Role of Ophthalmic Assistant in Cataract Surgery
Cataract
Cataract is defined as opacity of the crystalline lens or its capsule which prevents the passage of the rays of light and causes significant visual loss.
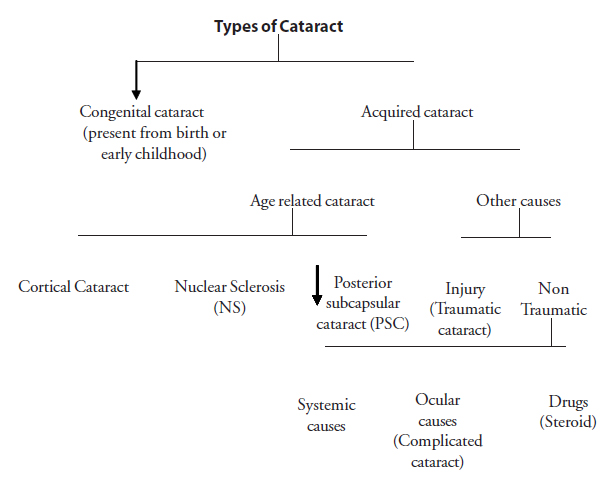
Cortical cataract
- Some opacities remain unchanged for prolonged periods, while others progress rapidly.
- Their effect on visual function varies greatly depending on the location of the opacification.Common symptom is glare from intense light.
- Progress slowly. Usually bilateral, though they may be asymmetrical
- Greater impairment of distant vision than of near vision. As cataract advances colour of lens changes to yellow, brown or black.
- Young age group
- May be due to injury, drugs or inflammation
- Patient complains more of glare
- Decreased vision
- Glare
- Contrast sensitivity
Once the patient has been admitted to the ward for surgery or treatment, as per the instructions in the case sheet, the OA is to do the necessary tests and record them in the case sheet. The following tests are conducted prior to the intra ocular/ cataract surgery.
-
Ocular examination
-
Visual acuity
Vision should be tested with and without glasses and with pinhole. In advanced and mature cataract,perception and projection of light should be tested in the entire four quadrants to rule out retinal problems. -
Refraction
Both the eyes should be refracted. If the extent of cataract does not correspond to the visual loss, posterior segment pathology should be ruled out by special tests.In such cases the possibility of poor prognosis is explained to the patient before the surgery. -
Intraocular pressure (IOP)
The tension must be normal. If the tension is raised due to glaucoma the tension has to be lowered either by operation or by medication. The IOP has to be normal before cataract surgery. Usually lOP is tested by Schiotz tonometer/non contact tonometer in both eyes. In borderline and raised lOP, differential tonometry and applanation tonometry are done. -
Syringing
Patency of nasolacrimal duct should be tested. If the duct is partially free with clear fluid, hourly antibiotic drops are started and conjunctival swab is taken for culture and sensitivity. The operation is performed only after the culture shows no growth. If duct is not free, with mucus or purulent discharge,Dacryocystorhinostomy / Dacryocystectomy is to be done and cataract surgery can be done after one month. -
A-scan, K-reading prior to cataract surgery
It is essential in case of IOL surgery. It gives the power of planoconvex IOL and +2 is added to this for biconvex IOL. In case of scarred cornea and irregular surface of cornea, the K reading will not be possible. In this case the other eye should be taken into consideration. -
Random blood sugar (RBS)>
Random blood sugar test is compulsory for all cataract patients to ensure that they are not diabetic. Normal random blood sugar value is below 160mgs. If the patient’s blood sugar is raised, additional test (fasting blood sugar and post prandial blood sugar) is done.
-
Visual acuity
-
General examination
Common systemic problems like diabetes,hypertension, and ischemic heart disease should be under control before surgery. Physician fitness is required in such cases prior to surgery.-
Blood sugar evaluation
In diabetic patients, fasting and post prandial blood sugar evaluation is done. Diabetes should be well under control, and if not controlled, physician's opinion must be taken and treatment added according to the doctor’s advice. On the day of operation, anti-diabetic treatment should be avoided to prevent hypoglycemia. (In uncontrolled diabetes, there is a chance of postoperative infection and delayed wound healing and the pupil is difficult to dilate). -
Blood pressure recording
In the presence of hypertension, blood pressure must be reduced to systolic 170mm of Hg and diastolic 100 mm of Hg. If surgery is done in uncontrolled hypertension, there is a grave risk of expulsive hemorrhage immediately after the section is made for cataract surgery.
