Basic Ophthalmic Assisting Procedures
In any health care facility, for a doctor to make a diagnosis/ diagnoses, a detailed and accurate history must be elicited. History taking is recording the story of the patient 's medical disorder. History taking is a series of specific questions linked in an orderly sequence. The patient ' s history collection will be relevant to the condition of the patient and the requirements of the institution.
Two types of patients are seen in the Eye hospitals:
- The patient who desires a routine ocular examination combined with a refraction.
- The patient with the symptoms of ocular disorders.
The OA should find out to which category, the patient belongs. While collecting the data OA should know what is relevant and what is not relevant to the case. They should develop a good rapport with the patient and collect the necessary information .They should be precise and pertinent in acquiring patient's history. Some patients may have the habit of visiting the ophthalmologist several times. Sometimes the patient with multiple systemic disorders may say that they enjoy excellent health but when questioned may answer that they are taking pills for hypertension, iron tablets for anemia, injections for diabetes. The patient may not connect a general systemic disorder with an ocular problem. The systemic diseases may have serious or minor complications in the eye.
First the OA should make the patient feel comfortable, then the patients will share their complaints. The should not refrain from asking a particular question because it appears to be too private or embarrassing. If the history is conducted in a frank and professional manner and the questions are posed with tact and good taste, the patient will reveal even the most private matters, just as he or she would remove a shirt for chest examination. Some patients may refuse to speak to anyone except the physician about any eye problems. This is the patient's privilege. These patients should be treated more carefully and tactfully. They should not attempt to interpret a statement made by the patient. This will waste valuable time of the ophthalmologist.
History taking
There may be four types of history collection
- Problem focused
- Expanded problem focused
- Detailed
- Comprehensive
It is very important to note that the history has to be simple, clear and accurate. Each type of history may include some or all of the following elements.
- Patient 's present illness / chief complaint
- Present ocular history
- Past ocular history
- Present medical history
- Family ocular and medical history
- Occupational history
- Treatment history
Chief complaint / present ocular history
This is the reason the patient is seeking help from an ophthalmologist, except in those patients who come for the periodic evaluation or a follow up check. The patient may describe symptom and this is usually stated in the patient's words. To define the chief complaint they can ask the following questions to the patients.
- What are your symptoms?
- When did the symptoms start?
- Does the symptom seem to be getting worse?
Depending on the patientstated in the patient's answer they can ask for a chronological description of the development of the patient's present illness. It may include the following elements;
- Status of vision
- Onset of the symptom
- Description of the present symptom
- Treatment
To derive at these elements they can ask the following questions;
- Any change in vision? Decrease in distance or near vision? Has the vision been affected in one eye or both eyes?
- Did the symptom start all of a sudden or gradually?
- Is it stationary or progressive?
- Where exactly is the problem?
- Are symptoms constant or just occasional? If it is occasional, how long does it last? how often
- When does it occur? What is the severity of the problem? For example, if the problem is pain, ask whether the pain is sharp or dull ache?
- Does it get worse with other activity? Do the symptoms interfere with your work or other activities?
Ocular history
- Any previous eye injuries - what type?
- Any previous surgery - what type, when?
- Glasses / contact lenses
- Is there a past history of eye Problems? What type, when?
- Do you follow any prescription - Drops/ medicines for your eyes? What type, Dosage, frequency?
Medical history
- Are you suffering from Diabetes, High B.P, Heart disease, asthma, etc
- What are all the medicines you are taking?
Family history
Headache diseases that run in the family
- Document in the chart family history of diabetes, type and onset.
- High blood pressure, heart disease, strabismus?
Allergies
Can cause eye problems
- Possible causes of allergies - oral or topical drugs, environment (pollen, dust etc.)
