Basic Refraction
Basic refraction is carried out to evaluate the visual acuity of the patient's eyes visual acuity is dealt in detail in Chapter 2.
Types of Refractive Errors and their Management
In perfect vision, the image is focused onto the retina, just as a camera has to be focused properly in order to take a clear picture. If the image is not focused exactly on the retina, the image will be blurred, just like an out-of-focus photograph. In this case, the person is said to have a refractive error.
1. Myopia/short-sightedness
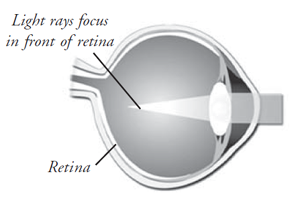
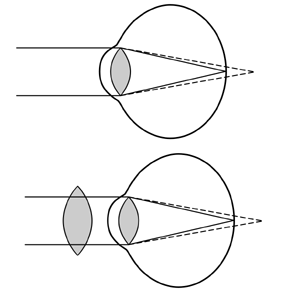
Near-sightedness is an error of visual focusing that makes distant objects appear blurred. It is also called myopia or short-sightedness (Fig.3.1).
Causes, incidence and risk factors
A near-sighted person sees near objects clearly, while objects in the distance are blurred. As a result, someone with myopia tends to squeeze the eye lids when viewing far away objects. A near-sighted person can easily read the Jaeger eye chart (the chart for near reading), but finds the Snellen eye chart (the chart for distance) difficult to read. Blurred vision results when the image is focused in front of the retina, rather than directly on it. A normal eye's lens and cornea focus light on the retina. In a myopic eye the light is focused in front of the retina and so the image is blurred
Myopia occurs when the physical length of the eye is greater than the optical length. Near-sightedness often increases in the rapidly growing school-aged child or teenager, and progresses during the growth years, requiring frequent changes in glasses or contact lenses. It usually stops progressing as growth is completed in the early twenties.
Clinical types of myopia
Near-sightedness affects males and females equally, and those with a family history of near-sightedness are more likely to develop it. Most eyes with near-sightedness are entirely healthy, but a small number of people with myopia develop a form of retinal degeneration. Early diagnosis of near-sightedness is important, since a person can suffer socially and educationally by not being able to see well at a distance.
Myopia can present itself in three categories
- Congenital myopia: This is present at birth and may be unilateral or bilateral. Bilateral congenital myopia may be associated with squinting (strabismus).
- Simple myopia: This type of myopia is not associated with any degenerative changes in the eye. It is the most common type of myopia. The power of glasses increases usually during the years of study in school and college and then remains steady.
- Pathological myopia: This type of myopia rapidly progresses and there are degenerative changes in the retina.
Symptoms of myopia
- Blurred vision or squeezing the eyelids when trying to see distant objects. (Children often cannot read the blackboard, but easily read a book). Near-sighted people tend to go near the objects to see them.
- Eye strain
- Headaches (uncommon)
Signs that may indicate myopia
- Sitting close to television
- Holding books very close when reading
- Having difficulty seeing the blackboard in school, or a wall menu in a Restaurant, place names in the bus
Relevant tests
- Visual Acuity test, both for distance (Snellen), and near (Jaeger)
- Refraction test to accurately determine the refractive error.
- Colour vision test to exclude colour blindness
- Muscle balance test
- Slit lamp examination of the eyes
- Measurement of the pressure of the eyes
- Retinal examination
Treatment
Properly prescribed spectacles (minus lenses) or contact lenses will enable the person to see clearly. The lens diverts the incoming light rays, so that they are correctly focused on the retina.
There are also a number of techniques available for reshaping the cornea (the front surface of the eye), in order to reduce its power and thus correct myopia. One technique (known as orthokeratology or "Ortho-K") uses rigid contact lenses to change the shape of the cornea. Other techniques use surgery to remove tissue from the cornea, leaving it with a flatter surface. Near-sightedness is easily corrected by eyeglasses or contact lenses, which shift the focus of the image on the retina.
Radial keratotomy is a surgical procedure popular recently. It has been almost completely replaced by LASIK, in which an excimer laser is used to reshape the cornea.
Complications
- Complication associated with the use of contact lenses: possible corneal ulcers
- Complications in laser vision correction are uncommon, but can be serious
- People with myopia may develop retinal detachments or retinal degeneration
- If a person with near-sightedness has flashing of lights, floating spots, or a sudden loss of any part of the field of vision, it may indicate a retinal detachment.
2. Hypermetropia / far-sightedness
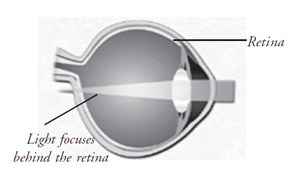
In far-sightedness, there is difficulty in seeing objects which are nearby. It is the result of the visual image being focused behind the retina rather than directly on it. It may be caused by the eyeball being short or the focusing power being too weak.
Far-sightedness is often present from birth, but children can often tolerate moderate amounts without difficulty, and most outgrow the condition. As aging occurs, glasses or contact lenses may be required to correct the vision. A family history of far-sightedness is a risk factor.
Clinical types of hypermetropia
- Simple or developmental hypermetropia: This is the most common type, and exists from birth. As the baby ages, the eyeball grows in size and the hypermetropia gradually diminishes (Fig. 3.2). If the growth of the eye is retarded however, the hypermetropia persists.
- Acquired hypermetropia: This is found in aphakia, a condition common following extraction of the lens for cataract. This hypermetropia is usually high. (+10.00)
Effects of accommodations on hypermetropia
Accommodation has considerable influence on hypermetropia as this error may be fully or partly corrected by accommodation. Depending on accommodation, several types of hypermetropia are described (Fig. 3.3).
Total hypermetropia : This is the type of hypermetropia which is elicited after complete paralysis of accommodation, (as after application of Atropine) we can detect the strongest glass with which maximum visual acuity can be obtained. This is total hypermetropia.
Latent hypermetropia : This is the amount of hypermetropia which is corrected by the normal tone of the ciliary muscle. It is more in young children than in elderly persons, as the tone of the ciliary muscle is much stronger in the young than in adults.
Manifest hypermetropia: This is the hypermetropia which remains uncorrected in normal circumstances, that is when accommodation is not being actively exerted (Fig 3.4). This may be divided into two
- Facultative (that part of accommodation which can be overcome by active exertion of accommodation)
- Absolute (that part of accommodation which cannot be overcome by the exertion of accommodation)
Complications
Hypermetropia can be a risk factor for glaucoma
Treatment
Far-sightedness is easily corrected with glasses or contact lenses. Surgical techniques are available for correcting far-sightedness and can be used for those who do not wish to wear glasses or contacts. (Fig.3.4)
3. Astigmatism
Astigmatism is a focusing error which causes asymmetric blur. Some directions in an image are more out of focus than others. This can be contrasted with short - sightedness (myopia) where all directions are uniformly blurred.
In astigmatism the cornea is oval. Most astigmatic corneas have two curves - a steeper curve and a flatter curve. This causes light to focus on more than one point in the eye, resulting in blurred vision at distance or near. Astigmatism often occurs along with myopia or hypermetropia or far-sightedness.
