Managing Emergency Conditions (Systemic)
Asthma
Asthma is a respiratory illness characterised by difficulty in breathing, wheezing and constriction in the chest. In response to a trigger, the air tubes of the lungs become narrower or completely blocked due to inflammation, thus restricting normal breathing. The condition affects the bronchi or bronchioles (airways); it does not affect the lungs' air sacs. Narrowing results, when the lining of the airways becomes inflamed and the muscles surrounding the airways contract. Asthma is one disease, but it has two main underlying components that happen deep within the airways of your lungs.
A.Inflammation: The airways of the lungs are often swollen and irritated and become more swollen and irritated when an attack begins. This swelling and irritation is known as "inflammation." Inflammation can reduce the amount of air taken in or breathed out of the lungs. In some people with asthma, the mucus glands in the airways produce excessive, thick mucus, further obstructing the airways.
B.Constriction: The muscles around the airways in the lungs squeeze together or tighten. This tightening is called bronchoconstriction. It can make it hard for breathing the air in or out of your lungs.
Inflammation and constriction together cause narrowing of the airways, which can result in wheezing, chest tightness, or shortness of breath.
The most common symptoms of asthma are
- Shortness of breath
- Wheezing
- Constriction of the chest muscles
- Coughing
- Sputum production
- Excess rapid breathing / gasping
- Rapid heart rate
- Exhaustion.
Symptoms
"Warning signs" symptoms
The appearance of asthma symptoms or their increased frequency can be early warning signs of an impending asthma attack. Some people experience a change in symptoms days in advance while others only have a few minutes notice. The most common warning symptoms are:
- An increase in wheezing or shortness of breath
- Shortness of breath or coughing after exertion or exposure to cold air
- Disturbed sleep because of coughing, wheezing, or shortness of breath
- Chest tightness or pain
- Poor response to asthma medications
- A fall in peak flow meter reading (usually the earliest warning sign)
The severity of attack symptoms can escalate rapidly. It is critical that treatment begins immediately to avoid life-threatening complications. Without prompt attention breathing can become even more labored and lead to decreasing amounts of oxygen in the blood. Blue lips or fingernails can be the first symptoms of this serious development.
Basics: types of asthma
Asthma is often put into categories or groups based on the "triggers" that cause the asthma symptoms or attacks. These categories or types of asthma are:
Allergic asthma
Allergic asthma is triggered by an allergic reaction to allergens such as pollen or pet dander. People with this type of asthma typically have a personal and/or family history of allergies (such as hay fever) and/or eczema (skin problem resulting in itching, a red rash, and sometimes small blisters).
Seasonal asthma
Trees, grass or flowers releasing pollen into the air can trigger seasonal asthma, a form of allergic asthma. For example, some people find that their asthma is worse in the spring when there is an increase in flowering plants. Others find their asthma is worse in the late summer or early fall when ragweed and mold from leaves on trees are more likely to cause problems.
Non allergic asthma
Asthma can occur in the absence of allergies also. Asthma attacks may be triggered or made worse by one or more non allergic asthma triggers including materials (irritants) in the air , such as tobacco smoke, wood smoke, room deodorizers, pine odors, fresh paint, household cleaning products, cooking odors, workplace chemicals, perfumes, and outdoor air pollution. Respiratory infections, such as the common cold, the flu, or a sinus infection may also give you symptoms. Finally, exercise, cold air, sudden changes in air temperature and even gastroesophageal reflux (heartburn) may be triggers for people with non-allergic asthma.
Exercise - induced asthma
Exercise-induced asthma (EIA) refers to asthma symptoms that are triggered only by exercise or physical activity. These symptoms are usually noticed during or shortly after exercise. Exercising outdoors in the winter seems to be particularly bad for patients with this type of asthma. Exercise can also trigger symptoms in people with other types of asthma.
Nocturnal Asthma can occur in a patient with any type of asthma. It refers to asthma symptoms that seem worse in the middle of the night.
Things that can cause asthma symptoms to get worse at night may include sinus infections or postnasal drip caused by allergens like dust mites or pet dander. The body clock may also play some role: levels of substances the body makes like adrenaline and steroids, both of which protect against asthma, are lowest between midnight and 4 AM, making it easier for people with asthma to get symptoms during these times.
Diagnosis
A device called a peak flow meter is used to diagnose asthma, and to monitor the progress of treatment. A peak flow meter measures how much, and how fast, air can be expelled from the lungs. This type of test of lung function is known as spirometry. Spirometry gives a measure of how severely breathing is affected. If measured regularly, over time, these readings can also help reveal how well or badly the asthma is being controlled.
