Introduction to Ocular Anaesthesia
The person who gives local anaesthesia (ocular) must have the back ground knowledge of the relevant anatomy and physiology of the eye, medicines used for anaesthesia, knowledge of the effects and side effects of the drugs used and management of complications both ocular and systemic. Such a person should be trained by a qualified medical practitioner.
Local Anaesthesia
- Local anaesthesia is very satisfactory and
convenient for many ocular surgeries like cataract
extraction, glaucoma, cornea and retinal
detachment surgeries.
- It is safer than general anaesthesia and the patient
remains conscious.
- It is quicker, creating less delays and allows better
use of theatre time if managed well.
- Much cheaper.
- Appropriate for practice even in remote areas with
basic hospital set up.
Contraindications
- Young children
- Mentally retarded persons.
- When verbal communication is difficult, or with
uncooperative patients.
- Drug sensitivity (allergy).
Trolley set up for ocular anaesthesia Drugs
- Xylocaine 2% with adrenaline- Xylocaine 2% without adrenaline
- Hyalase 1500 I/U (Hyaluronidase)
- Bupivicaine 0.5%

Materials
- Sterile syringes –10ml, 5ml, 2ml, 1ml- Sterile needles –22G X1 ½ inches for retro bulbar block
- Sterile needles 23GX 1 ½ inches for facial block
- Sterile cotton swabs in a sterile container
- Sterile eye pad in a sterile bin
- Bandages
Equipment
- Cheatle forceps with container- Torch light
- I/V stand
- BP apparatus and stethoscope
Eye drops
- Antibiotics- Steroids
- Mydriatrics (Tropicamide/cyclopent, phenylephrine)
- Miotic (Pilocarpine 2% )
- Local anaesthesia drops like 4% xylocaine
Emergency set up to manage systemic complications (Fig. 5.1).
Test dose of anaesthesia
The purpose of giving a test dose is to check whether the patient is sensitive or allergic to the drug.Method of giving test dose
1. Wash hands2. Draw up 0.5ml of xylocaine in a sterile syringe
3. Ask the patient to lie down and explain the procedure to them
4. Clean the site on the fore arm with spirit swab.
5. Inject the drug (0.2 ml) intradermal, with a 26 G needle and put a mark around the injected area
6. Check if the patient develops rashes, redness, oedema at the injection site or nausea, vomiting, breathlessness, sweating, or giddiness, within half an hour
7. If the patient is free from the above mentioned signs and symptoms ,the block can be given
Procedure for mixing hyalase and adrenaline in xylocaine vial
Wash and dry the hands- Take the xylocaine bottle, remove the metallic cap and clean with a sterile swab
- Take the ampoule of Hyalase and break the top with a file
- Draw up 1ml xylocaine with a sterile syringe and add to the hyalase ampuole (make sure the powder is dissolved well)
- Draw up the dissolved hyalase with the syringe and add it to the xylocaine vial
- In the same way take 1 ampoule of adrenaline and break the top with a file
- Draw up 0.5 cc of adrenaline from the ampoule and add it to the xylocaine vial
Block
Before giving the block, talk to the patient in a soft and comforting voice, explaining the reason for giving the block. Explain to the patient that if the eye ball moves it is not possible to do the surgery. To prevent movements, a block injection is given.There are two types of blocks; they are retro- bulbar block and peri- bulbar block.
Retro- bulbar or ciliary block
Purpose
1. Loss of sensation (anaesthesia) of ocular tissues.Restricts the movements of the eyeball (Akinesia) The amount of local anaesthetic used for a retro bulbar block is 2-3ml Xylocaine mixed with adrenaline and Hyaluronidase in a 5-ml syringe with a 22 gauge 1.5 needle.
Procedure for giving retro bulbar block
- Ask the patient to lie down in a comfortable face- up position- Wash and dry the hands
- Draw 2 or 3 ml Xylocaine in a sterile 5 ml syringe and attach a 22 gauge 1.5inch. needle
- Clean the site of injection (periocular region)with a sterile swab
- Ask the patient to look straight ahead
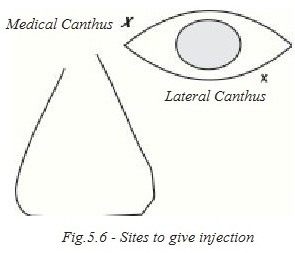
- Prick below the lower lid (1/3 distance from the outer canthus and 2/3 distance from the inner canthus) into the muscle cone (Fig. 5.2).