Astigmatism causes different amounts of blur in different directions. It causes images to appear distorted, or sometimes even double. Certain letters may be more difficult to read than others, depending on the orientation of the lines within them.
Causes of astigmatism
Most Astigmatism is caused by the shape of the front surface of the eye (the cornea). It can also be caused by slight tilting of the lens inside the eye. It may be an inherited characteristic or a normal variation accompanying growth.
Objects at all distances are indistinct or blurred and the eye cannot focus. Even slight degrees of astigmatism may encourage headaches and fatigue, and reduce concentration. (The eyes try, without success, to correct the blur. There is a tendency to squint to see better, producing discomfort in the muscles of the eyelids and face needs correction)
Types of astigmatism
- Regular astigmatism : When the refractive power changes uniformly from one meridian to the other.
- Irregular astigmatism : When the refractive power changes irregularly in different meridians as seen in corneal facets.
Regular astigmatism may be of three types
Simple astigmatism: One focal line falls on the retina and the other falls either in front of or behind the retina, when the eye is at rest. When one focal line falls in front of the retina the other line is formed on the retina, the condition is known as simple myopic astigmatism. Similarly, in simple hypermetropic astigmatism one line is formed behind the retina and the other on the retina.
Compound astigmatism: Both the focal lines are formed either in front of the retina when it is called compound myopic astigmatism or behind the retina, when it is called compound hypermetropic astigmatism (Fig. 3.5).
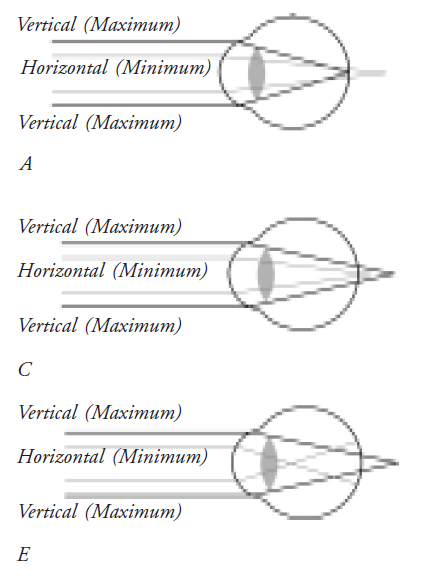
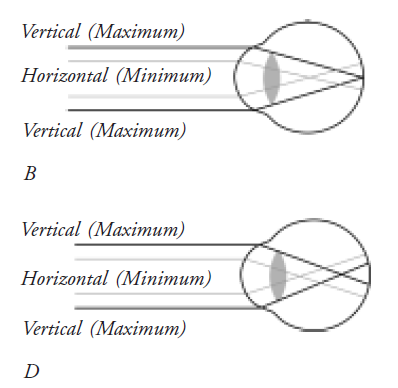
Mixed astigmatism: One of the focal lines is formed in front of the retina and the other behind the retina.
Symptoms of astigmatism
- Diminished visual acuity
- Headache
Astigmatism can be detected and measured with corneal topography, keratometry, vision testing, and refraction.
Treatment
- In regular astigmatism the error can be corrected by suitable cylindrical lens, the exact power being determined by retinoscopy
- In case of irregular astigmatism, contact lenses have to be used
Astigmatism correction
Cylindrical lenses in spectacles or contact lenses can be used to correct astigmatism. Sometimes correction of astigmatism can cause change in the apparent size and shape of objects, and it may affect the patient's judgment of distance. A patient may see taller or shorter, or walls may appear to slope and floors curve.
In most cases, adjustment to these side effects takes only a week or so. Astigmatism correction may involve a compromise between optimal clarity and visual discomfort.
4. Presbyopia
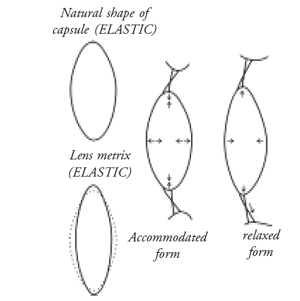
Presbyopia is an age-associated progressive loss of the focusing power of the lens. This results in difficulty seeing objects close-up.
The focusing power of the eye, which depends upon the inherent elasticity of the lens, is gradually lost as people age. This results in a slow decrease in the ability of the eye to focus on objects nearby.
People usually notice the condition around the age of 40, when they need to hold reading materials further away in order to focus. Presbyopia is a natural part of the aging process and affects everyone.
Symptoms
- Decreased focusing ability for near objects
- Eyestrain
- Headache
A general eye examination will be performed, including measurements to determine a prescription for glasses or contact lenses.
Relevant tests
- Visual acuity test
- Refraction test
- Muscle balance test
- Slit lamp examination
- Retinal examination
Treatment
Presbyopia can be corrected with glasses or contact lenses. In some cases, the addition of bifocals to an existing prescription is sufficient. As the ability to focus close-up worsens, the prescription needs to be changed accordingly. Around the age of 65, the eyes have usually lost most of the elasticity needed to focus close up. However, it will still be possible to read with the help of the appropriate prescription. Even so, it may be necessary to hold reading materials further away, and larger print and more light become necessary. People who do not need glasses for distance vision may only need half glasses or reading glasses.
With the use of contact lenses, some people choose to correct one eye for near and one eye for far. This is called monovision and eliminates the need for bifocals or reading glasses, but can interfere with depth perception.
New surgical procedures can also provide solutions for those who do not want to wear glasses or contact lenses.
Ocular motility and strabismus
Anatomy of the extraocular muscles
There are six extraocular muscles which rotate the eye about its vertical, horizontal, and antero-posterior axes: the Medial Rectus (MR), the Lateral Rectus (LR), the Superior Rectus (SR), the Inferior Rectus (IR), the Superior Oblique (SO), and the Inferior Oblique (IO).
Muscle movements
A given extraocular muscle moves an eye in a specific manner, as follows:
- MR - moves the eye toward the nose
- LR - moves the eye away from the nose
- SR - primarily moves the eye upward and secondarily rotates the top of the eye toward the nose
- IR - primarily moves the eye downward and secondarily rotates the top of the eye away from the nose
- SO - primarily rotates the top of the eye toward the nose and secondarily moves the eye downward
- IO - primarily rotates the top of the eye away from the nose and secondarily moves the eye upward
The primary muscle that moves an eye in a given direction is known as the "agonist." A muscle in the same eye that moves the eye in the same direction as the agonist is known as a "synergist", while the muscle in the same eye that moves the eye in the opposite direction of the agonist is the "antagonist". According to Sherrington's law, increased innervation to any agonist muscle is accompanied by a corresponding decrease in innervation to its antagonist muscle(s).
Muscle innervations
Each extraocular muscle is innervated by a specific Cranial Nerve (CN)
- MR - cranial nerve III
- LR - cranial nerve VI
- SR - cranial nerve III
- IR - cranial nerve III
- SO - cranial nerve IV
- IO - cranial nerve III
The following can be used to remember the cranial nerve innervations of the six extraocular muscles: LR6(SO4)3:
That is, the LR is innervated by CN6, the SO is innervated by CN4, and the remaining muscles (MR, SR, IR, and IO) are innervated by CN3.