Treatment
Inhalers: The most common way of taking treatment is with an inhaler - or "puffer" that delivers a precisely measured dose of a medicine in aerosol or fine powder form. The two main types of medicines used in inhalers are relievers and preventers.
- A reliever medicine helps to open up the airways and works rapidly. It is used at the beginning of an asthma attack. Common reliever medicines include salbutamol (Ventolin), terbutaline and ipratropium. Inhalers containing these medicines are coloured blue.
- Preventer drugs, which can be used together with relievers, are for preventing the symptoms. Most preventers are inhaled corticosteroids, usually referred to simply as steroids. They act to reduce the inflammation in the airways.
Tablets
If asthma is quite severe or unpredictable, it may be necessary to take a course of steroids in tablet form. These work in the same way as inhaled preventers, by reducing inflammation.
Nebulisers
Nebulisers make a mist of water and asthma medicine that is breathed in. They can deliver more of the drug to exactly where it's needed than conventional inhalers can. This is particularly critical in the event of a serious asthma attack.
Diabetes mellitus
The pancreas is a yellowish gray gland situated behind the stomach. It is 18cm long and weighs 60 grams. There are cells called Islets of Langerhans in the pancreas which produce endocrine secretions.
Langerhans Islets
Langerhan Islets contains three types of cells
- Alpha cell
- Beta cell
- Delta cell
Alpha cell
Glucagon is the hormone secreted by alpha cells. This promotes glycogen breakdown, thereby raising blood glucose levels.
Beta cell
These cells produce a hormone called insulin which lowers blood glucose by converting glucose to glycogen inside muscle cells. Insulin is produced when blood glucose levels are rising and glucagon when glucose levels fall in blood.
Diabetes mellitus
Diabetes mellitus is failure of the pancreas to secrete sufficient insulin to meet the body's requirements, or defective insulin action.
Two main groups of diabetes are
Type I diabetes
Type 1 diabetes involves deficiency of insulin occurring in the younger age group less than 30 years. It is due to hereditary factors or recent viral infection affecting the pancreas. These patients are thin and need life long insulin treatment, as there is no insulin secretion in their body.
Type II diabetes
This type develops in the older age group more than 40 years of age. It involves resistance to insulin action. These patients are usually overweight. They have reduced production of insulin, so treatment can be diet control, oral anti diabetic drugs and insulin only if necessary.
Symptoms of diabetes
Insulin is required for glucose to enter cells where it is utilised. When insulin is absent or defective glucose cannot enter cells it remains in the blood in high amounts. Symptoms of diabetes occur because body tissues are not able to utilise glucose.This condition is called diabetes or hyperglycemia.
1. Polyphagia
These patients have increased appetite, and eat more than usual. This is because cells are starved of glucose since glucose is not able to enter cells because of the cells' resistance to insulin. Although a diabetic person eats more, the cells do not get enough glucose.
2. Polyuria
Patient passes large volumes of urine. Normal urine does not contain glucose. In diabetics, kidneys are unable to reabsorb the excess glucose, so it appears in the urine. When glucose appears in urine, it drains a lot of water with it causing excessive urination.
3. Polydipsia
It is excessive thirst due to loss of water from the body.
4. Fatigue and weight loss
In order to obtain energy, cells start using body fat and protein for energy instead of glucose. This leads to weight loss and tiredness. Some people may not have any symptoms. They are discovered on routine urine and blood examination.
Diagnosis of type 2 (NIDDM) diabetes
- The diagnosis of diabetes is made in one of the following ways
- With classical symptoms and an unequivocally raised fasting (>= 7.8 mmol/L) or random plasma glucose level (>= 11.1 mmol/L)
- Without symptoms and 2 unequivocally raised fasting (>= 7.8 mmol/L) or random plasma glucose (>= 11.1 mmol/L) levels or
- With an oral glucose tolerance test (OGTT)
Diabetic diagnosis chart
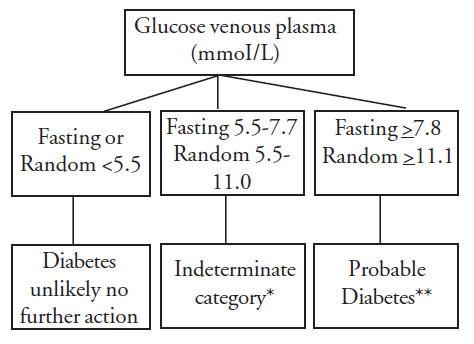
** Indeterminate category
- Assess presenting symptoms and/or signs
- Assess risk factors if considered at high risk of Type 2 diabetes or impaired glucose tolerance, proceed to oral glucose tolerance test ± periodic surveillance.
