Postoperative Ophthalmic Nursing Care
Preparation of Dressing
Required materials
- A basin containing sterile water
- Clean cotton
Step by step procedure in preparing wiper
- Wash and dry the hands thoroughly
- Fill half the basin with sterile water
- Immerse the cotton pieces into the water
- Take a pinch of cotton from the water and roll it into a round ball (round wipers- to wipe the eye of the patient after any procedure).
- Take a pinch of cotton from the water and roll it into a small strip with the ends tapering a little (This method is for strip wipers- used to remove dust / foreign body).
Points to Remember
The left over cotton must be used in preparing wiper balls and wiper strips. This will reduce the wastage of cotton.
Eye pad preparation
Required Materials
- A neat Mat
- Scissors
- A clean cotton roll
- Gauze piece
Step by step procedures in preparing eye pads
- Wash and dry the hands thoroughly
- Spread the mat in a clean dry area
- Spread the gauze piece and cut it into 9 square pieces
- Unroll the cotton
- Keep the left thumb on the front end of the cotton roll (the measurement must be 6 inches) and cut the cotton in a rectangular shape
- When one piece is finished, keep the rectangular shape cotton on the next part of the roll and cut the next piece
- Take one piece of the rectangular shape cotton and one strip of gauze piece
- Keep the cotton on the middle of the gauze strip and start rolling the gauze from bottom to top of the cotton piece. The rolling should be tight
- Cut the strip wrapped cotton in to square pieces. Each piece should measure 6 inches square. Use the thumb measurement for cutting the pieces
Points to remember
When you start cutting one roll of cotton complete the role and then start with the pad preparation.
Bandage preparation
Required materials
- A neat mat
- Scissors
- A clean gauze bundle
Step by step procedure
- Wash and dry the hands thoroughly
- Spread the mat in a clean dry area
- Take a roll of cotton from the bundle and fold it into 2 cubit measurement (cubit-length of the arm)
- Cut the extra side pieces
- Leave one lengthy end and one short end. Fold the strip and cut to the level of the ear.
- Eight pieces of bandage could be prepared from one roll of gauze.
Points to remember
Right place, right measurement, right method must be followed while preparing the bandage, pad and wiper.
Assisting Doctors in Ward Rounds
a. Preparations
- Ward should be clean and tidy.
- Only one attendant per patient should be allowed.
- Avoid children in the ward.
- Patient case sheets should be complete with all relevant information regarding the patient.
- Diagnostic tray should be ready for use (Local anaesthesia drops, antibiotic drops and ointment, steroid drops, sterilized cotton balls, fluorescien strips etc.)
- Do not conduct ward rounds during lunch time/visiting hours.
b. Conducting ward rounds
- The ward OA is to stay on the patient's left side to help in the examination
- Carefully and gently remove the eye dressing , instil antibiotic drops and wipe around the eye with wiper
- Help the patient to sit before the slit lamp, request the patient to keep their chin on the chin rest and forehead against the forehead bar.
- After the doctor has completed the examination, escort the patient to a nearby chair
- As per the doctor's instruction apply the drops or ointment and tie a new bandage
- Record orders/get them signed by doctors
Identification and Management of Postoperative Complications
Cataract surgeries demand an excellent visual outcome. The technology is far improved which has to a certain extent minimized the grave complications. Early detection and treatment of postoperative complications give good visual prognosis. Proper preoperative evaluation with a good postoperative care prevents a patient from going into catastrophic vision threatening complications.
Types of surgery
- ECCE-Extra Capsular Cataract Extraction
- SISCS-Small Incision Suture less Cataract Surgery
- Phacoemulsification- machine assisted
Lid edema
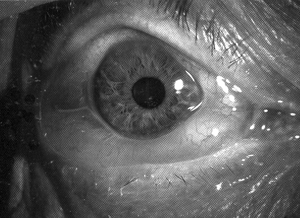
Swelling of the lid is due to injury with instruments, iritis, or allergy. It is treated with anti-inflammatory drugs, steroids. If allergy is the reason anti-histamine drugs are given (Fig. 10.1).

Chemosis
Chemosis is congestion and collection of fluid in the conjunctiva (Fig. 10.2).
Causes
- Injury to the conjunctiva with instruments during surgery
- Prolonged massage in block room
- Intraoperative sub conjunctival injection
- Allergic to eye drops such as tropicamide, Lidocaine
- Post operative Iritis and endophthalmitis.