If B.P is not controlled, physician's opinion is taken, important investigations like blood urea, serum creatinine and serum cholesterol may be done and treatment started according to the physician’s advice. Cataract surgery can be safely done with diastolic blood pressure under 100 mm Hg. In these patients, phenylephrine and adrenaline should be avoided and pupil dilatation is achieved with cyclopentolate and tropicamide.
-
Cardiac evaluation
Every cardiac patient should have fresh ECG . Surgery should be performed only after six months of the previous attack of IHD or MI. Here again adrenaline and phenylephrine should be avoided and surgery has to be done with cardiac monitoring. -
Asthma
In asthmatic patients, chest auscultation should be done for the presence of rhonchi. Patients should continue the anti asthmatic treatment. An injection of Broncho dilator before surgery can be given to make the patient comfortable on the operation table. -
Renal failure and renal transplantation
Blood urea and serum creatine tests results are obtained. -
Allergic conditions
If the patient has any history of medicinal allergy, a xylocaine test dose has to be given before giving local anaesthesia.Hence it is mandatory to get the information from the patient and record it in the case sheet. -
For paediatric patients
Hemoglobin and urine sugar should be tested. The anesthetist’s opinion is also needed. If the child has cough or cold the surgery should be postponed.
Hemoglobin, bleeding time, clotting time, blood group should be investigated for the patients with DCR, enucleation and evisceration.
The above mentioned tests are performed and recorded in the case sheet of the patient. The OA in the ward has to meticulously check whether all the necessary tests have been conducted and give instructions to the patient.
-
Blood sugar evaluation
Types of surgery
-
Intra capsular cataract extraction
This method involves removal of the whole lens with its capsule. It is rarely done now, except in cases where the zonular attachments are so weak that it is safer to remove the whole nucleus. -
Extra capsular cataract extraction
This method involves making an incision along the superior limbus, cutting open the anterior lens capsule, removing the cataractous lens and closing the wound usually with 4-5 interrupted sutures of 9-0 or 10-0 nylon. PCIOL may or may not be placed. A can opener capsulotomy is made and the nucleus delivered using the pressure and counter pressure method. Loose cortex is aspirated using the simcoe cannula. -
Manual SICS
A three step, valved tunnel is created which starts from the scleral surface about 2-3 mm from the limbus, passes through the sclera and the limbus into the cornea, and ends at the inner surface of the cornea just below the limbus. This tunnel is a watertight self sealing wound which does not require sutures. A large capsulo rheis is the preferred method of capsulotomy here, though a can-opener can also be used. Rhexis is followed be hydro dissection, in which saline is injected just under the rhexis margin to lift up the cataractous nucleus. The nucleus is then prolapsed into the anterior chamber and delivered using the irrigating vectis. Loose cortex is aspirated with simcoe cannula and PCIOL is placed. The wound is closed by filling the anterior chamber with saline and hydrating the side port (an opening made in the cornea near the limbus about and clock hours away from the edge of the tunnel, on the side of the surgeons dominant hand – i.e on the right in a right handed surgeon and vice versa). In SICS, viscoelastics should be liberally used to protect the corneal endothelium especially during nuclear delivery. -
Phacoemulsifiction
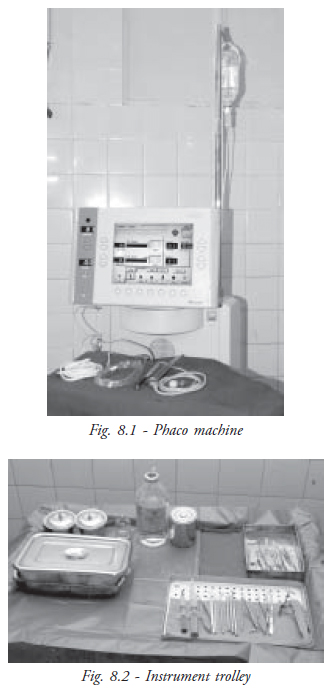
This method involves an even smaller incision than SICS. The incision may be scleral or limbal or clear corneal, and bevelled tunnel or stab entry may be used. Liberal use of visco elastics is advisable in Phaco. Capsulorhexis is a must, as is hydro dissection. Hydrodelination to separate the central nucleus from the epinucleus is also done. The side port entry is made on the side of the surgeon’s non-dominant hand; that is on the left side for a right handed surgeon and vice versa. The nucleus is broken up into smaller pieces using ultrasonic energy and aspirated. The Phaco machine hand - piece delivers the ultrasonic energy and aspirates the broken pieces. Cortex is removed using the I/A cannula or the Simcoe cannula and PCIOL is placed inside the bag. Rigid IOL or foldable IOL may be placed. The wound is closed by filling the anterior chamber with saline and hydrating the side port (Fig. 8.1 & Fig. 8.2).