- Medicines
- Over the counter drops
Patient complains of red eye
- How long has the eye been red-example 1day or 1month
- Any trauma to eye
- Foreign substance in eye (shampoo, dirt)
- Allergies
Questions to be asked to the patient suffering from red eye
- Pain and duration
- Irritation -F B sensation
- Itching
- Sensitivity to light (photophobia)
- Discharge present or absent
- Colour of the discharge - clear, white or yellow white
- Decrease in vision
- Any treatment taken
- Headache, vomiting
- Application of any medicene
Diagnosis to consider
- Conjunctivitis
- Iritis
- Angle closure glaucoma
- Contact lens over wear - sleeping in DWSCTL
- Dry eyes
- Post-op iritis
- Pingecula
- Pterygium
- Subconjunctival hemorrhage
- Penetrating foreign body or injury - if patient is carpenter or lathe worker
- Blepharitis
- Trichiasis
- Foreign body in eye - dust or stone particles, flying iron dust
Patient complains of decreased vision - Questions to be asked
- Duration of blurred vision
- Gradual or sudden loss of vision
- Defective vision -distance, near or both
- Is it during the day or night time
- Stationary/progressive
- Whether painful/painless
Diagnosis to consider
- Cataract
- Onset of presbyopia
- Optic neuritis
- Retinal detachment
- Diabetic retinopathy with CSME
- Vitreous haemorrhage
- Hx of diabetes - is BS under control?
Tips to win confidence of the patient
- Appearance
- Cleanliness and neatness
- Lab coat if possible
- Handling of patients
- Attentiveness to the patient's complaints without contradicting
1. Show concern by observing the following:
- Introduce yourself (My name is .................., I will be working with you for a few minutes to record your ocular problem).
- Explain: in order to get the best care and treatment from your doctor, I need to record a few important facts regarding your eye problem.
- Attitude toward patient: be friendly, be sensitive, and smile. Treat them cordially, so that they feel you are interested in them as a total person and not just in their eye problem.
2. Why is this important?
- By having a good relationship with your patient, you are more likely to be successful in winning your patient's trust.
- Therefore he/she will have confidence in you and will feel comfortable in sharing his/her history with you, thus saving the doctor some valuable time.
3. Why there is a need for an accurate record of the history?
- Story (with systemic ramifications) regarding insulin / penicillin. Technician asked patient if she had any allergic reactions to medications. Patient replied," Yes, penicillin " Technician recorded in the patient's chart as "Insulin". After surgery the patient developed an infection and penicillin was prescribed by the doctor. He was not aware of her allergy because of the incorrect history record. The patient almost lost her life due to this error. Her relatives wanted to know why the doctor had not observed her allergy and they checked the record and found out that insulin had been mistakenly recorded.
- Story (with ocular ramifications) regarding Diamox / Diuril. Technician asked patient, "What medication are you now taking?" The patient was taking Diamox for a severe glaucoma condition. But the technician recorded Diuril in the chart (which is also a diuretic, but it does not lower intraocular pressure like Diamox). After surgery the doctor ordered the patient to continue with her regular medications. When she looked at the chart, she noted Diuril (not Diamox) and followed the doctor's orders. The patient's intraocular eye pressure increased over a period of several days causing some glaucomatous damage (to the optic nerve and thus causing the vision to decrease). Finally the error of the OA 's history taking was discovered and appropriate medication was given, but damage to the optic nerve resulted from this mistake was irreversible.
- History taking must be concise and to the point by observing the following suggestions.
What can be learnt from these two examples?
- Listen carefully to your patient.
- Repeat the patient 's answer to your question so he/she can clarify the answer, if you heard it wrong or mistakenly put down a similar sounding medication. We are dealing with people's quality of life as well as their very life and so it is important to get it right in their record.
- Take notes on paper as the patient tells you about his/her problem. Look them in the eye to let them know that you are interested and concerned about their problem. Then organize the information in chronological order (arranged in order of occurence). The doctor will appreciate this very much.
- Write down the pertinent facts on the medical form in order of occurrence. Leave out all the unimportant information that the patient may tell you. Some times the patients will go into great detail and much of this does not apply to the chief complaint. Sometimes the patient needs to get someone's listening ear, therefore, be polite but guide the patient back to the chief complaint. The doctor will be appreciative if you let the patient unwind with you and not take his valuable time.
- Put the following facts in the patient's record:
- Chief complaint: brief description of the problem; indicate which eye(s).
- Present ocular illness: When did it start (over a period of time)?