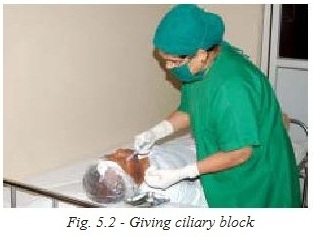
- If no blood comes into the syringe, give the injection, withdraw the needle slowly and apply pressure for 2-3 minutes after closing the eyelids.
- Massage the globe for 5 minutes with a sterile pad, making sure that the eyelid is closed, otherwise the cornea might get damaged (Fig. 5.3).

Disadvantages
1. Retro- bulbar haemorrhage may occur.2. Globe may be perforated.
3. The solution may enter the subdural space of the optic nerve.
Peribulbar block
Anaesthetic solution is injected into the orbit but not into the muscle cone.a. The purpose is the same as that of retro- bulbar block. However the risk of causing a retro- bulbar haemorrhage is less with this technique.
b. 3 ml of xylocaine adrenaline and hyaluronidase is drawn up in a 5-cc syringe and it is attached to a 22-gauge needle (Fig. 5.4).


Disadvantages
- Chances of globe perforation (common in peribulbar block)- Conjunctival chemosis
- Late onset of anaesthesia
Purpose of giving massage
- To reduce the intraocular pressure- To aid in the spread of the local anaesthetic
How to check the block
After giving a retro bulbar or peribulbar block and massage, ask the patient to look up, down, and to the left and right. If all these movements are restricted the block is fully effective.Facial block
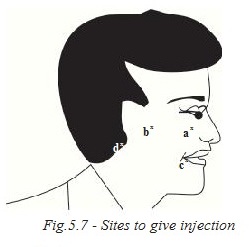
For intraocular surgery it is necessary to block the facial nerve (7th cranial nerve) which supplies the orbicularis oculi muscle, so that the patient cannot squeeze the eyelids.The injection is given where the nerve winds around the neck of the mandible bone (lower jaw) – O’Brien’s technique is the most commonly used for blocking the facial nerve. (Fig. 5.7)
Other methods are
a) Van lint’sb) Atkinson’s
c) Nadbath - Ellis
Procedure for giving a facial block
- Wash and dry the hands- Draw up to 4 ml of xylocaine in a sterile 5ml syringe and attach a 23 gauge 1" needle
- Clean the area with a sterile swab
- Ask the patient to open their mouth and feel for the head of the mandible bone
- Ask them to close their mouth
- Inject the anaesthetic slowly just below the head of the mandible, at its neck where the nerve winds around.
Note
Do not use adrenaline if the patient is hypertensive or has cardiac problems. Adrenaline stimulates the heart and increases blood pressure.1. Duration of action for xylocaine 2 percent is 1- 2 hours
2. Duration of action for bupivacaine 0.5 percent is 3-5 hours
3. Xylocaine is fully effective within 10 minutes of administration
4. Bupivacaine is fully effective within ½ an hour of administration
Attitude
- Talk softly to the patient- Tell them that an injection is given to restrict the movements of the eye ball and eye lids, and to avoid pain, which will enable the surgeon to do the surgery successfully.
Topical anaesthesia (Xylocaine 4%)
Anaesthetic drops like Xylocaine or proparacaine are instilled in the eye several times. This avoids all the complications of retro and peribulbar blocks. It works well for phacoemulsification cataract surgery performed by an experienced surgeon.Patient’s cooperation is very important; hence the procedure should be explained clearly to them. The anaesthetic drops are applied five times in the eye which is to be operated, at five minutes intervals. No injection is required
Inclusion criteria
- Immature cataract- Nuclear sclerosis grade I and II
- Cooperative patient in the age group 45 to 60
Exclusion criteria
- Combined surgical procedure like trabeculectomy and cataract extraction with IOL implantation, corneal graft with IOL implantation, long surgeries like retinal detachment etc.- Small pupil
- Pseudo exfoliation
- Corneal opacity
- Nuclear sclerosis group III and IV
- Psychiatric patients, mentally retarded patients, deaf patients, any un cooperative patient, and children.