- - Viscoelastic is very important in SICS and should be liberally used.
- - Trypan blue may be used to stain the anterior lens capsule in mature catracts in any type of surgery (ECCE, SICS, Phaco)
- - Sutures may be placed in case there is a wound leak or a pre-mature entry or flap tear. Several types of sutures may be used for e.g.: vertical sutures, horizontal mattress suture, infinity sutures, x- shaped suture etc.
- - CTR is used in cases where there is zonular weakness. It is inserted under the rhexis margin to stretch the capsular ring.
- - Cionni’s ring is used in case of sectoral weakness of zonules.
| Advantages | Disadvantages |
| Simple procedure | PCIOL is impossible |
| No microscope | Good best corrected vision but poor in quality |
| Advantages | Disadvantages |
| Better visual | Suture related |
| function | complication |
| Delayed wound healing | |
| Suture expenses | |
| Glass correction given after 3 months |
| Advantages | Disadvantages |
| No suture | Longer learning curve for surgeons |
| Quick rehabilitation | Residual astigmatism is present |
| Only one follow up | |
| Low cost, Minimum discomfort |
| Advantages | Disadvantages |
| Better quality of vision | Expensive |
| Fast rehabilitation | Difficult in advanced cases |
| Less tissue handling | Difficult technique |
| Less or no astigmatism |
- Foldable IOL
- Multifocal IOL
- Small size section is needed.
- It can be done through clear corneal tunnel.
- Can be done under topical anaesthesia
- Better quality of vision.
| Advantages | Disadvantages |
| Can be used for near vision and distant vision. So no reading glasses are needed. | Should be properly placed or else there will be discomfort |
Steps of surgery
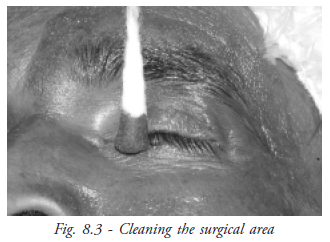
A. Extra capsular cataract extraction- Cleaning
The surgical area is cleaned using a swab or gauze dipped in 10% Povidone iodine. The lids and lashes are cleaned first followed by the adjoining areas in concentric circles of increasing diameter, the centre of which is the cornea. The entire area should be cleaned twice using two separate swabs (Fig. 8.3).
- Draping
A sterile towel or drape is placed such that only the cleaned surgical area is exposed. The patient’s hair should be properly tucked into the sterile cap and should not come into surgical field.
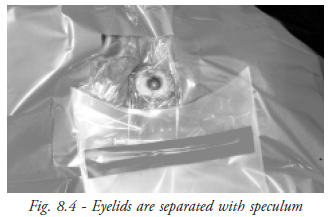
- Speculum
It is used to separate the lids as generally as possible without causing distress to the patient or pressure on the globe. The lid margin should be lifted clean off the globe (Fig. 8.4).
- Bridle suture
A bridle suture is placed over the superior rectus using cotton thread. The conjunctiva at the inferior limbus is grasped and the globe is rotated downwards. The superior rectus is located and the suture passed under it and anchored to the drape with artery clamp.
- Conjunctival section
- Cautery
- Limbal incision (groove)
- Corneal entry
- Anterior chamber reformation with visco elastic
- Can opener capsulotomy
- Cutting open the incision
- Nucleus delivery
- Cortex aspiration
- Placing the PC IOL
- Dialling the IOL
- Suturing the wound
- Washing and reforming the anterior chamber
- Conjunctival cautery
- Cleaning
- Draping
- Placing speculum
- Bridle suture
(In case of temporal SICS. Bridle suture is placed over the LR.) - Conjunctival section
- Cautery
- Scleral incision ( vernier callipers may be used to measure site and size of the incision)
- Tunnel is dissected
- Side port entry/ paracentesis (if Adrenaline or Trypan blue is to be used it is injected through the side part at this stage).
- Ac Formation with Visco.