- Duration: Complaints can change, such as light flashes, then floaters, then half of the vision is gone and the patient only sees a black shadow in half of his visual field. Start with the distant time: for example 1-1/2 years, and work toward the present time- 9 months, 6 months, 3 weeks, yesterday, today, etc.
Past history
- Diseases: Diabetes, tuberculosis, high blood pressure, etc., and dates when they were first diagnosed should be noted in the chart (duration in months/years)
- Operations: Cancer, appendectomy, Caesarian-section, retinal reattachment, trabeculectomy for glaucoma, laser for diabetic retinopathy, etc., plus approximate dates.
- Medications: Insulin, Digitalis, Eltroxin, Diuretics, Aspirin, etc.). Sometimes they will not know the name of the medication; but they may describe the color and the size of the pill or capsule and how often they take it and for what problem (breathing, heart, arthritis, etc.,). Do not assume the name of the medicine and come to your conclusion. If the patient is not in a position to tell the name of the medicine, right the same in the record.
- Allergies to drugs and foods.
- Family history: (Blood relatives living or dead who have had blindness or any eye disease).
Emergencies : ( which, what, when, where, how, and duration of symptoms?)
- Which eye?
- What happened? (Chemical or foreign body in eye, etc.)
- When did it happen?
- Where did it happen? (On job or at home)
- How did it happen?
- How has the injury affected your eye(s)? (can't see, pain, blurred vision, double vision, etc.)
- Duration of symptoms? (One hour-emergency/ conjunctivitis for three weeks-take the whole history)
- Needs to see the doctor immediately, soon, later today?
Assignment
" 24 HOURS " - Choose someone you love and respect (mother, father, a sister, a brother, a cousin, a very good friend) to be your constant companion. Pretend that person hears what you say to others, sees and hears how you react to other's treatment of you (either good or bad) and see if this makes a difference in your daily behavior towards other people. If you take this assignment to heart, it will change your attitude and you will become a more sensitive and positive thinking person with whom people will enjoy associating. It will also make a difference in how you treat your patients.
Key points to remember
A systematic order should be followed in taking an adequate history. Here are some of the tips in history taking:
- Identify the chief reason the patient has sought an eye examination
- Identify any secondary problems the patient has that are referable to the eye
- Identify any systemic or general illness the patient presently has and any medication being taken
- List past ocular disorders or operations
- Determine if the patient is wearing contact lenses or spectacles, and if so, how old they are and when the last eye examination occurred
- Be brief but also go into detail with any specific ocular problems that arise. General questions regarding any abnormality may be important, such as time and duration, family involvement, and so on
- Record any previous therapy and the response
- Never talk ill about any treatment taken outside or about the doctor who has treated the patient
Medical terminology
| VA | - visual acuity |
| RX/CTL | - treatment/contact lens |
| B.P | - blood pressure |
| FB | - foreign body |
| DWSCTL | - daily wear soft contact lens |
| CSME | - cystoid macular edima |
Student exercise
Say true or false
- History taking is a confidential experience with the patient and the OA who is involved (True / False)
- The most significant question is what medication are you taking? " (True / False)
- The patient should be allowed to speak freely of all their problems (True / False)
Answer the following question
List and describe the essential elements of a complete problem oriented medical case history.
Visual Acuity
Vision testing
Definition
Acuity of vision is defined as the smallest object or letter that can be clearly seen and distinguished at specified distances.
Types of visual acuity
- Distant visual acuity
- Near visual acuity
- Pinhole visual acuity
a) Visual acuity distance
Definition: The ability of a person to distinguish an object or letter whose rays are parallel and where no accommodation is required.
For all practical purposes 6 meters or 20 feet is used for distance visual acuity testing as the rays are considered parallel and no accommodative efforts are required
Various distant visual acuity charts are
In adults
- Snellen chart
- Log MAR chart
In illiterates
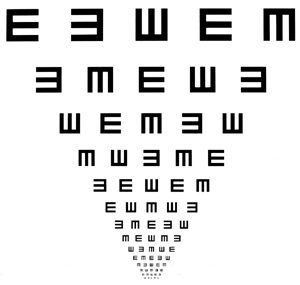
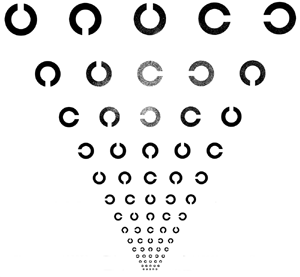
- E - chart (Fig. 10.1)
- Landolt's broken rings chart (Fig. 10.2)
- Multiple pictures chart
In children
- Cake decorations
- Sheridon-Gardinel testing
- Keeler's preferential looking tests
- Cardiff charts
b) Near visual acuity
Definition: The smallest objects or letter that can be distinguished clearly at a normal reading distance. For practical considerations the normal reading distance is considered to be 40cms (Fig. 10.3).