** Probable diabetes
- With suggestive symptoms, a single plasma glucose will suffice for diagnosis
- Without symptoms, 2 unequivocally raised plasma glucose values or an oral glucose tolerance test are required to establish diagnosis.
Oral glucose tolerance test (OGTT).
Indication
- If the fasting or random plasma glucose level is equivocal
- In the presence of two or more risk factors for Type 2 diabetes or impaired glucose toleranace (age -40, positive family history, overweight, hypertension, hyperlipidemia)
- In pregnant women
Procedure
- The patient should not restrict their food intake during the 3 days preceding the test.
- The patient should fast for 10-16 hours immediately before testing.
- The test should be scheduled in the morning.
- A fasting blood sample is taken, and the plasma glucose level is determined (if >= 7.8 mmol/L no need for further test).
- 75g of glucose, diluted in 250 mL of water, is given by mouth, within 5 minutes.
- After 2 hours, a second blood sample is taken, and the plasma glucose level is determined.
| The Result of the oral glucose tolerance test can be evaluated as follows (Using plasma venous sample) | |||
|---|---|---|---|
| Normal | Impaired glucose tolerance | Diabetes | |
| Fasting value | < 5.5 mmol/L | 5.5 - 7.7 mmol/L | > = 7.8 mmol/L |
| 2-hour Value | < 7.8 mmol/L | 7.8 - 11.0 mmol/L | >= 11.1 mmol/L |
Investigations
1. Urine test
Presence of glucose in urine is known as glycosuria. This can be detected by Benedict's test or strip method.
Benedict's test - method
Patient is informed that their urine specimen is required for testing urine sugar. Urine is collected in a clean bottle.
- 5ml of Benedict's solution is added to clean test tube and boiled
- 8drops of urine is added to the above solution using a dropper. This is boiled again for two minutes. If there is a colour change it indicates that sugar is present in the urine.
Green = +
Yellow = ++
Orange = +++
Brick red = ++++
2. Blood sugar
Normal blood sugar is 70-100 milligrams in fasting state and 110-140 milligrams post prandial. Fasting blood sugar of > 126mg (70m mmol/l) and post prandial (2hour) blood sugar of greater than 200mg (11.0 mmol/l) is suggestive of diabetes.
Treatment of diabetes consists of three main components
- Diet and exercise
- Oral hypoglycemic agents
- Insulin
a. Diet and exercise: It is the corner stone of diabetic management.
Sugar containing items are to be avoided. Balanced food within permitted calorie limits as prescribed by the doctor is taken.
Exercise helps in glucose utilisation and maintaining ideal weight.
b. Oral hypoglycemic drugs
They are categorized into the following groups:
- Sulphonyl urea - consist of drugs like Glibenclamide (Dasmil)
- Biguanides - Met formin
- 2 Glucoxidase inhibitors
- Glietezones
Drugs are started according to advice of family physician mainly use in Type II diabetes.
c. Insulin
Insulin is used in type I diabetes life long and in type II diabetics when blood sugar is not well controlled. Insulin has to be given only by injection continuously.
Types of insulin
- Short acting
- Intermediate acting
- Long acting
1. Short acting insulin (Plain insulin)
Duration of action is from 2 hours to 8 hours usually given 2-3 times per day.
2. Intermediate acting (NPH)
In this type of insulin action starts after 4 hours, effective for 24 hours.
3. Long acting (PZI)
Effective for 24-36 hours. Once daily dose is enough.
Complications of diabetes
- Acute complications
- Chronic complications
Acute complications
1. Diabetic ketoacidosis
It is a medical emergency which occurs in
- Infection or stress which increases insulin requirements.
- Patients not on treatment
- First time diabetic, previously undiagnosed.
Here blood sugar levels are very high (200-600mgms) due to lack of insulin. Glucose is not available for metabolic energy; instead fats are used by the body for energy. During fat metabolism, toxic products called ketones are formed, which gives rise to ketoacidosis.
Signs and symptoms
- Gradual onset
- Patient may be febrile
- Vomiting, abdominal pain
- Dry inelastic skin
- Low blood pressure and rapid pulse
- Deep sighing respiration
- Breath smells of acetone (sweat, sickly smell)
- Loss of consciousness
- Diagnosis is made by blood sugar estimation and presence of ketones in urine.
