Management of systemic emergencies in Operation Theatre (Intensive Care Unit)
ICU has become a symbol of modern medical care. It is a highly sophisticated unit engaged in delivering critical care to the patients. It is professionally managed by experts in order to deliver effective and efficient quality care.
DefinitionIt is a nursing unit staffed and equipped to look after critically ill patients who are often unable to communicate their needs. These patients require constant nursing care and observation.
Nature of serviceIt depends upon the unit
- Single discipline unit
- - Cardiac care unit
- - Paediatric intensive care unit
- Multidisciplinary ICU
- - Medical ICU
- - Surgical ICU
It should be located near the operation theatre and in a readily accessible location.
Staffing
- Medical staff: ICU should be staffed with two or three trained doctors and one senior medical officer.
- Nursing staff: It is according to the type of treatment given to the patient. Nurse: Patient Ratio should be 1:1. ICU should be managed by qualified and well trained R.N.s
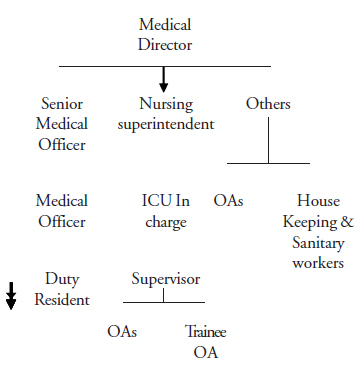
Staff
Equipment
- - Dressing tray
- - Emergency medicines trolley
- - Oxygen cylinder
- - Nebulizer
- - Glucometer
- - Pulse oxymeter
- - ECG machine
- - Cardiac monitor
- - CPR equipment – ambu bag, facemask
- - Ventilator and defibrillator
The emergency trolley must contain the following drugs: Injection Atropine, injection aminophyeline, injection lasix, injection adrenaline, injection calmpose, injection deriphyeline, injection dextrose, dopamine, dobutamine. etc. Also Venflon, IV fluids.
Physical facilitiesIt must be in an isolated area with adequate ventilation. Centralised A/C, adequate lighting, temperature and should be maintained at 60 to 70° F. Humidity should be 50 to 60 % .Noise should not exceed 60 decibels.
Registers- - Emergency drugs
- - Medication register
- - Equipment register
- - Narcotic - drugs record
- - Day and night report
- - Patient monitoring record
- - Temperature chart
- - Intake / output chart
OT Emergencies
Acute myocardial infarction
Definition
It is defined as sudden blockage of one or more branches of a coronary artery. It may interfere with cardiac function and can cause immediate death.
Causes- - Coronary spasm
- - Thrombosis
- - Chest pain radiating to shoulders, left hand, jaw and neck
- - Difficulty in breathing
- - Anxiety
- - Sweating
- - Tachycardia or bradycardia, low B.P, ECG changes like ST depression and T wave inversion
- - Patient is shifted to ICU on a stretcher
- - Oxygen should be started at 2.3 liters/minute
- - IV fluids – 5% dextrose, or ringer lactate
- - Sedate the patient with an injection of morphine, pethidine and an injection of phenergan
- - Sublingual sonbitrate 5mg if BP is normal. Injection perthidine
- - Dopamine drip should be started if BP is low
- - Monitoring of vital signs. Should be done constantly
Cardiac arrest
DefinitionAbrupt cessation of the cardiac pump function.Cardiac arrest may be reversible with prompt intervention but if timely intervention is not done, it leads to death.
Signs- - BP is not recordable
- - Absent pulse, respiration
- - Absent heart sounds
- - Pupils fixed, not reacting to light.( This may not be a useful sign in ophthalmology due to the use of dilating drops).
Basic CPR is ABC
- - Airway
- - Breathing
- - Circulation
Airway is maintained by artificial ventilation, either mouth- to- mouth or mouth- to-nose.
Mouth -to-mouth- - Remove any obstructing substances like dentures or food particles from the mouth by handkerchief
- - Place one hand under the nape of the neck and hyperextend it
- - Place the opposite hand on patient’s forehead, press down; compress the nostrils with the fingers
- - Take a deep breath, breath directly over the patient’s lips
- - Watch for chest movements. Allow the air to be exhaled
- - Repeat 4-5 times for an adult patient
- - Look for chest movements, listen for airflow
Mouth is closed with fingers. Air is blown into the nostrils.
CPR compression siteis found by measuring two fingers widths above the midline of the sternum.