Snellen near acuity charts are used; near vision is graded from N5 to N48 (Fig. 10.4).

Pinhole visual acuity
To be done for all patients with less than 6/6 vision.
- Reduces the peripheral rays and allows the central rays alone to reach the retina.
- Increases the contrast of vision
- Helps in attaining 6/6 vision following vision loss due to refractive error.
- Helps in differentiating visual loss correctable by spectacles and other disorders
Practical considerations
Distant visual acuity testing
The Snellen chart
Principle: This procedure measures the patient's distant vision by testing his/her ability to read a character at a standard distance from a specified chart. The size of the letter is standardized so that the letter in each row should be clearly legible at a graded distance to a person with normal vision.
Equipment necessary
- Snellen distant visual acuity chart with a good illuminating source
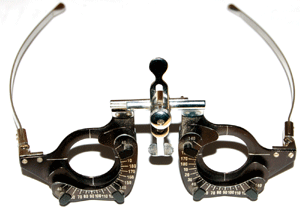
- Trial frame (Fig. 10.5)
- Occluder (Fig. 10.6)
- Pin hole

Procedure
- Explain the procedure and its importance to the patient and try to win their confidence
- The patient is seated comfortably at 6 metres distance
- The chart should be at the eye level of the patient
- Check the visual acuity of the patient without glasses first followed by with the present glasses if any.
- Occlude one eye and test the visual acuity individually (separately)
- Instruct the patient to read from left to right each line and observe
- Encourage the patient as this may give more accurate results
- Test for visual acuity with pinhole if vision is less than 6/6
- Interpret the visual acuity and record it in the case sheet for each eye separately
Interpretation of visual acuity
- Visual acuity is recorded as a fraction. The numerator indicate distance in meters at which the patient can read clearly the smallest possible letters/characters in the chart. The denominator indicates the distance in meters at which a normal person can see the same letters/characters in the chart.
- Normal visual acuity is 6/6.
- If the patient is unable to read 2 letters of last line it should be indicated as 6/6 - 2
- If the patient is unable to read last line at 6 meters but reads the previous lines then visual acuity is 6/9
- If they are unable to read last two lines but able to read others visual acuity is 6/12
- If unable to read last 3 lines then visual acuity is 6/18
- If unable to read last 4 lines then visual acuity is 6/24
- If the patient can read only the first 2 lines the visual acuity is 6/36
- If they can read only the first line visual acuity is 6/60
- If the patient is unable to read the first line the visual acuity is less than 6/60
- Then patient may be asked to go forward to read the first line. The distance from the chart from which the patient can read clearly the first line of the chart is considered the numerator e.g., 4/60, 3/60 etc.,
- Instead the OA may ask the patient to count fingers and the farthest distance at which the patient can count fingers is taken as numerator. E.g. 4/60,3/60 ½ meters / 60, etc.
- If the patient is not able to appreciate counting fingers, then patient may be tested whether they appreciate movements of hand close to face. If the patient can appreciate then the visual acuity is HM or hand movements
- If patient cannot appreciate HM then a strong source of light may be shined from different directions. If patients can perceive light and can accurately point out directions projection with perception of light (PL+ and PR accurate) may be recorded.
- If the patient perceives light but is unable to point out to the direction of the light then the visual acuity is perception with inaccurate projection (PL + PR inaccurate)
- If the patient is unable to appreciate light then the visual acuity is no perception of light or No PL
- The OA should create a good rapport with the patient so that they feel comfortable, particularly the uncooperative patients.