Treatment
I.V fluids are immediately started since patient is dehydrated. A large volume of about 6 litres is given rapidly. Normal saline or Ringer Lactate is given.
Short acting plain insulin is given hourly according to blood sugar level. Insulin is given intravenously in this condition. Insulin is given hourly until the smell of acetone is absent and blood sugar is less than 200 mg.
Serum electrolytes are estimated and potassium chloride and sodium bicarbonate given accordingly.Antibiotics are started if signs of infection are present.
Patient may be catheterised to check hourly urine sugar and acetone. Fluid balance chart - Intake and output of fluid should be accurately recorded. When the patient is conscious, oral fluids are allowed.
Hypoglycemia
Occurs when blood sugar is low, less than 60 mg. Occurs in the following situations.
- Too much insulin
- When food is missed
- Increase in exercise
Signs and symptoms
- Sweating - skin is warm and moist
- Pallor
- Weakness / dizziness
- Palpitation
- Loss of consciousness
Diagnosis is made by low blood sugar level
Treatment has to be immediate since brain cells can have irreversible death if glucose level is not immediately corrected.
When patient is conscious fluids with sugar or glucose can be given
- Intravenous glucose - 25% dextrose 50ml is given in severe cases. This is followed by 5% dextrose fluid for few hours.
- Glucagon injection 1ml is given if patient is unconscious
Points to differentiate between hypoglycemia and hyperglycemia
| Clinical features | Hyperglycemia | Hypoglycemia |
|---|---|---|
| Onset | Gradual | Sudden |
| Skin | Dry and cold | Warm & moist |
| Pulse | Faint and fast | Normal |
| Blood Pressure | Low | Normal |
| Breathing pattern | Deep and sighing | Normal |
| Breath smell | Acetone odour | Normal |
| Blood sugar | High | Low |
| Treatment | I.V. fluids, insulin | I.V. glucose |
Long term complications
Occur when diabetes is poorly controlled
1. Ocular
Diabetes affects the eyes causing cataract, diabetic retinopathy, retinal detachment and glaucoma. Permanent visual loss can occur due to above complications.
A Diabetic is prone to get any kind of infection more easily than a normal person. Also the infection takes longer to clear up. Diabetes affects the eye in many ways. In the eye, as well as the rest of the body, diabetes reduces the healing capabilities. Corneal abrasions take much longer than normal to heal. When blood sugar rises dramatically, the lenses within the eyes begin to swell.
This will cause a change in the eyeglass prescription. When the blood sugar returns to normal levels, the lenses return to their normal shape. With progression of diabetes, there is a decrease in oxygen supplied to various tissues in the body. Those tissues that metabolise, or reproduce faster than others require more oxygen and therefore will be more susceptible to diabetes. These tissues associated with progressive diabetic changes are referred to as the three "opathies". These are neuropathy (damage to nerves), nephropathy (damage to the kidneys), and retinopathy (damage to the retina).
Since the cells of the retina are constantly utilised by light, they are constantly metabolising waste products that need to be removed. This requires plenty of oxygen. If there isn't enough oxygen, these tissues become starved and emit a "vasoproliferative substance". This substance acts like a signal to the body that there is an area that requires more oxygen. The body reacts by growing new, abnormal vessels into the area, a process referred to as neovascularization. These blood vessels can be very damaging to the vision.
To stop these vessels from proliferating, doctors must stop the release of the vasoproliferative substance. This is acheived by lasering the retina that is producing it. Unfortunately, the damaged retina is no longer functional. Even if a patient is newly diagnosed and has no symptoms of diabetes, they still require a thorough baseline exam to which future exam results can be compared.
2. Renal
Long duration of poorly controlled diabetes leads to proteniuria and renal failure.
3. Heart
Increase in incidence of heart attacks occurs. These people can have " silent heart attack " without any pain since nerves become insensitive to pain.
4. Brain
Stroke occurs more frequently in diabetics.
5. Nerves
Commonly affects peripheral nerves. Tringling occurs in fingers and toes, reflexes may disappear. Painless ulcers can occur in skin.
6. Feet
Poor circulation and peripheral neuropathy causes infection or injury to feet, leading to gangrene and loss of foot. Diabetics need to take special care of their feet.
