An orientation to Refraction Chamber
Orientation to Operation Theatre
The operation theatre is the heart of an eye hospital. In some hospitals the operation theatre (OT) is called operating room. A team of skilled surgeons, nurses, OAs and anaesthetists operate on and care for patients in OT. Detailed scientific planning is imperative when designing an OT for effective utilisation and also for smooth functioning. When planning the operation theatre location, the placement of both the septic and aseptic theatres is to be finalised. The aseptic theatre can be one or many depending on the volume of operations done in the hospital. In aseptic theatre, cataract and other clean cases are done. Septic theatre is the place where enucleation of eye, dacryocysto rhinostomy and other ‘not clean’ surgeries are done. It is called a minor theatre because it is small in size compared to aseptic theatre and there is usually only one in a hospital. It is best to have septic theatre away from aseptic theatre.
It is often the theatre personnel who have the best knowledge about arrangement in the OT. The architect needs to work closely with theatre staff at the designing stage, to meet their specific requirements while constructing the OT. The theatre should be designed keeping in mind its future expansion plans
Planning of the operation theatre
An operation theatre should have
- A high standard of asepsis
- Maximum standards of safety for patients and staff from hazards due to electricity problem, fire etc.
- Optimum utilisation of space and staff time
Aseptic operation theatre location
The location of the operation theatre should be
- Free from general traffic i.e. away from the road side
- Free from noise and other disturbances
- Free from contamination and possible sources of infection especially toilets.
- Closer to the ward so that patients are transferred easily to and from wards.
The OT should have an entry and an exit point for patients. After surgery the patient should be guided out through the exit gate. While planning, the following points should be noted:
1. Patient load
The number of cases optimally expected for various ocular surgeries at a given time must be taken into consideration. In case of larger eye care institutions with high patient turn over , when high volume of patients is expected, OT should be designed in such a way that more than one operation theatre can be working at the same time.
2. Size
The size of each OT is to be functionally optimal. Large size operation rooms will give rise to problems in air conditioning, washing and cleaning. The optimum size is 6 X 6 meters width and it should not be more than 7 X 7 meters in length.
3. Walls and ceiling
These should be made of smooth plaster, and painted in off- white for easy and effective dusting and cleaning. The ceiling should be smooth to avoid any dust settling in it.
4. Floor
Floor should be of smooth surface without many joints and at the same time there should be no stagnation of water after the floor has been washed. Tiles should not be used because they may be slippery for both the patient and staff, especially when there is an emergency.
5. Doors
The OT doors should be wide enough to allow easy movement of patients, equipment, staff and materials. Doors could be of two-leaf type, double acting and at least 2 ½ meters wide.
6. Electricity sockets
All the sockets should be double and a fuse box should be kept in the operating room with provision to increase electrical capacity if needed. The position of the operating table should be decided before placing the electrical sockets. Sockets should be close to the equipment and must be properly earthed. Uncovered wires lying around the floor are hazardous. Socket outlets should be mounted on walls or ceiling or sunk into the floor. This needs to be carefully planned because there may be water leakage problem while cleaning and washing the room with water.
7. Efficient lighting
Efficient lighting is essential in an OT. Electric switches should be 1.5 meters above the floor and switches should be labeled to identify the correct switch and save time.
8. Air conditioning
Air conditioning helps in maintaining an aseptic environment in the OT by allowing only controlled air inside. This helps in providing optimum comfortable environment for surgeons as well as patients. The air conditioning system should be cleaned once, weekly.
9. Generators
The theatre must have an alternative electrical supply (generator) in case of power failure or other emergencies. The operating microscope light and flash autoclave should be capable of being powered by a generator. Generator must be of sufficient capacity to simultaneously support flash autoclave, microscope and other lighting.
If the power supply in the electrical system is not reliable, it is also worth while to put all machinery on to voltage regulators. These stabilise the equipment from fusing off.
10. Water
Water is essential for the effective running of operation theatre. Clean sterile filter water should be used for cleaning the instruments and scrubbing hands before the surgery. Ordinary tap water can be used for cleaning the theatre. If the water supply is unreliable ensure that containers with clean water are available in the scrub area. A separate reserve emergency overhead tank should be provided for the OT and should be periodically cleaned. Periodic microbiological examination of the source of water is essential.
11. Other conditions
Oxygen and nitrous oxide cylinders must be placed in a separate room away from naked flames. Easy access must be possible at all times.
There is always a high risk of fire accident in an operation theatre. Fire extinguishers should be fixed at strategic points.