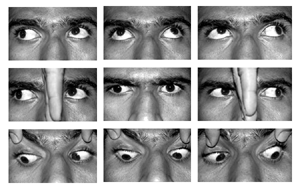
Cardinal positions of gaze
These are six positions of gaze which allow comparisons of the horizontal, vertical, and diagonal ocular movements produced by the six extraocular muscles. These are called the six cardinal positions:
- up/right
- right
- down/right
- down/left
- left
- up/left
In each position of gaze, one muscle of each eye is the primary mover of that eye and is yoked to the primary mover of the other eye. Below, each of the six cardinal positions of gaze is shown, along with upward gaze, downward gaze, and convergence. (Fig. 3.6)
Strabismus (heterotropia)
Normally, when viewing an object, the "lines of sight" of both eyes intersect at the object; that is, both eyes point directly at the object being viewed. An image of the object is focused upon the macula of each eye, and the brain merges the two retinal images into one. Sometimes, however, due to some type of extraocular muscle imbalance, one eye is not aligned with the other eye.
Types of squint
The classification of Strabismus may be based on a number of features, including the relative position of the eyes, whether the deviation is latent or manifest, intermittent or constant, concomitant or otherwise and according to the age of onset and the relevance of any associated refractive error. The type of strabismus is established by a detailed history and orthoptic examination.
- Infantile esotropia (syn: congenital or essential esotropia) is an idiopathic syndrome in which an esodeviation is present before the age of six months. It is invariably associated with other clinical features including dissociated vertical deviation, inferior oblique overaction, latent nystagmus, crossed fixation, asymmetrical monocular optokinetic responses (OKN) and, usually, no refractive error.
- Acquired strabismus includes fully and partially accommodative refractive esotropia, convergence excess esotropia, cyclic esotropia, occlusion esotropia and various forms of paretic squint.
- Exotropia may also occur in congenital and acquired forms, both concomitant and incomitant .
- Vertical strabismus includes dissociated deviations, cyclovertical muscle anomalies and restrictive conditions (e.g., Brown's syndrome) as well as rarities such as double elevator palsy .

These broad categories of strabismus are distinguished by having various aetiologies and usually differ in prognosis, with and without treatment.
Strabismus Management
1. Infantile esotropia
There are five broad considerations in planning management of infantile esotropia:
Development of binocular vision
Children with untreated infantile esotropia, when assessed at school age, will commonly show equal visual acuity and a dense alternating suppression with no form of demonstrable binocular cooperation. Early surgery is advocated on the basis that the primary defect is a motor one and alignment of the eyes before some critical age might permit the development of binocular function. This is the most controversial issue in the management of the condition and has the greatest influence on the timing of any surgery. As yet, there is not enough evidence to decide the matter and contrasting policies are followed by different surgeons.
To illustrate the variety of results that have been obtained, three studies have been selected:
- In a widely cited study that stimulated further work on early surgery, 93% of 106 children operated upon and successfully aligned before the age of two years, had worth 4-dot fusion or gross stereopsis. Of the children aligned after this age, 31% demonstrated a similar outcome.
- In a series of 358 patients who had undergone surgery for infantile esotropia, 20% were orthotropic with fusional amplitudes and normal retinal correspondence. None had stereopsis with TNO test and only three had low-grade stereopsis on the titmus test. The probability of achieving subnormal binocular vision appeared to decrease with increasing age at surgery and was consistent with the view that surgery before the age of two produces better results but these may still be obtained in patients at a later age.
- In a recent prospective study of 98 out of 118 patients who underwent surgery for infantile esotropia, and who had remained aligned to within 8 PD of straight five years later, one third had stereopsis on the titmus test (range 200-3000 seconds of arc). Thus 22% of the original group had obtained some form of binocular function and 68% had remained well aligned. No patient with a divergent squint of any degree demonstrated stereopsis.
In attempts to improve results, other studies have aimed for alignment by 12 or even 6 months of age, but no better stereopsis has been achieved.
The most common outcome of successful surgery is the monofixation syndrome with subnormal binocular vision. The surgical target in infantile esotropia is, therefore, usually within 10 PD of straight, this being the maximum angle at which monofixation is possible.
The advantages cited for various forms of subnormal binocular vision over complete suppression are: simultaneous binocular perception, fusional vergence, intact binocular field, normal distance judgement and, sometimes, gross stereopsis. An advantage to later surgery is a lower risk of subsequent amblyopia.
As an alternative to surgery, botulinum toxin injection into the medial recti has been reported but is not at present in general use.
Correction of amblyopia
While many children with infantile esotropia demonstrate balanced alternating fixation, amblyopia may occur. In untreated squint this is reported as between 13% and 33%, rising to 20-80% after surgery. It is therefore important to monitor infants following squint surgery and to treat any amblyopia detected.
Provided that suitable orthoptic supervision is carried out, it is not necessary to delay surgery until completion of amblyopia therapy.
General health issues
Systemic disorders which increase the risks of anaesthesia should be regarded as a relative contraindication to early surgery. The angle and direction of squint in infants with cerebral palsy and other neurological disorders is often unstable. In such patients surgery for presumed infantile esotropia may be better deferred at least until two years of age. However, in a prospective study of surgery for essential esotropia, the outcome was no worse in the neurologically impaired or premature infants.
Surgical treatment
The definition of satisfactory cosmetics and the optimum age for surgery in a given case are a matter for discussion between the parents, orthoptist and surgeon. As regards to the type of surgery, published evidence suggests that bi-medial rectus recession is the most effective procedure, perhaps combined with simultaneous resection of one lateral rectus for large angle squint.
The type and amount of surgery to perform for a particular squint is a decision for the experienced surgeon. Parents need to be advised that, whilst accuracy in measuring and operating upon Strabismus is essential, the response to surgery is variable and cannot be guaranteed. It is good practice to agree on the objectives and discuss the actions necessary if the desired surgical outcome is not achieved.
Correction of associated features
Correction of overacting inferior oblique muscles found in association with 'V' pattern strabismus may be required on cosmetic grounds, including a compensatory abnormal head posture and, if marked, is usually carried out at the same time as the esotropia surgery. If binocular function is present after surgery, persistent inferior oblique overaction may disrupt it.
In summary, there is no series of cases reported in which successful alignment in infantile esotropia has allowed the development of high grade stereopsis associated with bi-foveal fixation (40 seconds of arc or better). If the eyes are aligned to within 10 PD of orthotropia, up to one third of patients develop subnormal binocular vision. There is evidence to suggest that this binocular vision provides functional advantages. However, there are no accurate means of predicting preoperatively which patients will enjoy this outcome.
2. Acquired strabismus in early childhood
General principles
Most of the preceding recommendations in infantile strabismus management also apply in acquired strabismus.
The important differences are
- An assumed history of possible normal binocular vision prior to the onset of squint.
- A greater likelihood that optical treatment alone will be required.
- The related risk of loss of binocular vision if treatment for the squint is delayed.