Immediate action steps- - Shake and shout at the patient to see if there is any response
- - Open the airway by placing the patient in a supine position. Use head -tilt and chin - lift method
- - Use jaw thrust if any neck injury is suspected
- - Place the hand above the xyphoid process; arms must be straight, shoulders directly over the compression site
- - Compressions are delivered straight down with enough force to depress the sternum
- - Fully release the pressure on patient’s sternum
- - Compressions rate is 80 – 100 compressions permin. 15 compression, then give 2 ventilations
If two persons are performing CPR,5 compressions then 1 ventilation. After 1 minute, stop CPR and recheck carotid pulse, breathing. If absent,resume CPR
Hypoglycemia
DefinitionLow blood sugar. Signs and symptoms of hypoglycemia generally occur when the blood sugar level is below 60 mgs.
Causes- - Drugs- Insulin or oral hypoglycemic agents.
- - Diseases -like hepatic dysfunction, glycogen storage disorders.
| Symptoms | Signs |
| Headache | Tachycardia |
| Hunger | Cold and clammy skin |
| Giddiness | Coma or unconscious stage |
| Irritability | |
| Sweating | |
| Blurring of vision |
- - If the patient is conscious encourage them to take oral fluids
- - 25% dextrose - 2 ampoules (50ml) given intravenously
- - Maintenance IV drip - 10% dextrose for 12 - 24 hours
- - Administer glucagon 1 mg SC. If not improving with dextrose
Seizures
DefinitionSeizures are a manifestation of a massive discharge of a group or groups of neurons in the brain.
Causes- - Head injury
- - Drugs
- - Meningitis
- - Generalised
- - Focal seizures
- - Place the patient on the bed or floor, away from furniture and sharp objects
- - Clear and maintain the airway by suctioning.
- - Insert a mouth gag or airway into the mouth to prevent the patient from biting the tongue.
- - Head should be extended
- - If the patient is on a bed, keep the side- rails up for safety
- - Sedate the patient by injection of calmpose / midazolam Iv 50 mg, slow Iv / IM injection of phentyoin
Acute pulmonary edema
DefinitionAn increase in pulmonary venous pressure which results initially in engorgement of the pulmonary vasculature.
Causes- - Congestive heart failure
- - Aspiration of gastric contents
- - Shock to the lungs.
| Symptom | Signs |
| Difficulty in breathing | Tachycardia |
| Chest discomfort | BP is increased |
| Cough with sputum | Cyanosis (bluish discoloration of skin, lips, nails) |
- - Positioning the patient with a back rest
- - Start high oxygen by mask: 6-8 litres
- - Injection Lasix IVs (40 -160 mg) can be given
- - If BP is high, an injection of Nitroglycerine should be given through IV
- - Sedate the patient by injection of morphine and phenergan
Shock
DefinitionShock is the failure of the cardiovascular system to provide sufficient blood circulation to all parts of body
Types- - Haemorrhagic shock, caused by blood loss or plasma loss, as seen in burns and crush injuries. It is also called hypovolemic shock.
- - Cardiogenic shock caused by the heart failing to pump blood adequately to all parts of the body.
- - Anaphylactic shock is a life- threatening reaction of the body to an allergen. E.g. drugs (penicillin), food stuffs (fish, mushrooms, peanuts)
| Symptoms | Signs |
| Weakness | Urticaria |
| Nausea | Swollen lips, tongue |
| Thirst | Rapid pulse, shallow breathing |
| Dizziness | Cool & clammy skin |
| Breathlessness | Low BP, cyanosis of lips and earlobes |
| Loss of consciousness |
- - Airway to be maintained by oxygen supply
- - Keep the patient in a lying position
- - Elevate the lower extremities
- - Injection Adrenaline 1000 mg/ sc can be given
- - Fluid replacement by normal saline
- - Haemoaccel or blood transfusion should be started if there is severe blood loss.
- - Injection of Hydrocortisone 100 mg IV can be given every 8 hours
- - Basic monitoring of vital signs. Antihistamines- Injection Avil 50mg Im to be given.
In this unit the OA learns the importance of the Intensive Care Unit, its location near the theatre, and how to manage emergency cases efficiently. In the ICU the equipment should always be in perfect condition and all the drugs should be available at all times. The OA is to be alert and maintain the room appropriately.
Key points to remember- - Intensive care units patients require constant nursing care and observation.
- - Intensive care units must be in an isolated area and adequate ventilation is needed. Centralised A/C, adequate lighting, temperature at 60-700c should be maintained. Humidity should be 50 to 60 %. Noise should not exceed 60 decibels.
Answer the following
- What is the equipment to be kept ready in the Intensive care unit?
- Name the drugs stocked in an emergency trolley.
- What are the registers and records to be maintained in the ICU?
- What are the symptoms of acute myocardial infarction?
- List the steps in managing cardiac arrest.
- What are the causes and symptoms of acute pulmonary edema?
- List the steps in managing hypoglycemia.
- Write a short note on shock.
