscle are weakened or strengthened to realign the eye
- A weak muscle is made stronger and a strong muscle is weakened. Some cases require shifting of the muscle to a new position
Role of counsellor
The counsellor should explain
- The cause of squint in the child
- How squint affects the vision, appearance and academic performance of the child
- The importance of patching and using glasses to improve vision, if there is amblyopia
- Tell the parents not to get discouraged by hearing other’s comments.
- Counsel about surgery
- Moderate the parents‘ expectations
- Surgery will only make the eyes straight but will not improve or decrease the vision.
- Compliance with followup visits is essential
- To check vision
- To detect change in glass power
- To dignose recurrence of squint
Frequently asked questions
1. Will the vision in the eye improve after surgery?
No, the surgery only realigns the eye. It does not affect the vision at all. Hence vision neither improves nor degrades after a squint surgery
2. Will there be need for a 2nd surgery? Will the eyes be perfectly aligned after the first surgery?
Our goal is always to obtain an excellent alignment of eyes. However the results would depend on the amount or extent of the deviation. Generally 80-90% cases have a satisfactory alignment. However there are chances that there may be some residual squint. There may also be some overcorrection. If the squint is very large or if it recurs after few years, a 2nd surgery may be required.
3. Can the squint surgery be done at a young age or should one wait till the child grows up?
It is better to do the surgery at an early age so that the eyes become straight and both eyes can be used together. The optimal time of surgery varies from patient to patient. In some children the surgery is done later when correct measurements of squint can be obtained and after the vision in the lazy eye has improved by patching therapy.
4. Will the child need to wear glasses after surgery?
Surgery does not change the vision power of the child. If the vision of the child is low and he/she has been using glasses, these have to be continued after surgery. Failure to do so may cause recurrence of the squint.
5. Will one or both eyes need surgery?
This varies with the type of squint and the amount of deviation of the eye. Some cases require surgery in one eye only, others may require in both the eyes for better results. If the 1st surgery is done only in one eye, and there is a residual squint, 2nd surgery may have to be done on the other eye at a later date.
Retinopathy of prematurity – cause, risk factors & treatment
Definition: ROP is a disease of retina in premature children with a low birth weight and a history of prolonged oxygen therapy. The disease is characterized by abnormal growth of blood vessels on the retina which may lead to blindness.
Cause and risk factors
Premature babies born before 28-30 weeks of gestation and birth weight of less than 1250 gms are at risk of ROP. High O2 concentration contributes to the development of ROP. In premature babies, some parts of the retina are devoid of blood vessels, hence they suffer from lack of oxygen. Certain chemicals are released that promote growth of blood vessels in an irregular manner. Large amounts of O2 required for a baby’s survival is believed to be toxic to the blood vessels. These abnormal blood vessels cause bleeding, scar formation and later separation of the retina from its wall (retinal detachment) and decrease in vision. The disease is divided into several stages depending on the severity.
Treatment
This depends on the stage/severity of the disease
- Laser treatment: the aim is to destroy the immature retina and to slow down or stop the growth of the abnormal vessels.
- Cryotherapy The immature retina is destroyed using very low temperature
- Scleral Buckling: A silicon band is tied around the eye. This is done in later stages if the baby has developed a retinal detachment (Retina has separated from its wall)
- Vitrectomy: In this surgery the vitreous which is a gel like substance in the eye, is removed. The scar tissue pulling the retina, along with any blood in the gel, is removed. This helps the retina to go back and lie flat on the inner surface of the wall of eye.
Role of counsellor
- Should give clear information to the parents about the nature and progression of disease
- Explain how the treatment will work and prevent further damage to the eye
- Explain the visual prognosis if child has come at an advance stage
- Explain about the chances of myopia in the future
- Explain the need for follow up as instructed by the doctor
Frequently asked questions
1. Who should be screened for ROP?
Premature babies born before 32 weeks and weighing less than 1500gm should be screened
2. When should the baby be screened?
The first examination is done between 31 and 33 weeks of gestation or 2-3 weeks after birth. Then depending on the stage of the disease, follow up examination are done after every 1 week or 2 weeks.
3. What can be the complications of the ROP?
Retinal detachment – separation of retina from the eye wall leading to loss of vision, Bleeding within the eye, amblyopia – lazy eye, cataract, shrinkage of the eye, myopia or near sightedness, increase in pressure of the eye and squint – due to loss of vision or difference in refractive state of the 2 eyes.