In view of these factors, treatment should aim to restore ocular alignment and binocular vision as soon as possible. It is therefore necessary to consider whether a given case of childhood strabismus has a chance of a good functional result following therapy on the basis of the history, with particular regard, to age, and findings such as the presence and severity of any associated amblyopia and / or suppression. It may also be necessary to inform general practitioners that delay in the referral of young children with strabismus serves no useful purpose. Information regarding the mode (i.e., constant or intermittent) and time of onset of a squint is helpful in assigning appropriate urgency to appointments.
Management sequence
It is important to measure and fully correct significant refractive error before planning any surgical correction of strabismus. It is also desirable to have corrected any amblyopia present.
Pre-operative prism adaptation in acquired strabismus
There is good evidence to show an improved predictability and outcome of surgery in acquired esotropia following adaptation using Fresnel prisms on spectacles. Briefly, the method is used to discover patients with fusion potential and may disclose a larger angle of squint than that first measured. Surgery carried out on this larger angle has a greater chance of success without an increased risk of over-correction, and prism-responders so treated are less likely to require re-operation. This technique is recommended where practicable, particularly if measurements of squint angle are variable.
3. Exotropia
Exotropia may be constant or intermittent and may present as a primary condition or be consecutive (following esotropia) or secondary to unilateral visual loss.
Constant primary exotropia is much less common in this country than esotropia. It is thought to be more commonly associated with other developmental abnormalities. The deviation is usually large with alternating fixation and a low risk of amblyopia and the squint is present on near and distance fixation even when accommodation is stimulated.
In contrast, intermittent exotropia, which may begin in infancy, is noted when one eye drifts outward at times, particularly in bright conditions, on distance fixation and when the patient is tired or unwell. When the deviation is manifest there may be suppression or diplopia, typically overcome by closing one eye. Intermittent exotropia may be found to measure the same angle at near and distance. More commonly, the eyes are straight at near and divergent in distant and far distant fixation. In convergence weakness, the angle is larger on near fixation. Children who have straight eyes on near testing demonstrate good stereopsis (60 seconds of arc or better) when old enough to perform detailed tests.
Treatment aims are generally the same as for esotropia, namely eradication of amblyopia, restoration of fusion where possible and re-alignment where necessary to achieve satisfactory function and appearance.
Orthoptic treatment is useful in improving control of residual intermittent exotropia in children with good fusion who are old enough to learn how to be aware of the deviation of one eye. Training is then aimed at improving fusional amplitudes.
4. Vertical strabismus
The two most common causes of vertical strabismus in childhood are superior oblique under actions and dissociated vertical deviations. Superior oblique weakness may be due to paresis or to maldevelopment of the muscle tendon. Typically, hypertropia in the affected eye will be associated with a compensatory head tilt to the opposite side with chin depression and overaction of the ipsilateral inferior oblique. The head posture develops as soon as the infant gains head control when upright. It may not be noticed by the family and photographs are useful evidence. There is usually evidence of fusion in the presence of the head posture in primary gaze. Fusion is prevented if the hyperdeviation or cyclodeviation is large.
The aim of surgery is to allow normal binocular fusion in primary gaze and on looking down without abnormal head posture. Strabismic amblyopia is detected by the use of suitable tests performed on children who have presented with manifest squint. Anisometropic amblyopia is usually discovered when a child presents having failed a screening test of visual acuity.
Amblyopia may be of mixed etiology; e.g., children with anisometropic amblyopia may present with strabismus, and unilateral cataract may lead to secondary squint in which the amblyopia is likely to be severe.
The minimum criterion for diagnosing amblyopia on a test of visual acuity is accepted to be two lines difference between the eyes on the linear Snellen test. This is usually equivalent to a difference of one octave in spatial frequency resolution. On repeated testing it may be possible to detect amblyopia in an eye with visual acuity of 6/9 when the fellow eye sees 6/6 (i.e., one line difference).
Vigilance against strabismus
Intermittent deviation of the eyes is a quite common finding in healthy neonates and should not cause undue concern. Normal binocular co-ordination becomes evident at about three months and strabismus after this age is significant.
Constant squint is generally recognised early by the family, health visitor or general practitioner. A positive family history of squint or amblyopia should alert those in primary care when carrying out routine checks or immunisations.
Strabismus is often found in association with neurological disease such as in cerebral palsy and in craniofacial developmental anomalies.
Strabismus, amblyopia and refractive error are much more common in children with treated or regressed retinopathy of prematurely (ROP). Premature infants with a history of stage III ROP or worse should be followed up after the neonatal period to screen for these complications.
If squint or amblyopia is suspected in the primary care setting, it is appropriate to provide for direct referral to an optometrist or an orthoptist to exclude refractive error and strabismus. If no abnormality is detected, such patients may be discharged. Cases with intermittent or constant manifest squint should be referred to an ophthalmologist without delay. In all children referred with Strabismus or amblyopia the possibility must be considered that this is the presenting feature of a serious ophthalmic or systemic disease requiring urgent management.
There are many aspects of strabismus and amblyopia management which require audit from time to time in order to be sure of the quality and efficacy of care provided. Audit requires clear objectives and adequate resources in order to be carried out successfully.
In order to audit the results of treatment in strabismus, reference should be made to the aims of treatment which are:
- Optimum visual acuity in each eye
- Optimum binocular function
- Good cosmetic appearance
The first two aims may be quantified on examination, while the third requires questions to be asked of the patient and parents, although alignment of the eyes to within 10 prism dioptres of straight is usually compatible with an acceptable appearance and with peripheral fusion.
Suggested data to be assessed in audit
i) Status
- At presentation
- During and after amblyopic treatment
- Preoperative
- Postoperative
- On discharge
ii) Patient variables
- Age
- Visual acuity
- Refraction/prescription
- Diagnostic category
- Associated diagnoses
- Strabismus angle
- Surgery
- Target angle
- Technique
- Complications
iii) Event
- Out-patient appointment
- Out-patient attendance
- Under-correction
- Over-correction
- Re-operation
Visual Field
The visual field is the total area where objects can be seen in the peripheral vision while the eye is focused on a central point.
Visual field parameters
The normal visual field extends from the point of fixation to about 60 degrees nasally and superiorly, 70-75 degrees inferiorly and 90-95 degrees temporally. Visual field tests are used to discover any abnormalities in the retina and visual pathways in the orbit and brain.
Glaucoma is one of the most common conditions tested by perimetry in ophthalmology and gives the doctor a basic starting point of treatment to prevent further field loss.
When field abnormalities are found, they are analysed by their shape, placement and extent.
Terminology commonly used in perimetry
- Hill or peak is the area wherein the retina's potential to respond to a target (a light or a white object against a black background or any other stimulus) is the most sensitive area to yield a response.
- Isopter is the boundary of a number of points that are connected to form a visual pattern of perception that has been determined with the same size test object. It is found by starting a moving test object in from the nonseeing periphery to a point where the test object is first seen by the patient and this is tested in all twelve meridians and the points of perception are connected.
- Scotoma is a blind area where the patient cannot see a test object. It is an abnormal blind spot that is surrounded by a seeing visual field. Each scotoma is evaluated with different sized test objects first seen by the patient and this is tested in all twelve meridians and the points of perception are connected.
- Para indicates a nearness to something, such as the center or macula which would be termed paracentral or paramacular. Example: Paracentral scotoma.