- AC entry
- Capsulorhexis
- Hydrodissection
- Nucleus prolapse
- The nucleus is dialled into Anterior chamber
- Nucleus delivery
- Cortex wash
- PC IOL insertion and dialling
- AC wash
- Hydrating side port
- Conjunctival cautery
- Cleaning
- Draping in phaco, special plastic drapes are used.The part which is to cover the surgical site is transparent adhesive plastic. It is stuck over the eye lids and carefully slit open to allow access to the surgical area (Fig. 8.5).
- Speculum
- Bridle suture : may or may not be required.
- Conjunctival section is done only in case a scleral tunnel is made
- Incision -may be scleral or limbal or clear corneal
- Tunnel - as in SICS but much smaller. The size depends on the type of IOL (rigid / foldable /rollable) and the size of phaco sleeve. Some surgeons prefer a direct stab entry.
- Paracentesis (follow by injection of adrenaline /lignocaine/trypan blue/ visco)
- AC entry
- Capsulorhexis
- Hydro dissection and hydrodelineation
- Phaco emulsification: Nuclear cracking and aspiration of emulsified pieces. This is aided by an additional instrument passed through the side port without may be sinskey hook, cyclodialysis spatula or chopper (blunt or sharp).
- Cortex aspiration – usually done with I/A port though simcoe cannula may also be used.
- PCIOL insertion and dialling.
- AC wash.
- Stromal hydration.
- Conjunctival – cautery (if scleral tunnel used)

5. Instrumentation
- For cleaning and draping
- - Sponge holding forceps
- Lid speculum
- For bridle suture
- - Toothed forceps
- - Silcock’s locking needle holder
- - Elschnig’s forceps
- - Artery forceps
- - Spatulated needle
- For suturing the wound
- - Toothed forceps
- - Micro needle holder
- - Plain tying forceps
- - Suture with needle (9-0 or 10-0 nylon)
- - Small spring scissors
- For peripheral iridectomy
- Iris forceps
- Iris scissors or vannas scissors
- For IOL insertion
- Shepard’s lens holding forceps
- Sinskey hook
- Syringes
- - 5cc syringe (saline/simcoe)
- - 2cc syringe (visco/air)
- - 1cc syringe (Adernaline, Typan-blue, Deca/Gara)
- Extra capsular cataract extraction
- - Forceps
- - Dressing forceps with serrated edges at tip (for conjunctiva)
- - Colibri forceps (for cornea)
- - MC Phersons forceps (anterior capsule)
- - Westcott spring handled scissors
- - Blade breaker, razor blade
- - Cystotome: Fashioned from 26 G or 30 G needle using needle holder.
- - Corneal scissors
- - Lens expressor / nucleus hook and wire rectis.
- - Simcoe cannula
- - Dressing forceps with serrated edges at tip (for conjunctiva)
- - Forceps
- For SICS
- - Cleaning instruments
- - Draping instruments
- - Speculum
- - Instruments for bridle suture
- - Crescent blade on knife handle
- - Paracentesis knife
- - Angled keratome
- - Cystotome
- - Sinskey hook
- - Irrigating vectis
- - Simcoe cannula
- For phaco
- - Cleaning instruments
- - Draping instruments
- - Speculum
- - No 15 blade on BP handle
- - Paracentesis knife
- - Angled keratome
- - Cystotome
- - Sinskey hook / chopper with phaco probe
- - Cyclodialysis spatula with I/A probe
- - Phaco unit consisting of
- - Handpiece with phaco tip – 300 & 450
- - Phaco sleeve
- - I & A hand piece with tube
Cataract surgery complications and role of Opthalmic assistant (Scrub nurse)
- Premature entry during tunnel construction.
- If crescent blade is blunt, a sharper blade should be used and tunnelling started from another area
- If bleeding is obscuring the surgery field, cautery may be used
- If the pre mature entry is extensive, the section may be converted to ECCE - PCR
- The assistant should loosen the speculum and if he/she is pulling on the bridle suture, it should be released. The pressure on the eyeball should be minimal.
- At the end of the surgery, there should be no vitreous visible at the section/near the side port.
- Flow of saline in simcoe cannula is usually reduced – even dry tap may be used.
- Liberal amount of visco-elastic should be available.
- If the nucleus has not been delivered, instruments like irrigating and wire vectis, sinskey hook and cyclodialysis spatula should be ready.
Role of operation theatre OAs
Role of OA in the preoperative preparation roomThe theatre OA should arrive one hour prior to the start of surgery, wash the hands and prepare the ocular anaesthesia trolley.