The OT waste must be disposed after every surgery in a proper way to avoid infections.
B. Operation theatre zones
OT can be divided into 4 zones and they are as follows:
- Sterile zone
- Clean zone
- Protective zone
- Disposal zone
Sterile zone:This zone provides facilities such as
- Operation room
- Scrub room
- Anaesthesia room
- Instrument sterilisation
Clean Zone :This zone provides facilities such as
- Pre-operating or block room
- OAs’ work room
- Recovery room
- Anaesthesia / medication store
Protective Zone:This unit usually provides facilities such as
- - Reception room
- Waiting room for relatives of patients
- Dress changing rooms
- Pre anaesthesia room
- General store room
- Main auto clave room
- Trolley lay (store for OT trolleys)
- Control area for electricity
Disposal Zone: This zone provides facilities such as
- - Dirty / blood stained linen disposal
- Used head caps, masks, and socks disposal
All soiled materials both disposable and non-disposable should move without crossing sterile and clean zones.
C. Operation room set - up
Planning of space for the operating room area:
In the operating area the operating table, an adjustable chair for surgeon, instrument trolley, microscope and other necessary equipment have to be arranged. The sterilisation room should be adjacent to the operating room.
Size of operating table
- Length 180cm
- Height 70cm
- Width 47.05cm
Size of instrument trolley
- Length 67cm
- Height 90cm
- Width 45cm
A working space of 1.2 meters around the operation table is required. More space is needed if the theatre needs an anaesthetic machine, vitrectomy machine, monitor, etc., (Fig1.1).
The operating table must be of an adjustable type and needs to be firm and steady. It must be at a good working height especially if an operating microscope is used.
The surgeon’s chair height should be such that it allows space for surgeon’s feet to touch the floor comfortably and to use the microscope foot pedals. Surgeons’ chair should be well padded, have wheels in case of movements, adjustable height control and with back support. One bowl-stand for rinsing hands with sterile water and a IV - stand with tray and fluids are to be kept near the table.
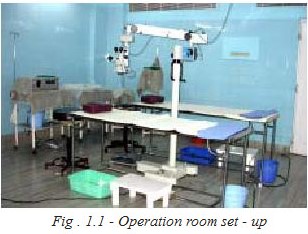
Operating microscope
If the operation theatre set up is to be used for teaching purposes, there must be an observer’s side scope, C.C.T.V, camera and monitor facility fitted on the operating microscope.
Instruments
There should be different sets of surgical instruments for different ocular surgeries
- - Bipolar diathermy with points
- Vitrectomy machine with vitrectomy probes
- Boyle’s apparatus for general anesthesia (when needed)
Sub-sterilising area
- Instaclave with cheatle forceps and container
- Stainless steel basin for cleaning instruments
- Electric water drums for boiling water or drum with clean sterile water. Adequate water supply, preferably distilled water, or sterile filter water for cleaning the surgical instruments and flushing the simcoe cannula and other tubes should be available
- Soft brush for cleaning surgical instruments
- Waste bucket
Scrub area
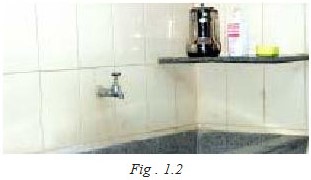
In the scrubbing area a sink is installed with running water. The sink must be deep enough to enable the staff to comfortably scrub their hands from fingers to elbows. Their hands should not touch the surface of the sink. The height of the tank should be 1 meter from the floor. If there is provision of clean water source, taps should have long knobs, which can be handled with elbows. If this is not available, a sterile water jug is kept for pouring sterile water for hand washing in the scrub area by one of the theatre OAs. There should be sufficient space to keep sterile water jugs, soap, solution, brush etc. The area must be very clean and tidy (Fig 1.2).
Orientation to septic operation theatre
Septic operation theatre is a place where the surgeries with risk of infection are performed, like evisceration, abscess drainage, dacryocystectomy, and dacryocys- torhinostomy. It is essential to organise and plan the location of the septic OT to prevent postoperative and intra operative infections in aseptic cases.
Location
It should be away from the main theatre. All the instruments and clothing used in septic OT should be separated from the main theatre by different colour codes.
It should be located at a place with limited access to patients.
- Should be a place from where patients can be easily transferred, but routine clean surgery patients have no access.
- Septic OT should have a separate clothing room and scrub room
- Should have a separate sterilization room away from the main theatre section, to prevent cross infection in places where asepsis is strictly maintained.