- Peri indicates that a scotoma can be around something, such as peripapillary which means around the disc. Below are some common perimetry definitions:
- Horizontal meridian - horizontal line through fixation which divides superior and inferior visual fields.
- Vertical meridian - vertical line through fixation which divides left and right visual field.
- Absolute - no recordable vision within a scotoma
- Acurate or bjerrum scotoma - Arching visual field defect within the area between 10 to 25 degrees in the superior and inferior field.
- Central scotoma - defect involving fixation.
- Caeco-central scotoma - defect encompassing the physiologic blind spot and fixation.
- Split fixation - defects close to but not involving fixation.
- Altitudinal - complete loss of either the superior or inferior field from the nasal to the physiologic blind spot.
- Hemianopic / Hemianopsia - defect respecting the vertical meridian.
- Quadranopic / Quandranopsia - defect of the vertical meridian, involving only one quadrant.
- Homonymous - defect occupies the same side of visual space in both eyes. Defect is named for the side which is abnormal.
- Congruous - Bilateral hemianopic defects which are essentially identical; the fields can be superimposed on one another. Congruity indicates a posterior lesion location.
- Incongruous - Heminopic defects which are not identical incongruity indicate an anterior lesion location.
- Rods are cells in the retina, mainly located in the midzone of the retina (30 degrees to 60 degrees). There are 138 million rods distributed in the retina outside the macula, they respond to low light better than cones and do not perceive fine detail or distinct colour. Night blindness is the common symptom of field defects in this region.
- Cones are cells found mostly in the macula and are capable of the best visual acuity and colour discrimination. There are six million cones in the macula. The center of the macula, the fovea, is made up of only cones and is the central fixation point for the visual field test.
- The optic disc causes the normal blind spot because it has no retinal receptors. The disc is located on the nasal side of the macula. It is also referred to as the optic nerve head. Afflictions to the optic nerve from vascular problems, tumour, trauma, infection or inflammation create field defects which are monocular and point to the disc. In other words vision can be completely gone in the eye in which the optic nerve is affected.
- The left half of both visual fields is produced by the retinal receptors in the right eyes' temporal retina and the left eyes' nasal retina. The opposite is true of the right half of the visual field.
- Chiasma is the part of the visual pathway to the brain where the pathway crosses each other. If there is a disease in the chiasma, the vision of both eyes can be affected either both temporally or both nasally.
- Optic Radiation is part of the visual pathway to the brain. Diseases affecting this part can cause loss of quarter field of vision (Quadrantanopia).
- Cortex: If there is a disease adjacent to the visual Cortex, half of the vision (temporally and nasally, just sparing the macula), can be lost.
The visual pathway and typical patterns of visual field loss. (Fig. 3.7).
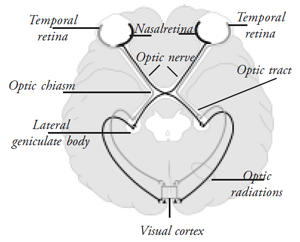
These 2 diagrams illustrate how the nerve fibres are arranged to transmit information from the retina to the brain.
All the fibers leave the eye, down the optic nerve. The first diagram shows how these fibres reach the optic nerve head (the optic disc), from each part of the retina. These fibers are very sensitive to increased pressure inside the eye (which is what happens in glaucoma). In untreated glaucoma cases more and more fibre bundles are progressively damaged resulting in bjerrum scotoma. When progressively more and more bundles of nerve fibres are damaged, this produces scotomas in the visual field, typically the bjerrum scotoma usually found between 5-20 degree from fixation, and the nasal step.
The second diagram shows the pathway of the fibers from the eye to the brain. Half the numbers of fibers from each eye crosses over and join the uncrossed fibers of the opposite eye at the chiasma. This arrangement makes the right half of the brain see objects in the right half of the visual field and left side of the brain sees objects in the left half of the visual field.
The fibers transmitting images of the temporal fields must cross over, which they do at the "chiasm". So if these fibres are damaged a bitemporal hemianopia is produced. The other typical field issues in damage to the different parts of the pathway are also shown.
Nerve fiber pattern of retina in its relationship to retinal vascular tree showing the two typical nerve fiber bundle defects found in glaucoma.
Extent of a normal visual field
Normal visual field is determined by the size of the test object employed and the distance at which the test is made. With a 3mm white test object at a distance of 33mm (Radius of the perimeter) the field limit is about 90 degrees temporally, 70 degrees inferiorly, 60 degrees medially and superiorly.
The structure of the normal field is considered to be of two portions: The central field, which constitutes that portion of the visual field within the 30 degree radius of fixation, and the peripheral field which makes up the remainder.
Blind spot: The blind spot is physiological blind area which corresponds with the exit of the optic nerve. It is located about 12 to 15 degrees temporal to the fixation and about 1.5 degrees below the horizontal meridian. The normal measurement of the blind spot is approximately 5.5 degree horizontally and 7.5 degree vertically.
Isopter: The isopter is the contour lines of the visual fields and it is decided by the size of the stimulus and the distance at which it is viewed. It is expressed as a fraction (size/distance).
Visual field examination
The visual field examination measures the expanse and sensitivity of vision surrounding the direct line of sight, that is, peripheral vision. Unlike most losses of central vision, defects in peripheral vision can be subtle and are often unnoticed by a patient. Disturbances in peripheral vision are commonly due to diseases of the retina, optic nerve, or structures of the visual pathway in the brain. Early detection of these abnormalities by a visual field examination permits initiation of treatment that may halt further progression of the disease and prevent irreversible loss of central, as well as peripheral vision.
The visual field examination consists of a number of different testing procedures. Two relatively simple techniques are included in the comprehensive visual examination to obtain a gross evaluation of the patient's peripheral vision: confrontation visual field testing and Amsler grid testing. Performance of these tests is often the responsibility of the OA. The results of these two tests may indicate the need for more exact procedures of perimetry.
Confrontation field test: The confrontation field test compares the boundaries of the patient's field of vision with that of the examiner, who is presumed to have a normal field. Here is how to perform the confrontation field test:
- Seat the patient at a distance of 2 to 3 feet from you. Confront (face) the patients, cover or close your left eye, and have the patient cover the right eye. You and the patient should fixate on each other's uncovered eye.
- Extend your arm to the side at shoulder height and slowly bring two fingers from beyond your peripheral vision toward your nose into the field of vision midway between the patient and yourself. Ask the patient to state when the fingers are visible.
- Repeat the process of moving fingers into the visual field from four different directions. If you picture a clock face in front of the patient's eyes, you perform the hand movement from about 2 o'clock, 4 o'clock, 8 o'clock, and 10 o'clock, each time bringing the fingers toward the center of the clock face.
- The patient should see the fingers at the same moment you do in each of the four quadrants (upper-left, upper-right, lower-left, and lower-right quarters) of visual field. (Note: A quadrant of vision described from the patient's point of view) If the patient does not see your fingers the same time you do, the breadth of patient's visual field in that quadrant is considered to be smaller than normal and additional perimetric studies will probably to be performed.