- - Check case sheet
- - Check which is the eye to be operated
- - Reassure the patient
- - Explain to the patient what is going to be done (eg –RBB, facial block, topical anaesthesia, drops to be instilled, duration of surgery)
- - If patient needs something like a drink of water or a visit to the rest room, it should be arranged.
- - Check pupillary dilatation
- - Check whether block has taken up fully
- - Check that patients’ hair/dress/jewels etc are not going to come in the surgery field
- - Escort the patient to operation theatre
- - Arrange for stretcher if required
- - Show the case sheet to the assisting scrub nurse or surgeon
Receive the patient in a friendly manner and have them lie down in a comfortable position. Patient counselling involves creating awareness about patient’s condition and keeping them well informed about the local anaesthesia and the surgical procedure.
Preoperative case sheet checking- Patient’s name and the eye to be operated.
- Check that the consent letter is signed by the patient
- Check the patient’s eye for congestion, discharge, pustule etc
- Special attention and monitoring of the patient with high risk like cardiac, renal failure, asthmatic etc
- Patient with one eye, myopic or other ocular problem should be reported to the doctor
- Verification of A - scan and keratometery
- Explain to the patient the procedure and where exactly the retro bulbar and facial injection will be given
- Reassure the patient and allay the anxiety
- Clear any doubts regarding the procedure
- After giving injection, massage the eye ball with a sterile pad (making sure the eye lid is closed) for three minutes by giving intermittent pressure and check the on set of action. While giving the massage, talk to the patient softly so that the patient will have no fear. Clean the eye and the periorbital area with sterile cotton soaked with 10% Betadine
- Patient to be dressed with cap, bandage and leggings before being shifted to operation theatre
- Before entering the theatre the Ophthalmic Surgical Assistant has to wash her feet thoroughly. Remove chappels outside theatre.
- Change to proper theatre attire (Foot wear, cap, mask, gown)
- Check operating room schedule for operating surgeon.
- Wash hands thoroughly and enter the operating room. Connect electronic equipment to the switch board and place them in proper position. (E.g. The foot pedal in easy reach of surgeon’s foot). Check whether it is in working condition.
- Check that all the equipment is in good condition. If maintenance is needed inform the operating room supervisor.
- Place the waste bucket in a convenient place to receive the waste.
- Check that all the supplies are adequately stocked.
- Help the scrub nurse in scrubbing.
- Open the sterile gown and gloves for the scrub nurse and the surgeon.
- Tie the gowns for scrub nurse and surgeon.
- Pour sterile water over gloves to remove powder.
- Open the sterile pack required for surgery.
- Sterile wiper in a sterile jar
- Small cup of 10% Betadine
- Artery clamp or sponge holding forceps
- Assist the patient to the operating room table
- Check the name and eye to be operated.
- Prep the operative eye according to the surgical eye prep procedure.
- Assist the scrub OA in draping the patient.
- Keep the correct IOL ready, open and give to scrub nurse when instructed.
- When surgical procedure is completed, apply drops (as ordered by surgeon). Scrub OA will close the patient’s operated eye and place a sterile dressing and shield. Tie the bandage securely over the eye.
- Patient will be shifted from the operating table back to the ward.
- Complete operating room records must be attached to the case sheet, recording date of surgery, operative eye, name of surgeon, scrub OA, surgical procedure, and any intra operative complications. If an IOL is implanted attach the IOL sticker and sign the name.
- The packages are opened without touching the inside of the package. Pull the layers apart and gently let the sterilised item slide out of the package onto a sterile field
- The sterile storage room should be a limited - access area, well ventilated with controlled temperature and humidity. It must be clean and dust free
- Ensure that the sterile supplies are used before their expiry dates
- Any sterile item that comes in contact with an unsterile surfaces is considered contaminated
- The edge of the sterile container is not considered sterile once the package has been opened
- All the sterile packaged items expiry dates have to be checked once a week
- Before opening the package for use check the following. Each package is marked with
- Name of the item
- Date of sterilisation
- Date of expiry
- Load number
- Autoclave number
- Name of the personnel packing the item
Purpose – prevention of infection
Before starting the procedure explain the procedure to the patient and position the patient on the operating room table and cover them with a body cover.
Instill one drop of 5% Betadine into the operative eye. Before applying it, in a soft voice inform the patient. It is applied to clean the surface of the eye for surgery. Ask them to keep the eyes closed until they are informed to open them
- With sponge- holding forceps take Betadine soaked cotton ball and gently clean both eye lids and lashes starting from outer canthus to inner canthus. Then clean the eyebrow and peri- orbital area about five centimeters diameter around the operative eye. Dry the prepped area with sterile cotton if necessary.