Complications associated with type 2 diabetes
- Ischaemic heart disease
- Peripheral vascular disease
- Hypertension
- Hyperlipidaemia
- Chronic foot ulcers which needs amputation
- Polyneuropathy
- Autonomic neuropathy
- Reduced visual acuity
- Clinical nephropathy
- Urinary tract infections
Evidence is mounting that if Type 2 diabetes is recognised earlier and treated more effectively, the progression of complications can be slowed and the morbidity and mortality associated with this condition could be reduced.
Early and more effective treatment can be achieved through early diagnosis namely, screening by measuring blood glucose levels in patients at risk, or those presenting with symptoms associated with diabetes.
Prevalence
- It has been estimated that the overall prevalence of Type 2 diabetes in caucasian populations is approximately 2%. However, the prevalence of Type 2 diabetes increases with age:
- 4% of the population above 60 years of age
- 10% of the population above 70 years of age.
Furthermore, it has been estimated that approximately another 2% of the total population currently have undiagnosed Type 2 diabetes.
Clinical management guidelines: Blood glucose
Background: The occurrence and progression of microvascular complications can be reduced by improved blood glucose control.
Aim: To achieve blood glucose control as near to normal as possible without producing unacceptable hypoglycemia.
Procedure
Measure HbA1c
If unavailable measure fructosamine. (If unavailable measure fasting / 2 h postprandial blood glucose.)
Frequency of measurement
- Every 3-6 months for insulin-treated patients.
- Every 6-12 months for non-insulin treated patients.
Interpretation of results
| Parameter | Goal | Needs Improvement |
|---|---|---|
| HbA1c (%) | Normal | > 2% above normal |
| Fructosamine (µmol/L) | Normal | > 360 |
| Fasting Plasma Glucose (mmol/L) | 4.0 - 5.5 | >= 7.8 |
| 2h Postprandial Plasma Glucose (mmol/L) | < 7.8 | >= 11.1 |
What to do if blood glucose is not controlled?
- Explore reasons for unsatisfactory control.
- Review treatment.
- Consider referral to diabetes educator.
- Consider referral to dietitian.
Consider referral to Diabetologist/Diabetes Clinic. Adjust medication and consider insulin if on maximum doses of oral agents.
Clinical management guidelines: weight
Background: Weights above a Body Mass Index (BMI) of 28 for men and 27 for women is associated with excessive cardiovascular mortality. Target weights should aim to achieve a lower BMI than these levels.
Aim: To reduce weight to lower BMI below the above critical levels.
Procedure
Measure height and weight of patient at initial visit and calculate BMI (Weight(kg) / Height(m).
Refer to the Table to determine the maximum weight which will achieve the target BMI.
Weight to achieve the target Bmi
| Height (cm) | Men Weight (kg) | Women Weight (kg) |
|---|---|---|
| 150 | 63 | 61 |
| 155 | 67 | 65 |
| 160 | 72 | 70 |
| 165 | 76 | 73 |
| 170 | 81 | 78 |
| 175 | 86 | 83 |
| 180 | 91 | 88 |
What to do if weight is not controlled?
- Refer to dietitian or provide basic dietary advice.
- Advise about exercise program.
Clinical management guidelines: Retinopathy
- Background: Retinopathy is common and prevalence increases with increasing duration of diabetes.
- Up to 20% of people with NIDDM have retinopathy at the time of diagnosis.
- Visual impairment is rare in the early stages and should not be used as an indicator of retinopathy. Normal visual acuity does not exclude significant retinopathy.
Aim: To identify individuals who require referral to an ophthalmologist for treatment and/or further assessment.
Procedure
- Check visual acuity with Snellen chart - correct with pinhole if indicated.
- Dilate pupils.
- Examine fundi
What to do if not controlled?
- Refer to ophthalmologist:
- If visual acuity is < 6/6 in either eye at initial examination.
- If declining visual acuity at subsequent visits.
- If any retinal abnormalities detected.
- If unable to get a clear view of the retina.
- Once in 2 years.
Clinical management guidelines: diabetic nephropathy
Background
- Incipient nephropathy can be detected by urine testing for microalbumin. Microalbuminuria is a strong predictor of macrovascular disease in Type 2 diabetes and such patients require careful assessment and follow up.
Aim: To identify and treat individuals with micro albuminuria in order to reduce the number progressing to overt nephropathy.
Procedure: Test for microalbumin in urine sample, either timed collection or first morning sample.
How often: At diagnosis and then annually.