- Record the patient's responses in the patient's chart by indicating simply that the visual field is comparable to yours or that it is reduced in any of the four quadrants for that eye.
- Repeat the procedure as described with the patient's other eye and record the results similarly.
Amsler Grid test
The Amsler grid test determines the presence and location of defects in the central portion of the visual field. The Amsler grid is a printed square of evenly spaced horizontal and vertical lines in a grid pattern, with a dot in the center. The chart grid and dot may be either white on a black background or black on a white background. Here is how to perform the Amsler Grid test.
- Have the patient hold a white-on-black test card about 16 inches away with one hand and cover one eye with the other hand, an occluder, or a patch.
- Direct the patient to stare at the center dot and to report if any portions of the grid are blurred, distorted, or absent. The patient should not move the gaze from the center dot, so that the presence of any distortion can be assessed.
- If the answer is yes, you may repeat the test with a black-on-white Amsler recording chart, on which you ask the patient to mark the location of visual difficulties.
- If test results are normal, state so in the patient's record. If abnormal, state so. Include the Amsler recording chart in patient's record. If visual disturbances noted, the patient is a likely candidate for further studies.The patient may also repeat this convenient procedure independently at home and report the changes to the ophthalmologist's office. The patient should perform the test monocularly one eye at a time, always at the same 16-inch distance and under the same illumination.
Tangent screen test
The purpose of this test is to determine the central 30 degree of the visual field. It is best performed by the use of a tangent screen. A tangent screen is usually made of black felt material. The meridians are stitched in 5 degrees interval (stitched at 10, 15, 20, 25 and 30 degrees from the point of fixation). The test is conducted at a distance of one or two meters from the eye. Test objects varying from 1mm to 50 mm are used. This is the most common visual field test. The test is simple and easy to perform. The targets are in the form of circular discs or balls of sizes which vary from 1 mm to 50 mm in diameter.
These test objects are inserted in the end of a long wand. The holder or wand should be covered with a black cloth of the same material as the screen. Painted black wands cast a considerable amount of light reflection and should be avoided because they are distracting to the patient.
The most common method of recording one's results is to insert black pins into the screen at the points indicated and then transferring these points to a chart after the examination has been completed. In some of the newer tangent screens (Bausch and Lomb), there are projection devices and a self-recorder, so that the insertion of pins is not necessary. It is desirable that when pins are inserted the distraction caused by this movement is at a minimum. With the new tangent screen, the projection of targets virtually eliminates the distraction caused by the movements of the examiner.
Perimetry: Generally Lister's perimeter or Fimonk projection perimeter is employed. An ideal perimeter would be formed by an arc of one half of a hollow sphere (with a radius of 33 cms) which could be rotated throughout the 360 degree of the fixation. The stimulus or test object would be moved from the periphery towards the fixation target with the help of the knob behind the instrument. The chin rest is placed at the center of the sphere.
Use of the Goldmann type perimeter
I. Set-up
- The instrument should be placed in a room that is completely blacked out where there is total control of illumination (the only illumination should be from the instrument itself).
- The instrument should be placed on a level table and the legs of the instrument should be adjusted so the spinite level bubble is centred.
- At the start of any clinic when the instrument is used the calibration should be checked using the light meter as follows:
- The illumination of the target spot should be set at 1000ive tangent shining on the light meter head placed in the slot as shown in the manual, this adjust using the rheostat on the side of the instrument.
- The background illumination is adjusted by sliding the housing around the lamp (at the top of the bowl) up and down - the setting should be 31.5 as indicated in the manual and is measured with the light meter now placed in the slow by the chin rest.
If at any point during the test a defect appears, it should be explored for its size, shape, and density. This is accomplished by moving the test object from a blind area into a seeing area at right angles to the border of the defect. The size and shape of this defect should be outlined at least twice in order to check the patient's reliability. The density of the field defect is determined by using a number of test objects of various sizes. If a small test object was employed when the defect was initially discovered, then a larger test objects should be used and vice versa.If the patient's responses are confusing and equivocal, it is probably because the test object is too small to be easily seen. In such a case, a larger test object should be chosen.
II. Performing perimetry using the Goldmann instrument
- After placing a chart into the holder the patient is seated at the perimeter-one eye occluded, chin on the chin rest and head against the bar the buzzer in his / her hand.
- Adjust the chin rest with the two control knobs asking the patient to look at the fixation target looking also the telescope to check the fixation - the pupil should be lined up with the cross wires.
- Peripheral fields are normally plotted with the 1.4 e target i.e. maximum brightness with 0.25 mm target. The normal dimensions are indicated on the front of the Goldmann manual.
- If there is any field (central 30 degree) the patients prescription should be placed in the lens holder-using full aperture lenses. It should be the prescription they normally use for reading. 1.4 e target should be used.
- The technique for checking the field is the same as for tangent screen and Lister perimeter.
The advantages of this method are
- Totally controlled and even illumination for background tangent.
- Using the knob on your right for presenting the target you can either have the target constantly displayed and when you push down on it, it disappears or the way it is normally used. If you use the knob through 180 degree the target will be suited off and only presented when you press the knob down, you can then make the target disappear at will to check the patient's response.
- As more accurate and repeatable fields can be plotted with the instrument it should be used whenever you wish to have a full visual fields exam carried out and whenever you wish to monitor a changing field.
III. Automated perimetry
Automated perimetry was developed to standardise visual field testing and therefore to increase the reliability of visual field tests. Various manufacturers make automated perimeters based upon computerised projection systems and LED (Liquid Crystal Display) systems. Automated perimeters can perform screening and diagnostic field tests and can use kinetic and static methods. These perimeters are most often used for static threshold testing.
The most widely used automated perimeter is the Humphrey field analyser, which has become the standard for visual field testing.
Visual field pathologies
Field defects: Fields are classified as those which encroach from the periphery of the field, and those which originate within the confines of the margins of the field itself.
Scotomate
A Scotoma is an area of partial or complete blindness within the confines of a normal or relatively normal visual field. Within a scotoma, the vision is more depressed than in the area of visual field surrounding it. When the depressed area of scotoma expands into the periphery of the field, it is said to have "broken through". Scotoma may be divided into the following types:
- Central scotoma, which involves the fixation area and is always associated with a loss of visual acuity.
- Pericentral scotoma (annular scotoma), when the fixation area is relatively clear and the field immediately surrounding it is deficient.
- Paracentral scotoma, when the area of depressed visual field is to one side of fixation. These scotomate may also be denoted as to their position, whether they are nasal or temporal in relation to the fixation point.
- Cecal scotoma, when the area of the normal blind spot is involved.
- The nerve fiber bundle scotoma, also referred to as an acurate, Bjerrum, or comet type of scotoma. This type of depression extends around the fixation point from the blind spot in an arched fashion and ends typically on the nasal side of the field with a sharply demarcated border. This type of scotoma can occur either above or below the blind spot but seems to issue from it.
The intensity of a scotoma varies from absolute blindness to a minimum detectable loss of visual acuity. If there is complete blindness to all sizes of test objects, it is an absolute scotoma. If the area involved is definitely out only to smaller test objects and larger test objects can be seen, then it is referred to as a relative scotoma.