Post Operative Complications
| Types of Surgeries | Mild | Moderate | Severe |
|---|---|---|---|
| ECCE | Lid edema, Sub Conjunctival Haemorrahge, Chemosis, Straite Keratopathy, epithelial and epithelial and epithelial and | Corneal edema, Fibrin Membrane, iritis, Hypheama, Pupillary capture, Cystoid macular edema | Hypopyon, endophthalmitis, Decemet's membrane stripping, iris prolapse, papillary block, Secondary glaucoma, shallow Anterior Chamber, broken sutures, Suture infiltration |
| SISCS | Lid edema, Sub Conjunctival Haemorrahge, Straite Keratopathy Chemosis, epithelial defect | Corneal edema, Iritis, Fibrin Membrane, hyphaema, pupillary capture, Decentered IOL, Cystoicl macular edema | Endophthalmitis, Decemet's membrane stripping, iris prolapse, papillary block, secondary glaucoma |
| PHACO | Lid edema,Chemosis, Sub Conjunctival Haemorrahge, Straite Keratopathy epithelial and endothelial damage | Corneal edema, Iritis, Fibrin Membrane, pupillary capture, Cystoid macular edema | Endophthalmitis, iris prolapse, papillary through the section, pupillary block |
Treatment
Chemosis absorbs spontaneously and some patients need anti-inflammatory drugs/analgesics incase of pain.
Sub conjunctival haemorrhage (SCH)
It is a collection of blood beneath the conjunctiva. Injury, Retrobulbar haemorrhage, Bleeding disorders, Hypertensive, Uncontrolled cough are the causes for SCH. This is also absorbed spontaneously within 2-3 weeks.
Corneal abnormalities
Corneal transparency is one of the major factor for a good vision. After cataract surgery, cornea can lose it's transparency for many reason. They are:
a. Epithelial defect
Rupture of epithelium by instruments, swabs and pad lead to epithelial defect. After retro bulbar injection eye is opened for long time which may lead to epithelial defect. Patient has the symptoms like pain, blurring vision and irritation. Discontinuation of epithelium is seen through slit lamp. Sometimes fluorescein staining is needed.
Treatment
Antibiotic ointment with pad and bandage.
b. Corneal edema
Prolonged irrigation and aspiration, trauma to endothelium, pre excisting corneal problem are causes.
Signs
- Increased IOP > 30 mm/hg
- Iritis
- Descemets membrane stripping
- Endothelial damage
Treatment
- Timolol eye drops and Tab. Diamox are given to reduce the Intraocular pressure (IOP)
- Oral glycerol / IV mannitol given for uncontrolled increase in Intraocular pressure
- Frequent use of steroids speed up recovery
- Hypertonic saline drops
- Cycloplegic eye drops twice per day and steroids 2 hourly may reduce the iritis
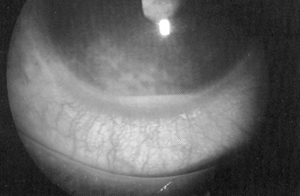
c. Striate keratopathy
It may occur on the immediate post operative day and incidence is higher if the pre-existing corneal dysfunction present. It is present as a localised stromal and epithelial edema especially seen in superior half of the cornea which indicates intraoperative trauma.
Causes
Operating trauma - trauma to endothelium by instruments, IOL, Swabs, excessive irrigation of balanced salt solution. This can be prevented by maintaining a deep Anterior chamber by using the Air bubble or visco elastic material. Tight suture is another reason for striate keratitis.
Management
In general it resolves 4 to 6 weeks after cataract surgery. As a rule if corneal periphery is clear it resolved with time. In most of the cases 0.1 % of dexametyhasone sodium resolves it. Corneal edema in periphery for over 3 months does not clear. Such patients require Penetrating Keratoplasty.
d. Detachment of descemet's membrane
Descemet's membrane is an elastic membrane and it's loosely bound with the stroma and thus allowing easy separation from stroma.
Causes
- Entry into the globe with inadequate sized incision
- Faulty instrumentation
- Fluid is injected between the decemet's membrane and Stroma
Management
- Small DM detachment is common and doesn't require active treatment.
- Wider detachment needs to be treated early. If it's diagnosed intra-operatively Air bubble should be left in the AC. This will help to holding the decemet's membrane and stroma together.
- If it is extensive then full thickness corneal suture is needed until the healing occurs.
- It can be prevented by using proper instrument and putting adequate sized incision.
e. Endothelial damage
The corneas can decompensate if large amount of endothelial cells are damaged. In endothelial damage visual prognosis is low because endothelium cannot regrow.