Minor procedures which can be performed under topical anaesthesia are
- FB removal- Suture removal
- Checking the duct patency (syringing)
- Tonometry
- A scan keratometry
- Pustule pricking, etc
General emergencies of block room
- Drug toxicity / Hypersensitivity (allergy )- Central nervous system may be affected after retro bulbar anaesthesia (Fig. 5.8).

Symptoms
- Dizziness- Drowsiness
- Mental confusion
- Convulsions (fits)
- Respiratory distress
- Loss of consciousness
In cardiac patients the symptoms
- Sweating- Loss of consciousness hypotension (fall in blood pressure)
- Bradycardia (fall in heart rate)
- Cardiac arrest
- Trauma to major blood vessels leads to epilepsy, respiratory and cardiac arrest.
Asthma patients may develop breathlessness and pulmonary edema.
- Treatment: deriphyline and Inj. Lasix.
Diabetic patients may develop hypoglycemia in the block room.
Symptoms
- Giddiness- Loss of consciousness
- Sweating
Treatment
Check blood sugar immediately by Glucometer and give I.V.Dextrose 20%An emergency trolley must be kept ready with the following:
Medications
- Inj.Adrenaline- Inj. Deriphyllin
- Inj.Aminophyllin
- Inj.Decadron
- Inj.Avil
- Inj.Hydrocortisone
- Inj.Lasix
- I.V. fluids
- 25%Dextrose
Equipment
- Oxygen cylinder with flow meter- IV set
- Venflon
- Disposable syringes & needless
- Ambu bag
- Boyle apparatus with laryngoscope & endotracheal tube
- Pulse oxymeter
- ECG monitor
The team members must be able to identify the situation and treat symptomatically. The physician and anaesthetist should be informed immediately.
Student exercise
Answer the following
1. What are the uses of local anaesthesia.2. List the contraindications of local anaesthesia.
3. Name the drugs to be kept in the trolley for ocular anaesthesia.
4. List the materials and the equipment needed to give ocular anaesthesia.
5. Describe the method of giving a test dose.
6. What is the procedure to mix hylas in xylocaine vial.
7. Write in detail about retro bulbar block.
8. Describe the procedure for giving a facial block.
9. Write a short note on topical anaesthesia.
10. List the medicines to be kept in an emergency trolley.
General anaesthesia
General anesthesia is a process of making the patient attain a reversible state of unconsciousness with the help of multiple pharmacological drugs thus removing pain during surgery (Fig. 5.9).In ancient times attempts were made to relieve the pain of surgery by oral or rectal administration of herbal plant preparations. Dr.William Thomas Green Marton first introduced Ether for painless surgery on 16 th October 1846 to this world. Hence it is declared as Ether Day or World Anaesthesia Day.

Purpose of general anaesthesia
1. The patient should not feel pain during surgery.2. The patient must be in an unconscious state, and not to know what is happening to them.
3. During anaesthesia the muscles are relaxed, so that the surgeon can do the surgery more easily.
Indication of general anaesthesia
1. Children2. Mentally retarded patients, as such patients can not cooperate for surgery
3. Long duration surgery e.g. orbitotomy, retinal surgery
4. Un cooperative patients
5. Patients with allergies to local anesthetic drugs
Equipment used for general anaesthesia
Boyle’s apparatus
It is the machine used to give general anaesthesia by using a mixture of the gases Oxygen, Nitrous oxide and Halothane gevoflurane. It is also useful in emergency situations to give oxygen through a bag and mask or with the help of endotracheal tubesPulse oxymeter
In 1983 the Nellcor pulse oxymeter was introduced. The pulse oxymeter represents a very significant advance in patient safety. It gives the patients’ pulse and oxygen saturation.Suction apparatus
1. It is useful in any unconscious patient to clear the airway2. To clear the oral cavity and throat of secretions at the end of the surgical procedures before extubation
3. If there is excessive bleeding during the surgery such as DCR, the oral cavity and field of surgery can be cleared with the suction apparatus.
Laryngoscope
It is used to view the larynx and adjacent structures for inserting an endotracheal tube. Two different sizes are available, adult and paediatricEndotracheal tube
It is inserted into the trachea and delivers gases and vapours from the apparatus to the patient’s lungs.Different types of tubes are available.
- Cuffed tube
- Un- cuffed tube
- RAE’s tube
- Spiral embedded tracheal tube
Formula for calculating diameter of endotracheal tube is( age in years +16) /4. This formula is used only for children up to the age of 10. After calculating the size by this formula we can add or subtract 0.5mm accordingly. Endotracheal tubes are available in various sizes.