Interpretation of Result
| Albumin (µg/min) | Albumin : Creatinine Ratio | |
| Normal | < 20 | Male 0 - 2.5 , Female 0 - 3.5 |
| Microalbuminuria | 20 - 200 | Male 2.6 - 30, Female 3.6 - 30 |
| Macroalbuminuria | > 200 > | 30 |
What to do if micro albuminuria and hypertension are present
- Review blood pressure and treat with a pharmacological agent to control blood pressure as outlined in the guidelines on blood pressure.
- Consider referral to a physician experienced in the care of diabetic renal disease.
If microalbuminuria only is present
- Review diabetes control and improve if necessary.
- Treat with a pharmacological agent
(Recommended first line of therapy: ACE Inhibitor.
If adverse effects develop, treat with calcium channel blockers).
If macroalbuminuria is present: refer to a physician experienced in the care of diabetic renal disease.
Clinical management guidelines: lipids
Background: The occurrence of macrovascular complications is influenced by lipid abnormalities.
Aim: To normalise lipid levels.
Procedure
- Measure lipids including total cholesterol, triglycerides, HDL cholesterol. Frequency of measurement
If lipids are normal - every12 months
If lipids are abnormal - every 3-6 months
Interpretation of results
| Parameter | Goal | Needs Improvement | Action Recommended |
|---|---|---|---|
| Total Cholesterol (mmol/L) | < 5.5 | 5.5 - 6.5 | > 6.5 |
| Triglycerides [mmol/L] | < 2.0 | 2.0 - 4.0 | > 4.0 |
| HDL Cholesterol [mmol/L] | > 1.0 | - | < 1.0 |
What to do if symptoms are not controlled?
- Non-pharmacological interventions initially including,
- Improve blood glucose control
- Reduce saturated fat intake
- Regular moderate exercise
- Weight control if indicated
- Reduce alcohol intake if triglycerides elevated
- Consider referral to dietitian
- If the above interventions are unsuccessful after 6 months, consider pharmacological therapy.
Points to remember
- People in their 50s getting recurrent stye should get their blood sugar checked for diabetes.
- The risk of blindness in diabetics is 25 times greater than the normal population.
- Frequent fluctuations in blood sugars leads to earlier development of cataract.
- Diabetics are more likely to develop inflammation of the eye after any surgery, esp. cataract surgery.
- Diabetics develop changes in the retina, called Diabetic Retinopathy (DMR).
- Optic Neuritis, an inflammation of the optic nerve can occur.
- The elderly diabetics may discover a 'crooked face' or inability to close one eye. This is due to a nerve palsy. Due to paralysis of one or more nerves, the muscles are affected, leading to disability. Consult the doctor, don't worry, most recover with time.
Hypertension
Background
- Hypertension is a recognised risk factor for microvascular and macrovascular complications of diabetes.
Aim
- To identify individuals with elevated blood pressure and to reduce blood pressure see the below the following target levels:
1. In non-pregnant diabetic patients aged 18-40 years
- Systolic > = 140 mmhg and diastolic < = 90 mmhg
2. In diabetic patients aged > 60 years
- Systolic <= 160 mmhg and diastolic < = 90 mmhg
Procedure
- Measure blood pressure after a minimum of 5 minutes sitting. Record diastolic at the disappearance of sounds (phase 5).
How often:
- Every clinical visit
Interpretation of results
| Category | Age (Years) | Systolic BP (mm Hg) | Diastolic BP (mm Hg) |
| Normal | 18 - 40 | < = 140 | < = 90 |
| > 60 | < = 160 | < = 90 | |
| Hypertension | 18 - 40 | > 140 | > 90 |
| > 60 | > 160 | > 90 | |
| Systolic Hypertension | 18 - 60 | > 140 | < = 90 |
| > 60 | > 160 | < = 90 |
What to do if blood pressure is not controlled?
- All patients should receive non-pharmacological interventions including
- Weight control
- Regular moderate exercise
- Reduced salt consumption
- Reduced alcohol consumption
- Cessation of smoking
- If pharmacological intervention is required, ACE inhibitors and calcium channel blockers are the preferred agents for treating hypertension in people with diabetes (unless contraindicated).
Cardiac arrest
I. Resuscitation
Cardiac arrest is the sudden failure of the heart to supply adequate blood circulation. It occurs in two forms - asystole, when there are no contractions of the myocardium at all and ventricular fibrillation, when the contraction of the myocardium is uncoordinated and ineffective. Effective circulation must be restored within three minutes to prevent irreversible brain damage.