Causes
- Trauma with surgical instruments intra-operatively
- Constant touch by vitreous or IOL post operatively
- Pre operative inflammatory condition.
Management
- It can be prevented by maintaining deep anterior chamber as far as possible.
- Endothelial cell count should be documented for pre existing corneal problem.
- Penetrating keratoplasty may be helpful in severe cases.
Depth abnormalities
The AC may become shallow or flat in any kind of IOL surgery for many reasons. It is an absolute emergency in which treatment should be considered immediately without delay. It produces permanent damage like IOL touching the cornea and secondary glaucoma. Following conditions are the reason for the flat AC.
a. Wound leak
The main reason for the wound leak are:
- Size of the section is larger than the normal
- Loose suture or wound gap
- Inadequate and improper suturing of the wound
- External trauma after surgery even during suture removal
Management
- If wound is too large, proper resuturing and AC reformation to be done. Wound leak can be diagnosed by sidels test. Apply 2 drops of 2% fluorescein solution over the section. If wound leak is present fluorescent solution gets diluted at the site of leak. Often gentle pressure over the globe is needed to confirm the site of leak
- Cyclopent eye drop is applied with pad and bandage
- Carbonic anhydrase inhibitor and beta-blockers may decrease the aqueous out flow
- Avoiding the use of steroids enhance the spontaneous closure of wound.
b. Pupillary Block
It is an emergency condition. Pupil may be blocked with many materials such as IOL, Vitreous, cortex. Pupillary block leads to rise in IOP and produces secondary glaucoma.
Causes
- Anterior chamber intraocular lens without peripheral Iridectomy
- Vitreous touching the pupil
- Intraocular lens capture
Treatment
- Inj. Mannitol 20% and Tab. Diamox are given to reduce IOP
- YAG PI is done for ACIOL
- IOL repositioning done for IOL capture
c. Residual cortex
This is due to improper aspiration of cortex material, PXF, small pupil, pc rent where the cortex could not be removed completely. Small residual cortex usually doesn't cause problem unless they are touching the endothelium or obstructing the AC angle. Small piece of cortex will get absorbed by using steroids. Lot of cortex or cortex not getting absorbed need AC wash.
d. Hyphema
Hyphema is blood in the AC. Main source for hyphema is intraoperative injury to Iris. Other reason for hyphema are iridodialysis bleeding disorders.
Treatment
- Usually it resolves spontaneously
- Severe cases patient should be monitored carefully and given complete rest
- Apply double pad and bandage
- Recurrent bleeding with increased IOP needs hyperosmatic therapy and rarely anterior champer wash
e. Hypopyon
Pus in the AC is called hypopyon. This can be sterile or infectious (Fig. 10.3).
Causes
- Infection-It may be pre operative or post operative
- The incidence of hypopyon is high in complicated cataract, phacolytic or phacomorphic glaucoma.
Treatment
Color of the hypopyon is noted. If it is yellow if indicates an infectious stage. First AC tap should be taken to find out the organism which caused hypopyon. Cycloplegics and Antibiotics are used according to the severity.
Iritis
Inflammation of the iris is called iritis. Due to surgical trauma or using of toxic material may lead to fibrin formation. In such cases are intensively steroids and antibiotics used. Dilation helps to break the fibrin membrane (Fig. 10.4).

1. AC cells and flare
It can be recognized by slit Lamp. Cells and flare are graded Presence of cells and flare is the sign of intraocular inflammation. Steroid eye drops is used frequently depending on the severity.
Iris prolapse
After cataract surgery iris may prolapse out from the wound. Incidence of iris prolapse is more in ECCE than phaco.
Causes
- Inadequate or irregular suture.
- Size of the section is more than normal.
- Injury to the eye
- Positive pressure
Treatment
- Hourly antibiotic drops
- Repositioning and resuturing done in a less than a day did proplapse
- Excision done prolapse more than 1 day
Fibrin membrane
It appear as a dense fibrin net in the pipillary area. Prolonged irrigation with balance - salt solution and unsterile IOL are the causes for fibrin membrane formation. It gets absorbed by using antibiotic and steroids hourly. If needed oral steroids to be given.
Bullous keratopathy
This usually comes in late postoperative period. The causes are pre existing endothelial pathology, significant intraoperative endothelial damage, and chronic uveitis and in appropriate IOL design. Clinically it is present as stromal and epithelial edema. Patient may manifest blurred vision early in the morning which improves later in the day. Chronic edema causes scarring. It can be managed by drops and ointment. In some cases bandage contact lens may be fitted. PKP is done for the cases, which are not responding to other treatment.