Airway (Oro Pharyngeal airway)
It is made of rubber or plastic. It extends from the lips to the pharynx. It fits between the lips and teeth in front and the tongue and posterior pharyngeal wall at the back. Different sizes of airways are available.Purpose
1. To help to maintain an open airway.2. To prevent patient from biting and obstructing a tracheal tube inserted through the mouth.
3. To protect against tongue biting during epilepsy (seizures)
4. To prevent the tongue falling back in to the posterior pharynx
Gases
Oxygen
It is a tasteless, colourless, odorless gas which forms 20.95 percent of the atmosphere. The oxygen is absorbed by the lungs and after metabolism in the body it is eliminated as carbon dioxide. Oxygen is stored in a black body and white shoulder cylinder. The gas is stored at high pressure in cylinders, 2000 pounds/square inch.Nitrous oxide
It is stored as a liquid at low pressure in a special cylinder painted “French blue colour". During balanced anaesthesia the depth is maintained by 60% nitrous oxide and 33% oxygen. It is a weak anaesthetic agent.Halothane
It is a non- inflammable, volatile liquid, with a sweet smell. It is a bronchodilator and does not irritate the airway. It has a moderate effect on skeletal muscle relaxation. It is favored for induction in children, especially for rapid induction and recovery.Other drugs used for anaesthesia
Thiopentone
Is a short acting barbiturate commonly used for induction of anaesthesia (Fig. 5.10).Propofol
It is a newer intravenous induction agent. It is a painful injection. The pain can be overcome by adding xylocard to the injection Fentanyl is a synthetic opioid. It is a powerful analgesic with predictable results and minimal incidence of post operative nausea and vomiting, or respiratory depression Suxa Methonium is a depolarizing muscle relaxant drug with short onset (1-1.5mins.) and a short duration of action (5-10mins.)Vecuronium, atracurium
These are all non- depolarising muscle relaxants. Intubations can usually be performed about 2mins. after injecting the relaxant.Duration of action
1. Atracurium 10-15 mins.2. Vecuronium 30-40 mins.
Neostigmine
The action of a muscle relaxant is usually reversed by neostigmine. Bradycardia and hypotension are the major side effects. These side effects can be prevented by giving atropine or glycopyrrolate along with the drug.
Anaesthesia tray contents
| Name of the articles | Purpose | |
| 1. | Venflon, scalp vein set | To start IV line |
| 2. | Syringes | To load medicines |
| 3. | IV set | To transfuse IV fluids |
| 4. | Xylocaine jelly | To anaesthetise and lubricate the endo tracheal tube |
| 5. | Cylinder key | To open the O2,N2O cylinders |
| 6. | Airway | To maintain the airway |
| 7. | Laryngoscope with blade | To help with tracheal intubation |
| 8. | Endotracheal tube | To give artificial ventilation |
| 9. | Mask with circuit | To ventilate the patient |
| 10. | Head ring | To prevent shaking of the head |
| 11. | Booegys | To help in difficult intubation |
| 12. | Maggiles forceps | To pack the oral cavity and Pharynx with gauze |
| 13. | Plasters and scissors | To place the venflon and endotracheal tube |
| 14. | Spirit and cotton balls | To clean the injection site |
| 15. | Small pillow | To extend the neck |
| 16. | Laryngeal mask airway | To give O2 and anesthesia gases |
Pre operative preparation for general anaesthesia
1. History
- Birth history - parents of infants should be asked whether child was born at term and about any other problems during and after birth- History of recent upper respiratory tract infection (cough, cold)
- History of allergic reaction to drugs or food
- History of previous surgery and anaesthesia
- History of drugs being taken for any major illness
- History of systematic problems like IHD, DM, HT, epilepsy and asthma should be noted
2. Investigations
- Before surgery the patients should under go blood investigations- Hemoglobin and urine sugar are a must for all patients
- Bleeding time, clotting time, blood grouping for surgeries with likelihood of excess blood loss from DCR, orbitotomy, enucleation, etc. should be noted
- Patients above 40 years of age require ECG, blood sugar and urea examination
- If the patient has any systemic problems, the physician must be consulted
- Aneasethetist should be informed about any systemic conditions like diabetes, hypertension, IHD etc.,
Preparation of the patient for general anesthesia
- Inform the patient and their parents (if the patient is a child) about the surgery and type of anesthesia to be given- The investigation results should readily be available for the anesthetist
- Patient should fast for 4-6 hours before surgery. (liquid for 4 hours, solid for 6 hours)
- Male patients should shave before surgery
- All patients should have a bath before surgery
- Any prosthesis (i.e.) artificial eye, dentures (false teeth) should be removed and the anaesthetist should be told about them
- The patient must wear a clean loose cotton dress
- All jewels should be removed and hair tied up properly
- The consent form should be read and signed by the patient, parent, or guardian
- The weight and temperature of the patient recorded in the anaesthesia chart
- The OA who gives the injection must record the name of the drug, the dose, date and time given in the notes and sign their name
Before sending the patient to the operation theatre the OA should ask if the patient wants to pass urine. If so a bedpan is provided. The patient should not be allowed to walk as they may feel drowsy from the pre-medication.