- The instruments and eye towels should be sterilised separately from other linen like coats. Sterilisation of septic operation theatre instruments should be in a separate area away from routine sterilisation area.
- Should have good ventilation to prevent infection.
- Most of the surgeries in septic OT are done
without a microscope so the lighting system

should give good illumination and be adjustable according to the surgeon’s need (Fig. 1.3). - A flash autoclave should be available to provide routine instruments in between the cases.
Staffing pattern
The OT manager is usually the OT nursing officer. It is the OT manager who takes care of the day to day running and the efficient management of theatres.
The OT manager ensures
- The availability of facilities, equipment, instruments and nursing staff for scheduled surgeries
- Proper care and maintenance of equipment
- Theatre cleanliness and sterility
- Adherence to work discipline
- Maintenance of OT records
- Good working relationships with other departments and administration
Some hospitals with high surgical volume have dedicated staff allocated for theatre. The OT manager obtains the list of surgeries to be done the next day. Under their guidance necessary preparations are done such as allocation of cases to surgeons, OAs duties, instruments to be sterilised, etc.
The number of staff allocated to work in the theatre depends upon workload for the specific operating session: number of surgeons operating, and types of surgery to be performed.
In smaller hospitals, where surgical volume is low or where surgery is done only weekly, they may not have separate staff for OT. Cross-trained OAs will be posted in OT whenever needed. Theses OAs are cross trained in OP, theater and in the ward. Sometimes an OA is given specialised training in glaucoma or retina clinic and if they are called for OT duty, the department may be reluctant to send them. One solution is to have part-time staff or staff from outside. They are given prior information about surgery, so that they can do necessary preparations for surgery. If OT training is given to all nurses in it will be easier to handle any situation.
Staff allocation in key areas
Operating area
- - Scrub OA – two persons per surgeon (if surgeon operates on two tables simultaneously)
- - Circulating OA – one person per surgeon
- - Local block room – 1-3 persons depending upon the volume of cases
- - General anaesthesia – 2 persons
Information board
At the entrance of the OT there is a notice board. The daily operation schedule is displayed. Notice boards are also called information boards. They give information about workload in the theatre for the day, and enable the theatre staff to plan. All hospitals may not have separate operating rooms for different types of surgeries. For example they may perform cataract, orbit and retina surgery in the same theatre and the time schedule is planned accordingly. Retinal surgery may require longer than a simple cataract surgery, so the OA responsible for setting up of the instrument trolley has to arrange it first and inform the patient the time of operation. The information displayed on the notice board helps the OA to begin the preparations without delay. The name of the operation will determine which drape pack, instrument set and supplies to select. All of the information on the notice board is important to the OA.
The OT information board should have the following details
-
- Patients name
- Medical record number
- Eye to be operated
- Type of surgery
- Name of the surgeon
- Name of the anaesthetist for general anaesthesia cases
- Name of the physician in case of high risk patients who need monitoring
-
- Total number of cases
- Specific and complicated cases. e.g. high risk cases, high myopia, complicated cataract, traumatic cataract etc
-
- General anaesthesia cases
Roles of the OA in the operation theatre
The OAs in the operation theatre play different roles for the effective and smooth running of the theatre. The OA may work as a scrub OA or as a circulating OA in the OT.
The circulating OA plays a vital role in providing the smooth flow of patients before, during and after surgery. In the circulating role they help the surgeon. They check the case sheet of the patient to verify that all necessary tests have been completed. The OA helps the doctors giving local anaesthesia and counsels patients about the same. They provide the sterile instruments and supplies needed for surgery. They also function as a vital link in communication between members in the sterile field and the unsterile area including patients’ attenders.
The scrub OA
The scrub OA is well trained and familiar with the procedure with which they assist. The OA scrubs, wears sterile gown and enters the sterile field. They arrange the instrument trolley and other emergency instruments which may be needed (like vitrectomy machine in case of posterior capsular rupture). The OA assists the surgeon throughout the surgery by handing over the necessary instruments.
The different roles of the scrub OA in the operation theatre are elaborately dealt in the speciality surgery Chapter.
Dress code in operation theatre
The theatre has a separate dress code. All medical personnel should strictly adapt the dress code inside the theatre and maintain the necessary standards of cleanliness. The theatre staff wears special theatre dress to minimise the risk of cross infection. The medical personnel wear only sterile clothes inside the operation room. They should not move around various zones while wearing sterile clothes as this may cause cross infections. The staff should not leave the OT with theatre linen.