The most common causes of cardiac arrest are
- Myocardial infarction
- Anaesthesia over dosage
- Electrolyte imbalance
- Drowning
- Electrocution
- Shock
The OA must know
- How to diagnose cardiac arrest
- How to summon the emergency team
- How to initiate resuscitation effectively
- Where to find the necessary equipment
Signs of cardiac arrest are
- Unconscious patients without pulse, low or unrecordable blood pressure, absent respiratory movements.
- Cyanosis
- Cessation of heart beat
- Dilated pupils - (not a reliable sign in ophthalmology due to use of dilating agents)
Management
Upon discovering a collapsed patient the OA must act quickly and calmly. Initially she should try to rouse the patient by shaking them carefully and calling out their name. The OA must remember that the patient who has fainted has a palpable pulse.
If the patient is unresponsive the OA should then shout for help- alert a colleague to summon medical aid and bring the resuscitation trolley/ECG machine and defibrillator. On no account OA must leave the patient to look for help. It should only take a matter of seconds for the OA to diagnose cardiac arrest. A useful aid to remember in emergency is ABC.
A - Airway
B - Breathing
C - Circulation
The OA should open the airway to see if it is clear. This is done by the combined maneuver of head tilt and chin lift. Any obvious obstruction should be removed from the mouth. To establish if the patient is breathing the OA should observe the patients chest to see if there is any movement or listen for breath sounds and feel for exhaled air on the back of her hand.
If the patient is not breathing, mouth to mouth or nose breathing should be commenced by the OA. Initially, two slow full breaths should be given, each sufficient to cause the chest to rise. The chest should be allowed to fall between inflations. When a colleague arrives with the resuscitation trolley, an oral airway should be inserted and a bag and mask (ambu bag) used to ventilate the patient. Before proceeding to this step, the OA should establish if the patient has circulation by checking the carotid pulse. The pulse should be palpated for at least five seconds to find whether the circulation has stopped.
If the pulse is absent cardiac compression should be commenced.
Before doing so, it is important to ensure that the patient is lying on their back on a firm surface. Kneeling by the side of the patient, the nurse should locate the base of the heart. The position of the hands should be two fingers breadth above this point.
The ribs are depressed forcefully and rythmically by about 3-5cm, 60-80 times per minute in an adult. The arms should be kept straight when performing cardiac massage. It is important not to compress too quickly since the ventricles will not have enough time to refill with blood. Some find it helpful to establish the rhythm by saying one-one thousand, two-one thousand, and three-one thousand. The hands must be carefully positioned and should not lose contact with the point of compression.
If too low, pressure on the xiphoid process may cause internal injury. The fingers should be raised; pressure by the fingers or the hand on the ribs may cause rib fractures.
If there are two OAs, one should carry out cardiac compression while the other delivers one breath after every fifth compression. If there is only one OA the compression to ventilation ratio is 15:2. The OA should check for the return of the pulse and breathing after one minute and thereafter every three minutes. If pulse and breathing are still absent, she should continue resuscitation until medical help arrives.
On arrival of medical help
To be of maximum help to the doctor, the OA should be familiar with the location and use of equipment and drugs on the emergency trolley. ECG electrodes will be required and applied at once to record heart rate and rhythm. The patient should be intubated immediately, ideally by an anaesthetist. If no anaesthetist is available, the attending doctor will have to intubate the patient himself and delegate a nurse to ventilate the lungs via an ambu bag connected to a continuous supply of oxygen. The doctor must set up an intravenous infusion as soon as possible in order to administer I.V. drugs.
If the patient is in ventricular fibrillation, this can be corrected by electrical fibrillation. The defibrillator machine delivers electrical shock to the heart muscle which stops the chaotic electrical activity and allows normal electrical conduction and normal heart rhythm to return. The doctor applies electrode jelly to the paddles to prevent skin burns. These are placed at the right upper chest and the left axilla so that the electric current will pass across the chest through the cardiac muscle. To avoid getting a shock, everyone must stand well clear of the bed when the defibrillator is operated. If defibrillation is unsuccessful the doctor has to give the patient I.V. adrenaline 1mg, followed by I.V. lignocaine.
If the patient is in asystole, there is no electrical activity and the ECG shows a straight line. Defibrillation will have no effect whatsoever because there is no electrical output from the heart. The doctor has to give the patient I.V. adrenaline 1mg followed by I.V. atropine 2mg.
Post resuscitation care
The patient's airway, breathing, circulation and blood pressure are assessed. The doctor should arrange for the patient to be transferred to an intensive care unit where he can be observed, monitored and treated (arterial blood gases and electrolytes should be taken by the doctor).