Pre-medication depends on the weight of the patient and is given forty- five minutes before surgery according to the anaesthetist instruction. The purpose of pre-medication is to help the patient feel calm and relaxed.
Drugs used for pre-medication and their purposes
1. Atropine (or glycopyrrolate) – to reduce secretions and prevent bradycardia during2. Surgery
3. Midazolam _ To produce sleep and avoid anxiety
Causes of bradycardia during anaesthesia
Bradycardia can occur during the following steps- Laryngoscope introduction
- Tracheal intubation
- Tracheal suctioning
- Traction on eye muscles
Role of Anaesthetic OA
The senior OA should- Know how to set up the anaesthetic machines and equipment
- Check that the machines and apparatus are in good working condition and check that the oxygen and nitrous oxide cylinders are full. The cylinder opening key must be in the Boyles apparatus
- Check the anasethesia tray for the presence of all anaesthesia drugs including emergency drugs.
- One laryngoscope with all sizes of blades should be tested and placed on the tray
- Endotracheal tubes of various sizes and stylet (or boogy) for use in difficult intubations
- Mask of appropriate sizes and airways must be kept on the tray
- A functioning suction apparatus with catheter should be available
- A BP cuff must be applied and the patient’s BP should be taken before starting the anaesthesia
- Pulse oxymeter (or cardiac monitor) should be in place prior to giving anaesthesia
- Anaesthetist’s assistant must be familiar with the patient’s history, physical status, and should anticipate problems during surgery and anaesthesia.
- Check the ECG monitor
- Make sure there are sufficient syringes and needles.
- Any defect found in the working of anaesthetic equipment must be reported to the anaesthetist immediately.
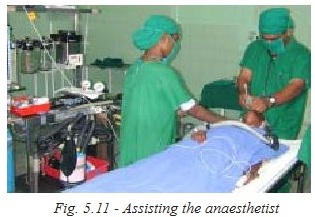
Assisting the anaesthetist
- The OA should help the patient lie down in a comfortable position on the operating table and give assurance if the patient is nervous- All equipment needed should be readily available before the anaesthetist induces anaesthesia
- During induction the OA should help the anaesthetist by giving the laryngoscope and endotracheal tube. They should keep checking the patient’s pulse and oxygen saturation
The OA should apply the BP cuff to the patient’s arm and connect them to the ECG monitor (Fig. 5.11).
Note
At all times an endotracheal tube, atropine and Succinylcholine must be available along with a mask, airway laryngoscope and suction apparatus. During extubation (removal of tube) the anaesthetist may require suction apparatus, and should help in turning the patient’s head down or turning to one side in case of vomiting. They may need drugs and to re- intubate the patient if there is any respiratory problem. The patient should be placed in the recovery position before being transferred to the recovery room.Care of the patient in recovery room
On receiving the patient in the recovery room, the OA should observe the following:- The patient should lie on one side (in the lateral position) with the head and neck extended and knees should be flexed (bent). This is to prevent airway obstruction by the tongue.
- Breathing
This is monitored by observing
- Respiratory rate
- Pattern of breathing
- Noisy breathing
Observe the pulse oxymeter and see that SPO2 is always above 95% in room air.
Circulation
- Colour of the patient’s tongue, lips, fingers should be watched- Feel the pulse
- Check the BP
Remember to listen carefully to the anaesthetist’s instruction
- Take careful note of the instructions from the surgeon- Keep noise level to a minimum.