Dress code
- - Dress as suitable (gown, pant, shirt)
- - The material should be cotton or polyester /cotton for easy washing and drying
- - Gown, pant and shirt should have pockets and be available in different sizes like small, medium and large.
- - If wearing the trouser suit, the shirt bottom must be tucked in to the trouser.
- - Dress should be any light colour preferably light blue, green or pink. (Fig. 1.4 & Fig. 1.4a)
Caps and face masks
Caps must be worn to cover the hair completely
- - Hair is a potential source of infection even if it is clean
- - Caps can be made out of cotton cloth with an adjustable tie to allow for different head sizes.
- - Caps and face masks are available in reusable or disposable form. In high volume set ups reusable

masks and caps are used. Disposable caps and face masks can be used but they are costly. - - A separate container is kept outside the OT to collect the used caps and face masks for washing purpose.
Slippers and over shoes
- - Before entering the theatre, OT staff should remove personal slippers outside the theatre and they should be kept in the place allocated for them. Mud attached to footwear is a potential source of the microorganism nocardia, which is a common cause of eye infection. Feet must be washed thoroughly. Clean slippers dedicated to OT should be available in various sizes and should be kept at the entrance of the OT. These are also available in disposable forms
- - Theatre slippers are normally made up of rubber for easy cleaning
- - Slippers should be scrubbed daily after use
- - Theatre slippers should not be used outside the theatre
A dedicated theatre OA
- - Should have a sense of sincerity, honesty, punctuality and compassion for all the patients.
- - Should have sufficient knowledge of medical terms to enable them to write notes.
Operation theatre discipline
The OA should come early before the start of surgery.They are responsible for the operation room arrangements, arranging the table and instruments. Theatre personnel should wash their hands thoroughly with antiseptic before entering the theatre. Theatre personnel should change into proper OT dress. Dress is to be provided for both male and female staff. Sterile caps and masks should be worn properly. Eating and drinking are strictly prohibited in OT area.
Personal hygiene
- - Staff must be meticulous about their own personal hygiene
- - Hair and nails must be kept clean and short. If hair is long it must be tucked up neatly
- - No nail polish or jewels like rings or bangles may be worn in the theatre
- - Cuts and abrasions should be treated and reported to the person in charge, who will decide if action needs be taken. This will prevent spread of infections both to the patient’s eyes and to other patients
- - Infectious diseases like common cold should get prompt and complete medical treatment to prevent spread of infection. Most of the infections are caused by droplet spread, so avoid coughing and sneezing in the sterile zone areas.
Patient’s hygiene
- - Patients coming for surgery should have a bath and wear clean dress
- - Before entering the operation theatre they should have their feet thoroughly washed
- - A patient with healed diabetic ulcer, Hansens or other infected diseases should be operated last
- - Disposable head cap and over shoes for feet are provided to every patient
- - These precautions are taken to prevent spreading infection
Summary
This unit deals with the proper planning of the operation theatre. The theatre area is a sterile place. It must be isolated, well set-up with clean, sterile environment and with all facilities like water, electricity, air-conditioning and dressing rooms. The medical personnel in the theatre should maintain strict discipline in handling patients and assisting in surgeries. Behavior inside the operation room must be well disciplined to avoid distraction. Personal hygiene of medical personnel must be maintained and the patient should also be instructed in the proper manner to avoid spread of infections both to themselves and to the medical personnel. The OAs play a vital role in making preliminary arrangements for the surgery; their early presence in the operation theatre will support the smooth flow of all the activities. They should foster certain qualities like punctuality, discipline, personal hygiene, and, above all, the commitment to their profession.
Key points to remember
- - Operation theatre should be located away from pollution (noise, air and dust)
- - The attender / visitors are not allowed to stand in front of the operation theatre
- - The OA checks the working condition of the equipment, electric connections, etc. prior to surgery
- - The OA takes responsibility to make arrangements for the repair and replacement of equipment and instruments.
- - An extra supply of instruments should be available when needed.
- - An extra supply of all operation theatre clothes must be available for visitors and staff.
- - The OAs should follow theatre discipline.
Student exercises
I. Answer the following
- Write a short note about the location of operation theatre
- Give details about the 4 zones of OT
- Briefly explain about the septic OT
- Write in detail about the dress code in OT
II. Write true / false
- Tiles should be used on the OT floor
- Sterilisation of septic operation theatre instruments need not be separate from routine main theatre instruments.
- Circulating OA normally assists the surgeon.