Contraction of the visual field
Contraction usually occurs as an area of blindness emanating from the periphery of the field and extending towards the center. If the contraction affects only one part of the field, it is often referred to as a sector defect. Sector defects bounded by vertical or horizontal diameters of the field are hemianopic defects. The term hemianopic is used to indicate a defect occupying half of the visual field and which is, usually, a bilateral defect. A hemianopic defect is homonymous right or left, when the corresponding halves of both eyes are affected. In this instance there is blindness in the temporal field of one eye and in the nasal field of the other eye. The dividing line between the seeing and the non-seeing portions of the field is vertical.
When a quadrant of each field is affected, a quadrantanopia is present. A defect or loss of the upper or lower half fields is termed as altitudinal hemianopia. A bi-temporal hemianonia is a visual field defect that may vary from the slightest depression of the upper temporal portion of the field to complete blindness in each temporal field.
A congruous homonymous hemianopic defect is one in which the defects in the two fields are super imposable, i.e., completely in this instance, when one maps the visual field of one eye, its margin will be identical to the visual field of the other eye.
Common testing methods
- Confrontation
- Tangent screen
- Goldmann perimetry
- Automated (Humphrey, Octopus, Dicon, Topcon)
- Amsler grid
Low Vision Aids
Low vision has been a subject of continued neglect by ophthalmologists for various reasons. In reality it is only the willingness of professionals to take up the low vision field that would prevent avoidable blindness.
The difficulty in availability, accessibility, and the high cost of low vision devices, are problems in this field. If a large number of ophthalmic professionals are involved in this field, these problems could be rectified. The global initiative for elimination of avoidable blindness includes low vision as an important cause.
The strategies are
- To develop and make low vision services available and optical devices available for all those in need, including children in blind schools, and integrate their education.
- To include provision of comprehensive low vision care as an integral part of national programmes.
When conventional spectacles can no longer help and surgery or medical treatment is not appropriate, it is time to consider low vision aids. Low vision aids are magnifying devices in a wide array of strengths and designs to enhance the functional vision for poorly sighted persons. They range from simple hand-held lenses.
Low vision aids are classified into conventional lenses and magnifying devices. Different ones are required for different visual tasks. They do not enable everything to be seen clearly and easily. Low vision devices are determined depending upon the patient's existing visual acuity, age and occupation for which the optical aid is designed. For viewing distant objects, telescopes or binoculars sometimes can be helpful. The patient often will have to try two or three aids before deciding on the appropriate one.
Definition
The World Health Organization defines - "A person with low vision is one who has impairment of visual functioning even after treatment, surgery or standard refractive correction and has a visual acuity that range from less than 6/18 to light perception or a visual field of <10 degrees from the point of fixation, in the better eye but who is potentially able to use vision for the planning and or execution of a task".Optics of low vision aids
LVA function by presenting the patient with a magnified view of the object. It increases the visual angle subtended by an object at the eye thus producing an enlarged retinal image. The basic principle of most of the optical devices is to provide magnification, spreading the image over a greater area of the retina to incorporate a larger number of functioning receptors.
Classification of low vision aids
Optical aids
- Telescopes
- Ashperic lenticular spectacle lenses
- Hand magnifier
- Stand magnifier
- Fresnel prism
- Prismospheres
- Paper weight magnifier
- Bar magnifier
- Pocket magnifier
- Electronic aids as closed circuit television system
Non optical aids
- Large - print books
- Reading stand that supports posture and comfort
- Illumination devices such as fluorescent lamps and glare control devices such as photochromatic glasses
- Writing devices such as typoscopes
- Medical management devices such as insulin syringes with bold letters
- Mobility canes
- Sensory substitution devices such as talking books
Ocular conditions benefited by low vision aids
- Albinism
- Central serous retinopathy
- High myopia
- Microphthalmos
- Diabetic retinopathy
Ocular conditions where there is not much benefit from low vision aids < 2/60 and field of vision is <10 degrees.
- Retinitis pigmentosa
- Advanced glaucoma
- Optic atrophy with field defects
- Retinal vascular occlusion
- Macular dystrophy
Low vision evaluation
Evaluation of a low vision patient begins with assessment of the clinical background, functional assessment, vocation, independence in daily living activities, mobility, social interaction, psychological reaction, reading and writing performance with patient's stated needs. It is more important to evaluate the patient as a whole. Just recording the complaints and examination will not help to support the patient.
The optometric evaluation includes vision examination using a 1 meter or 3 meter chart. The patient has to be seated at a specific distance. The chart has a geometric progression of letters with lines equivalent to the standard snellen visual acuity chart. This chart has logarithmic units and the dioptric add on the right side and letter size in "M " units on the left side. This is the Logarithmic visual acuity chart 2000 by the precision vision company. This chart is very useful in evaluation of the low vision patient. The refraction is done at one-meter distance, using retinoscopy. Bracketing method can be used subjectively to arrive at a proper refractive correction. A majority of low vision patients will benefit from LVA for near vision. All that is required is motivation to use a low vision device and the need to use it professionally. The following formulas are useful in the day today low vision practice:
- The "Kesten Baum Rule" is the reciprocal of the distant Snellen visual acuity; e.g. if the distant Snellen visual acuity is 6/60 then the reciprocal will be 60/6 = 10D. A patient will require 10 D add for near vision.
- The Brazelton formula: Magnification = Best corrected distant visual acuity x 2.5x.
- Lighthouse method: The lighthouse near visual acuity card can be used at 40cm test distance requiring an add of + 2.50 D. The add can be increased depending on test distance even up to 10cm. The chart gives the letter size in 'M' units on the left side and diopteric adds on right side.
The Halberg trial clips make refraction quicker, more convenient and accurate. The errors arising out of vertex distance, pantascopic tilt, are eliminated. The optometric evaluation also includes visual fields examination using amsler grid, central and peripheral fields. If the scotoma recorded in amsler grid is more than 30 degrees from fixation then the use of a magnifying spectacle is guarded. The central and peripheral fields are documented. If the fields are constricted more than 10 degrees then the use of a telescope may not help the patient. Contrast sensitivity is recorded to help in the functional vision testing of a low vision patient. Having gathered all the information, a trial of low vision devices is given with telescopes for distance and the hand or stand magnifier for the near work. The required illumination, glare control devices, contrast requirement are also explained to the patient. In the following description, specific low vision management pertaining to different ocular conditions is discussed.
Eccentric viewing
A common difficulty when trying to read with a magnifier is that some parts of a word can be seen and some parts can not be seen. With this particular problem, which anyone with central vision loss due to maculopathy may well experience, people often discover that they can see the whole word if they look above it rather than directly at it. This is known as eccentric fixation.
Therefore, in order to read, it is necessary to hold the eye steady (steady eye technique) with the gaze firmly fixed above the line to be read. Thus it is no longer possible to read in the ordinary way, with the print held steady and the eyes moving quickly along the line, taking in whole words and phrases. Using eccentric fixation, the line of print must be moved, not the eye. Reading by this technique is much slower than by traditional methods, particularly at first as it goes against a lifetime's experience. It can be tiring and frustrating, but at least it does enable reading. Eccentric viewing methods can also be used for activities other than reading. This is comparatively simple to do when trying to see objects. Most people with maculopathy, for example, soon find that to see the clock on the mantelpiece they need to look at from the sides, or to look down towards the fireplace or up towards the ceiling. Relatives and friends can help by making sure, for example, that a cup of tea is placed on the "good side" rather than immediately ahead.