The recovery OA should maintain an accurate record of the following
- Time of patient arrival in recovery room- Observation of pulse, BP and respiration
- Any complication occurring during recovery. The anesthetic nurse should inform the anesthetist immediately and get their help to relieve the problem. If there is any special postoperative instruction, they must inform the ward OA about this clearly when the patient is handed over to the ward OA.
After full recovery the patient is shifted to the ward by stretcher accompanied by the OA who hands over the report of the patient to the ward OA. Oral fluids may be started after 2-3 hours if the patient is absolutely awake, and soft solid diet is given after 6 hours. The patient should be monitored by the ward OA throughout the day.
The recovery room must be equipped with an emergency trolley containing drugs and equipment required in an emergency. This should be checked daily by theOA in charge. In addition, the following items must be ready;
- Pulse oximeter
- Oxygen cylinder with O2 delivery system like Nasal O2 catheter or Venturi mask. (or) Boyles apparatus
- Suction apparatus
- BP apparatus and stethoscope
- IV stand
- Kidney tray
- ECG machine
Problems and emergencies in recovery room
- Respiration may be depressed or absent- Obstruction of airway with vomiting material
- Cyanosis (bluing of body, especially lips and fingertips)
- Laryngeal spasm (narrowing of upper air way)
Management
- Check the patient’s airway; make sure it is clear. Extend the neck, pull the jaw forward and turn the head to one side- Use suction if necessary
- Give O2 by mask
- Inform the anesthetist if there is no improvement
- In case of laryngeal spasm, the patient may require re-intubation. The anaesthetist should be informed immediately
Vomiting
The patient should always be in the recovery position when they are unconscious. If they vomit in this position it is not aspirated and can be cleared by use of suctionShock
This is due to heavy blood loss in some surgeries like orbitomy, enucleation
Signs / symptoms
- Weak and rapid pulse- Low blood pressure
- Pale, cold and clammy skin
- Breathing shallow and fast
Management
Place the patient in a head down position or lift the feet to facilitate blood flow to the brain. Start the IV fluid immediately. Inform the anaesthetist immediately.Pain
If the patient becomes restless and complains of pain, the anaesthetist will prescribe postoperative analgesic or sedation.Fever
If the patient has high fever, sponging is done with cold water. If fever is persistent give antipyretic drugs according to the doctor’s instructions.Summary
Three types of anaesthesia are used: local, general and topical. The indications and contraindications that must be considered before surgery are explained. Equipment and medications were explained, as well as the necessity for administering these anaesthesias. The importance of giving a test dose is stressed to avoid allergic reactions. The OA should take all precautions for a safe outcome. The OA must be aware of a plan to handle any postoperative complications.Key points to remember
- Different types of anaesthesia are used for different surgical procedures.- Trolley set up for local anaesthesia is essential
- Emergency trolley must be complete and present in the postoperative area
- Preoperative history of the patient must be complete to avoid complications
- The OA must be well- versed with postop medications and their uses
- The OA must be familiar with all instruments and equipment and their uses.
Student exercise
I. Say “True or False" of the following statements
1. Hemoglobin and urine sugar tests are not a must for all patients.2. The patient must wear a clean loose cotton dress.
3. Atropine drug is used to produce sleep and to avoid anxiety.
4. Anaesthesia drugs include suxamethonium, Halothane, Fentanyl and Neostigmine.
5. Suction apparatus is useful in an unconscious patient to clear the airway.
II. Fill in the blanks
1. _____________is the machine used to give general anaesthesia by using a mixture of the gases ___________and __________.2. Endotrachael tubes are available in ________ sizes.
3. ________________protects against tongue biting during epilepsy
4. Nitrous oxide is stored in special cylinder painted_____________colour.
5. ____________is favoured for induction in children especially for rapid induction and recovery.
III. Answer the following
1. Why do we give anaesthesia to patients.2. What are the points to be noted in the history of patients.
3. Write in detail about preparation of the patient for general anaesthesia.
4. What is the role of the anaesthetic nurse.
5. Mention the names of the instruments used for anaesthesia.
6. What are the drugs used for anaesthesia.
7. What is the role of the OA in the recovery room.
8. What are the symptoms of shock and how are they managed.
9. What are the gases used for anesthesia (GA).