Notes about drugs in the emergency drug box
1. Adrenaline
This increases the heart rate and increases the force of cardiac contraction. It is supplied in 1ml ampoules of 1/10,000. Dosage is initially 1ml until an effect is obtained.
2. Isoprenaline
This primarily increases heart rate but also increases the force of cardiac contraction.It is supplied in 2ml ampoules of 50mg per ml.
3. Atropine
This increases the heart rate. It is supplied in 1ml ampoules of 600mg per ml.
4. Calcium chloride
This increases temporarily the force of cardiac contraction and will reduce the effect of dangerously high blood potassium. It is supplied in 10ml ampoules of 10% calcium chloride.
5. Lignocaine
This is local anaesthetic that acts on the heart to reduce electrical excitablility (It suppresses ectopic and the likehood of ventricular tachycardia or fibrillation) and is supplied as 10ml ampoules of 10mg per ml.
6. Aminophylline
This causes bronchodilatation and therefore relieves bronchospasm. It is supplied in 10ml ampules of 250mg/ml.
7. Hydrocortisone
This is an anti-inflammatory steroid used in anaphylactic shock. It suppresses tissue oedema and is supplied in 1ml ampules of 100mg.
8. Naloxone
This reverses the depressant and analgesic effect of opiate narcotics. Supplied in 1ml ampules of 400mg.
Very important
When you take a drug for use from the box, read the label to be sure it is the drug you have been asked for.
Shock
The supply of oxygen to the tissues is essential in the maintenance of life; this can only be ensured when the circulatory system is functioning normally. Sudden collapse of the circulation known as shock is one of the common and formidable conditions in clinical practice.
Clinical causes
- Haemorrhage
- Severe wounds
- Severe burns
- Multiple fractures
- Pulmonary embolism
- Myocardial infarction (heart attack)
- Severe infection
- Severe allergic reaction
Signs and Symptoms
Varies with type of shock
- Apprehension, light headedness
- Generalized itching
- Swelling of eyelids, lip, tongue, hands, feet.
- Skin colour pale and grey, slow capillary refill of nail beds.
- Cool, moist skin
- Weak, rapid pulse
- Fast, shallow breathing
- Low blood pressure
Types of shock
- Hypovolemic - blood or plasma is lost from circulation to exterior of the body or into the tissues. Also may be due to dehydration.
- Cardiogenic - failure of pumping action by the heart causing inadequate circulating blood volume.
- Vasogenic or low resistance shock - widespread vasodilation causing increased capacity of circulation. Existing blood volume, even if it is normal, becomes inadequate.
Septic - caused by overwhelming infection
Anaphylactic - severe allergic reaction produced by the injection of a protein to which a person is sensitive, e.g penicillin, anaesthetic agent.
Neurogenic - loss of sympathetic control (nervous system), can result from spinal anaesthesia.
Treatment
- The patient should be laid flat, preferably in the head down position. This helps supply more blood to the brain.
- Depending on the type of shock the volume of circulating blood should be increased as quickly as possible, by setting up intravenous infusion.
- Venous blood should be taken for grouping and cross matching in severe cases of hypovolemic shock.
- Fluids to be administered ringer lactate or 0.9 normal saline in to be instituted until medical help arrives.
- Injection adrenaline 1 amp subcutaneous is the drug of choice in anaphylactic shock.
Summary
The major systemic complications of asthma, diabetes, hypertension, cardiac arrest and shock have been described. Management by OA of the above is described. Majority of patients coming to eye hospital may not have these complications. But OA must have this knowledge.
Key points to remember
- Asthma can be chronic or acute
- Medications are available to treat asthmatic attacks
- Diabetes is common in eye hospital patients
- OA should have a thorough knowledge of symptoms and treatment
- Hypertension may lead to serious complications in the eye and the whole body
- Hypertension must be constantly monitored and controlled
- Cardiac arrest is a life threatening condition
- Resuscitation must be started immediately
- Shock has many causes
Student exercise
Say True/ False
- Asthma can only be chronic.
- No medication is available to treat asthmatic attacks.
- Diabetes is common in the eye hospital patients.
- Hypertension must be monitored occasionally.
- Cardiac arrest is not a life threatening condition.
Answer the following
- Why should OA be concerned about surgical patients with asthma?
- Why it is necessary to check blood sugar for diabetic patients?
- List the steps to be taken upon finding a collapsed patient.
- List three causes of shock.
- List three medications in the emergency drug box and their uses.