Scanning
People with a very narrow field of vision, perhaps because they suffer from advanced glaucoma, need to move both their eyes and their head in order to read, for example, a notice pinned up on a wall. Anything printed in columns, such as a newspaper, will be easier to read because the need for scanning will be reduced. When reading longer lines it may be better to move the print across the line of vision in order to read it.
Keeping to the line and finding the next line can present problems when scanning. A finger on the line or a ruler underneath it can help. Many people are helped by using a typoscope, a matte-black thick card with a window cut out the width of the line. This can be homemade or purchased from the Partially sighted society.
When the right side field is lost, as may happen after a stroke, reading can be extremely difficult as the eye is scanning into nothingness/nothing. Loss of the field on the left side is not so incapacitating, though there may be problems in finding the next line. A bright red vertical line drawn down the page margin may help. It would need to be drawn on the side of the visual loss. For someone with a right field loss, the line denotes how far it is necessary to complete one line of reading. If the field loss is on the left, it shows the starting point of the line.
Another method is to place a bright bookmark along the left-hand edge of the print, so that the reader can turn his head at the end of each line until the bookmark is seen. Typoscopes may also help, by keeping the eye on the line and limiting the number of words that can be seen. This reduces the amount of information the brain has to sort out.
Monocular vision
A large number of people lose sight in one eye by accident, injury or disease. No one knows the exact statistics. People who have lost the sight of their right eye will have a blind spot to the left of center, and vice versa. Looking at a page containing a cross and a circle spaced three inches apart demonstrates this.
Someone who has lost the sight of their right eye should look at the cross from a distance of about 15 centimeters, and then move the page slowly further away, and then bring it closer. The spot will disappear and then reappear. Someone who has lost sight in the left eye should first turn the page upside down (but still look at the cross) before trying this experiment. People with sight in both eyes can compare what happens if they do this with either eyes open or one eye shut. Anyone with normal vision in the remaining eye is not entitled to be registered as partially sighted, though it may well take them some time to adjust to coping with monocular vision. This is because they lose part of their field of view, and initially at least they will have problems with depth perception.
It is possible to relearn how to see in depth. Nick Rumney, an optometrist who only has vision in one eye, suggests a useful exercise. Pour coloured water into a clear glass, and ask a friend to keep moving the glass so that the distance required pouring into it accurately varies. The safest way to pour is not from a height, but to let the bottle or jug touch the edge of the glass. To learn to judge the distance between objects, move the head from side to side. The objects will appear to "move" in relation to each other. The distance they appear to move apart can then be used to gauge the actual distance.
Eventually the remaining eye adjusts to its new role, though there is nothing that can be done to compensate optically for the lost field of view. People need to learn to turn their head more, and when driving make more use of their wing mirrors. People with one eye can hold an ordinary driving license, though they must inform the DVLA and their insurance company of their condition. They are not allowed to hold a professional driving license as needed for public service or heavy goods vehicles. As with other visual impairments, the best support and advice is likely to come from someone else in the same situation. "A Singular View - The Art of Seeing With One Eye" was originally written by Frank Brady, an American engineer who lost an eye as a result of a flying accident. The English edition is edited by Ron Hearnden, a Canadian businessman who lost an eye in asking accident. Nick Rumney, who lost the sight in one eye as a schoolboy, recalls that the most constructive help he received was from a teacher who only had one eye.
Here are some tips that can help people with only one eye
- When putting a drink down, place the other hand on the table and put the glass down next to it.
- It can be very difficult to judge the last step on a staircase. It may merge into the floor, especially in poor light or when the stair and floor carpets are the same. Move cautiously, feel ahead with your foot, and keep a hand on the banister.
- Wear protective spectacles at all times, especially when gardening. Polycarbonate lenses are the safest.
- When going out for a meal with a friend, make sure that he or she sits on your seeing side, but remember that the waiter may turn up on the blind side.
- In the early days, stop at a kerb to gauge the depth before crossing the road.
- If you are afraid that you may "miss" the outstretched hand when a friend greets you, put yours out first!
Points to remember
Whenever approaching the low vision patient, the optometrist should consider the following points to provide the best of devices depending upon their visual needs:
- Possible wider field of view
- Light weight for easy-handling
- Minimised or no aberrations with great light transmission
- Ability to focus
- Appropriate magnification
- Compactness
Low vision devices usually help the patient to enhance the functional vision with
- Good illumination for close work
- Moving closer to objects to see better
- Using objects with high contrast
- Allowing enough time for looking
- Adequate training / practice to learn to use.
The basic principle is to use the simplest device that will satisfy the specific visual needs of the patient. Low vision aids helps only to enhance the impaired vision, not to improve or restore vision. Even a small improvement by means of low vision aids often can help the patients, allowing a greater chance for education and employment.
Summary
This unit teaches the trainee the common refractive errors and how the tests are conducted with different equipment and instruments. Steps to be followed in conducting the visual field tests are also given in detail. Details about the different types of squint and the treatment to be given to the patients will help the trainee in guiding the patients. The aids that could be used by patients with low vision are also listed for the trainees. Here are some key points to remember:
- Myopic patients will have blurred vision of the objects at a distance
- Hypermetropic patients will have difficulty in seeing objects which are near by
- There are two types of Astigmatism: regular and irregular Astigmatism
- There are six extraocular muscles which act to rotate the eye about its vertical, horizontal and antero-posterior axes
- The visual field is the total area where objects can be seen in the peripheral vision while the eye is focused on a central point
Student exercise
I. Fill in the blanks
- Myopia is corrected by ________ lens.
- Astigmatism is corrected by _______ lens.
- The near vision is recorded at a distance of ______.
- Hypermetropia could be corrected by using ______ lens.
- Symptoms of astigmatic patients are _______.
- Visual acuity is measured with the help of ________ chart.
- _______ is the normal distance maintained for vision assessment.
- ________ is a non optical aid.
- Humphrey perimeter is used to measure _________.
- Normal field of vision extends on the temporal side to _______.
II. True/False
- Prism lens is used to correct squint.
- Vision test is done at 3 mts distance.
- Plastic lenses are highly recommended for low vision patients.
- Myopia should be fully corrected in the exotropic patient.
- All hypometric patients should be checked with cycloplegic refraction.
- Myopic shift occurs in Keratoconus.
- Myopic patients are corrected with contact lens only.
- Presbyopia is not a refractive error.
- Peripheral fields are recorded at Bjerrum screen.
- Head tilted to one side is one of the symptoms of Astigmatism.
III. Answer the following
- What is Myopia?
- What is Hypermetropia?
- What are the types of Strabismus?
- What are the types of Myopia?
- What are the types of Astigmatism?
- What is meant by Squint?
- Mention the normal limits of fields.
- What are the devices of Low Vision Aids?
- What are the different types of fields?
- Name the extraocular muscles.