- The OA should be humble and explain the procedure to the patient in a proper way in patient's own language.
- They should identify the appropriate chart for each patient. E.g. E-chart, picture chart etc.
- They should be responsible to arrange the necessary equipment to carry out the procedure.
Do's and Don'ts
- Each eye should be tested separately
- Test with and without glasses separately
- Observe whether the patient misses letters on particular side, like temporal half or nasal half
- Don't irritate the patient if they are unco- operative, instead try to gain their confidence.
- Observe whether the illumination is adequate.
- Never allow the patient to open/close the eye partially or squinting of eyes, which may alter the visual acuity.
Key points to remember
- Test each eye separately
- Make sure illumination is adequate and patient is seated comfortably at 6m distance from the chart.
- Test pinhole acuity in all patients with vision less than 6/6 with correction
Student exercise
Fill in the blanks
- Normal visual acuity is _______.
- Near visual acuity is tested at a distance of ____________cms.
- If the patient is able to read only the first two lines then their visual acuity is________.
- Visual acuity charts used in children are ________ and _________.
True or False
- Sherdran - gardinel chart is used to test visual acuity in adults.
- Distant visual acuity using Snellen chart is done at a distance of 8m
- Pin hole visual acuity helps in differentiating visual loss corrected by spectacles and others which cannot be corrected by spectacles.
Answer the following
- What is visual acuity? What are its types?
- What is the use of testing pinhole visual acuity?
Instillation of eye drops
What are eye drops?
OAs commonly assist the ophthalmologist by instilling eye drops in patients' eyes. Eye drops are drugs in liquid form that are applied in the eye (topically).Diagnostic types of eye drops are used during certain eye tests; therapeutic eye drops are used to treat ocular conditions or diseases.
Forms of ocular topical medicines
Ocular medications are formulated in three forms: as solutions, suspension, and ointments.
Solutions
These are in liquid form and usually they are instilled into the eye. In a solution, the active drug is completely dissolved in an inactive, transparent vehicle. The solutions are clear.
Suspensions
In a suspension, particles of the drug are visibly suspended in a liquid. The fluid is cloudy or milky, unlike a solution, which is clear. Shake the suspension well before use.
Ointment
Contains a drug added to an oil base. The ointment melts and is absorbed into the tissues.
Types of doctors order
- Written order - are the accepted type of order
- Verbal orders - are accepted in an emergency situation but are to be written as soon as the emergency is over.
- Telephone orders - are accepted in many institutions. Whoever speaks with the doctor over the telephone writes it in the appropriate place along with the name of the doctor and the signature of the person receiving the order. The telephone order must be read back to the doctor for confirmation. It must be signed by the doctor when he/she comes to the unit.
- Standing orders - they are to be carried out whenever a certain condition exists. For eg. Pre-operative eye drops for cataract.
- Stat orders - one that is given immediately and only once.
- PRN orders - It may be given as and when necessary.
Safety in administring eye drops
- Eye drops should be kept away from the reach of children.
- Follow the " 5 Rights " in administering eye drops. The " 5 Rights " are:
- The Right eye drop
- The Right dose
- The Right route
- The Right time
- The Right patient
The right patient involves positively identifying the patient. Special care must be taken when there are two or more people with the same name, in the same room or unit.
- Always check the expiry date of the eye drops before use.
- Check the label before administering and after administering the eye drops.
- Do not use if the colour has changed or if there is any turbidity in an eye drop.
- If the patient refuses to have eye drops instilled or it is omitted for any reason, it should be recorded in the patients case sheet along with the reason.
- Do not use if there is any damage to the bottle or if the nozzle cap is lost.
- It is possible for errors to happen. As soon as it is realised, check the patient's eye and immediately notify the doctor.
Common abbreviations used
| Q.d. | - Once a day |
| b.d. | - Two times a day |
| t.i.d/t.d.s | - Three times day |
| q.i.d | - Four times a day |
| prn | - Whenever necessary |
| Stat | - Immediately, once |
| Q6H | - Every six hours |
| A.C. | - Before meals |
| P.C. | - After meals |
| H.S. | - At bed time |
| E/D | - Eye drops |
| Oint | - Ointment |
Practical
Steps and techniques in administering eye drops /ointment
- Collect the necessary equipment to administer eye drops
- bottle with sterile forceps
- Necessary eye drops / ointment
- Jar with cotton wipers
- Kidney tray
- Sterile pads and bandages.