4. What happens if ROP is not treated?
In 90% of case the disease heals on its own especially those of the early stage. But in 10% of cases the disease worsens and the child develops vision threatening problems. These cases have to be treated.
5. Does laser treatment cure the disease completely?
In most cases laser treatment is successful if done at the proper time. The baby is re-examined after 2-3 week to ensure that the laser treatment has worked. If so a regular follow up is required every 4 weeks and then several months later to see that no further change has occurred. If the laser treatment fails then a further laser treatment or a surgery, may be required.
Congenital anomalies of the eye
Congenital anomalies of the eye like anophthalmos, microphthalmos, corneal opacities, aniridia, albinism, coloboma and hypoplasia of disc and macula are associated with poor vision that cannot be corrected completely.
Role of counsellor
- The counsellor must offer emotional support
- He/she must encourage the parents and child to make best use of the residual vision.
- He/she must encourage to do visual stimulation exercises and use low vision aids as required.
Frequently asked questions on general anaesthesia
1. What is anaesthesia?Will my child feel the pain? Will she/he be awake during the procedure?
Your child will be operated under general anaesthesia. It is a procedure in which your child will be made unconscious and will have absolutely no pain during the surgery.
2. Is my child fit for general anaesthesia?
The anaesthetist will examine your child before the day of the surgery to ensure fitness for the surgery. It is very essential that your child be healthy, and free from problems like fever, cold, wheezing or systemic problems like heart diseases. Giving anaesthesia is risky in children with such problems. Certain additional tests will have to be done before surgery, like blood tests, X-ray of the chest, etc. A paediatrician’s opinion may be required in some cases.
3. What can I give him for food tonight or today?
Any food can be given, however, the child should neither eat nor drink anything 6 hrs prior to the surgery. Antibiotic drops have to be put 4-6 times the previous day. Dilating drops (for cataract surgery) will be put by the nurse before the surgery.
4. How long will the procedure take?
The whole procedure will take 1-2 hrs depending on the type of surgery. After the operation the child will be kept in the recovery room for 1 hour or more. One of the parents can stay along with the patient in the recovery room. Later the child will be shifted to the ward.
5. Will anaesthesia produce any side effects?
The child may vomit a few times. The child may be dizzy for few hours after the surgery. Food or drinks can be given to the child only when advised by the doctor. If there is any problem it should be reported to the ward doctor or nurse.
Key points to remember
- Refractive errors - wearing glasses is the only treatment for refractive error in childhood. Glasses should be worn continuously and regular follow up is essential to see for change in glass power.
- Amblyopia can be due to various causes like refractive error, squint, cataract, severe ptosis. Treatment is by removal of opacity in the visual axis, use of glasses and patching the good eye. Patching has to be done for a long duration as visual improvement is a slow process.
- Congenital cataract has to be treated by surgical removal of the cataractous lens. Cataract removal may be with or without IOL implantation. Surgery should be as early as possible.
- Squint is misalignment of eyes and is treated by strengthening, weakening or changing the position of muscles of the eye. It is always done after correction of amblyopia. Some squint can be managed with glasses alone. Squint surgery does not affect the vision.
- Retinoblastoma is the most common tumor of the eye in childhood. Child generally presents to the doctor by 2 – 3 years of age. Parents may notice a white reflex in the eye. It may or may not be hereditary. It is necessary to check the eyes of siblings as well as parents depending on the stage of tumor. It is treated by photocoagulation, cryotherapy, enucleation, chemotherapy or radiotherapy.
- ROP premature babies born before 28 – 30 weeks and weight less than 1500 gms are at high risk of developing retinopathy of prematurity. High oxygen concentration increases the risk. All such babies should be screened and treated by laser therapy at the optimal time. If left untreated, complications like vitreous hemorrhage and retinal detachment may occur and lead to blindness.
Student exercise
I. Write short answers
- What is refractive error?
- A patient diagnosed with refractive error comes to you, as a counsellor what is your role?
- How do you counsel the parents to make the child wear patching and glasses?
- Why do amblyopia cases need regular follow up? If they do not come for review what problem will arise?
- What is cataract? How does it affect the vision in a child?
- What is squint? What are the causes for squint?
- What are the points you explain to the patient in squint surgery counselling?
- What treatment is given to ROP children?