Secondary glaucoma
Closed angle glaucoma
Causes
- Severe iritis
- Pupillary block
- Iris bombe and periphereal anterior synechiae
Treatment
- Treat the causes as for iritis
- Anti-glaucomatous drug
- Sometimes trabeculectomy may be required
Endophthalmitis
This is a vision threatening condition; delayed treatment would cause severe visual loss. Endophthalmitis can present as an acute form or chronic form. Patient has the symptoms of mild to severe pain, redness, loss of vision, floaters, photophobia. The hallmark of endophthalmitis is vitreous inflammation. Other findings are eyelid and periorbital edema, chemosis, corneal edema, AC reaction, hypopyon.
Investigations
- Vitreous culture is taken in a sterile conditon. This is to identify the type of organism which cause endophthalmitis and also we can differentiate the sterile endophthalmitis from infectious endophthalmitis.
- Ultrasound to confirm the diagnosis. It has the characteristic like RCS (Retina, choroids and sclera) Complex thickening and vitreous exudation.
Treatment
Immediate diagnosis and treatment may give better visual prognosis. Antibiotic can be given intravitreally. Intense therapy of antibiotics and steroids will help to reduce the reaction of endophthalmitis. Once the diagnosis is made, refer the patient to retina specialist without delay. Many cases require core vitrectomy.
Posterior capsular opacification (PCO)
This is a late postoperative complication in which a white membrane is formed behind the IOL. This can be managed by YAG capsulotomy.
Cystoid macular edema (CME)
This is one of the vision threatening complication, it may occur early in the late post op periods. Reason for CME after cataract surgery is still unknown. But it is believed to occur due to the increased perifovealor capillary abnormality. Intra vitreal steroids are given in the recent days. It can be diagnosed by Fundus fluorescein angiography and optical coherence tomography. The later one is preferable as it is a non-invasive procedure.

Night Duty of OA
Rules and responsibilities of night duty OA
Arrival: Night duty OA arrives at 6.00 PM or according to the hospital schedule. On entering the ward she must know the name of the Doctor posted for night duty.
Charge take over: Night duty OA has to take over the preoperative case sheets from day duty OA and collect information about complicated cases and other details.
Work description
Monitoring
Checking the preoperative case sheets regarding completion of details in the case sheet. If any investigation is not completed, it must be completed immediately.
Execution
- Self introduction to the patient
- Application of eye drops for preoperative and postoperative patients (Steroids & antibiotics accordingly)
- If any ocular or systemic complications are seen, they have to be told to the night duty doctor immediately and necessary steps taken
- In the morning of the surgery apply dilating drops to preoperative cases, and send the cases to operation theatre in batches after confirming the timing with the theatre staff.
- If any patient need to be discharged, complete the discharge rounds
Charge hand over
- While handing over to day duty OA in the morning. All the necessary details about ward cases should be conveyed.
- Post operative complications, though rare, are extremely important to recognise. The OA must notify the doctor immediately.
- Some complications require no treatment, and will not affect the outcome. However, the OA must never make any assumptions about the seriousness of the complication and must always report to the doctor.
Summary
In this unit we have covered preparation of dressings, assisting the doctors in the post operative examination, identification and management of complications and the responsibilities of night duty OA. Postoperative results are highly dependent on the accuracy and attentiveness of the OA. The OA must always have concern for the patient's doubts, fears or confusions.
Key points to remember
- Cleanliness is most important in preparing dressings and bandages
- The OA should not waste the materials
- Always be attentive to the patient's needs and concerns
- The OA is responsible for the smooth running of the postoperative check up by doctor
- The OA is to be alert to notice the potential complications in the eye of the patients and inform the doctor
- Reassure the patient that everything will be taken care of
- The night duty OA should communicate to the day duty OA, information about those who might need more observation and assessment
Student Exercise
I. Fill in the blanks
- The first step in preparing any dressings is ___________.
- Two essential figures in the ward round are _______ and ________.
- Three causes of severe pain after cataract surgery are _________ ,________ and ________.
- If the lids do not open because of severe inflammation _________ drug will be prescribed by the doctor.
- Treatment of sub conjunctival haemorrhage is _________.
Answer the questions
- What is lid edema?
- List three causes of conjunctiva chemosis
- What are the steps to be taken for wound leak?
- Describe the steps necessary in preparing eye pads.
- What are the materials needed for bandage preparation?