- Keep the prep tray ready for the next case, so unnecessary delay can be avoided.
- Management of an infected patient: Each member of the theatre staff must be aware of their responsibility within the operating theatre, especially in managing an infected case. When operating a known infected patient the following procedures should be followed
- Always schedule such patients as the last cases for the day.
- Limit the number of staff in the OR and allow only those who are experienced.
- Remove all unnecessary items from the trolley and equipment from the theatre.
- Those who are involved in the procedure should wear double gloves.
- Discard all the disposable items from the trolley in a double wrapped bag and incinerate immediately.
- When discarding contaminated sharps, place them in containers that are closable, puncture resistant, appropriately labeled or colour coded and leak proof on the sides and bottom.Incinerate immediately.
- After surgery soak the instruments in 2% gluteraldehyde or any other strong disinfectant for ½ an hour.
- If the instruments are boiled, ensure that the water is discarded after use and the sterilizer properly cleaned.
- After soaking in antiseptic or boiling, the instruments are again washed with hot soapy water, rinsed in clean water and dried.
- The linen is soaked in antiseptic agent (E.g.Dettol 1:40 ratio) for 30 minutes and then washed as usual.
- If specimens are taken for lab investigation they should be clearly marked “CONTAMINATED” according to the hospital policy, wrapped in a plastic bag and sent immediately to the laboratory.
- Inform the anaesthetist when there is a risk of infection so necessary precautions will be taken for personnel and equipment. Once the operation is over the theatre must be washed with detergent, mopped with disinfectant and fumigated.
- In any surgery, the role of the assistant is to help the surgeon so that the surgery proceeds smoothly. The assistant should be careful in handling the instruments and should take care that his/her efforts at assistance do not block the surgeon’s view or hamper the surgeon’s movements.
- The ophthalmic assistant should check that all the tests have been done.
- If any of the test results are abnormal, or if the patient has some systemic risk factor, a physician’s opinion should be taken.
- The ophthalmic assistant should check that proper consent has been taken for the surgery.
- The ophthalmic assistant should also check which is the side to be operated on.
- Before starting the case, the opthalmic assistant should check that the supplies are adequate.
- If the patient on table is apprehensive/uncooperative, sedation should be arranged for or the surgery post-poned, counselling done and if required GA planned for the patient.
- Before cleaning and draping the patient, the ophthalmic assistant should note the presence of signs of recent infection, or inflammation if any. For e.g a patient posted for cataract surgery may overnight develop congestion and swelling due to drug allergy, or redness with watering and discharge due to conjunctivitis. Any mild discharge in the fornix should be investigated. A patient posted for DCR may develop some skin rashes or eruptions, or acute dacryocystitis with pain, redness and swelling in the sac area. Such conditions should be brought to the notice of the doctor / operation theatre supervisor.
- In ocular surgery, the cornea has to be kept lubricated by ophthalmic assistant using saline from an angled cannula.
- The drapes should not be allowed to get wet by overflow of saline over them. If they do, a dry folded towel should be placed over the wet area.
- If there is an intra-operative complication, the tension among the surgeon and the assistants should never be audible to the patient. If the patient does get stressed, he/she should be reassured both during and after the surgery.
- During intra-op complications, the ophthalmic assistant should assist the surgeon calmly and efficiently. If in doubt, a more experienced senior should be called to help.
In this chapter we have covered the different types of cataract surgery and the role of OA in the preparation stage as well as during the surgery. The OA is to prepare the patient for the surgery and neatly arrange the sterilised instruments in the trolley for the surgeon to use for the surgery.
Key points to remember- - The opthalmic assistant should check that all the tests have been done.
- - The surgical area is to be cleaned using a swab or gauze dipped in 10% Povidone using Pecidomiodine.
- - The lids and lashes are to be cleaned first followed by the adjoining areas
- - A sterile towel or drape is to be placed such that only the cleaned surgical area is exposed.
- - Speculum is to be used to separate the lids as gently as possible without causing distress to the patient or pressure on the globe
- - The assistant should be careful in handling the instruments and should take care that his/her efforts at assistance do not block the surgeon’s view or hamper the surgeon’s movements.
- What are the different types of cataract surgery?
- Write short notes on:
- Phacoemulsification
- Bridle suture
- Instruments needed for suturing the wound
- List the instruments used for SICS.
- Explain in detail the steps involved in cataract surgery.
- What is the role of OA in the block room?