- Identify the patient by comparing the information in the case sheet
- Explain the procedure to the patient and explain if any discomfort is to be expected
- Bring the prepared tray to the patient's bedside.
- Wash hands thoroughly and dry with a clean towel
- Place the patient in a sitting position with his head tilted back or in a supine position with neck extended back over a pillow. Ask the patient to look up. Give them a cotton wiper to hold.
- If the patient has crusts or exudates around the eye, clean the eye with sterile wiper, then apply drops / ointment
- Open the eye drop container. Hold the container with the nozzle pointing downwards.
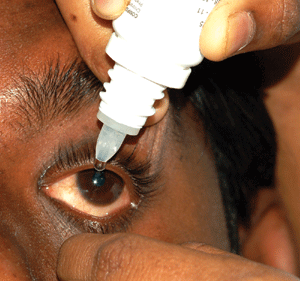
- The pouch technique (Fig. 10.7)
- Make a pouch in the lower fornix by pulling the lower lid away from the globe. Instill one or two drops / ointment directly into the pouch. Instruct the patients to close their eyes gently. Give the patient the cotton wiper to hold and remove excess medication and tears.
- Replace nozzle cap properly.
- Wash hands
- Record eye drops in the case sheet.
- Do not apply more drops / ointment as it may increase systemic absorption and toxicity and drug wastage
A clean tray containing
Exercises
Key points to remember
- Always check the doctors order before administering any eye drop
- Follow the five rights in administering eye drops.
- The tip of the bottle should not touch the eye or elsewhere.
- Always remember to check the expiry date of the eye drop.
Student exercise
Say True / False
- Mydriatics could be given to patients with acute angle closure glaucoma.
- Anaesthetics: do not use in patient with history of hyper sensitivity to the drug.
- Do not use if there is any damage to the bottle or if the nozzle cap is lost.
- Always check the expiry date of the eye drops before use.
- Steriods: do not use in patients with acute infections.
| Classification of Drops | uses | Action | Adverse Effects | Points to Remember |
| Mydriatics & Cycloplegics Eg:Atropine, Homatropine, Tropicamide, Cyclopentolate | - Used in patients undergoing examination of the fundus - Used in refraction examinations that require the absence of accommodation (changing the curvature of lens to focus images of near objects). - They act as pain relieving agents in some patients by preventing spasm of the ciliary muscles e.g. eye injuries, corneal ulcers, uveitis | Mydriatics usually dilate the pupil by stimulating the iris dilator muscles or inhibiting the constrictor pupillae - A temporary paralysis of the ciliary muscles is caused by cycloplegics |
- Irritability, ocular congestion with long-term use. - Photophobia | Do not uses in patients with acute Angle closure glaucoma. |
| Anaesthetics Eg: Xylocaine Lignocaine | Used to anasthetise during diagnostic procedures Ex: hypertonometry, gonioscopy, and any other examination that involves touching the surface of the eye. | - It produces local anesthesia in the eye instilled instillation. - It anaesthtises the eye in which it is instilled |
- Burning sensation for 30 seconds after initial - Allergy develops with repeated use. | - Do not use in patient with history of hypersentivity to the drug - Warn patient not to touch or rub the eye after instillation, since this may cause corneal abrasion. |
| Antibiotics Eg: Chloram phenicol Gentamicin, Tobramycin, Natamycin | Used to prevent and treat ocular infections | Bactericida (kills the bacteria) or Bacteriostatic. (prevents multiplication of bacteria) | Local Burning, discomfort, itching, conjunctival hyperemia, bad taste | Avoid in patients with history of hypersensitive reactions to antibiotics |
| Steroids Eg: dexamethasone , prednisolone | used seperately or in combination with antibiotics to prevent and treat any ocular inflammatory conditions of inflammations. | Decreases the inflammatory reaction by decreasing the infiltration of WBC ' s at the site - Secondary infections. |
- Corneal ulceration, increased intraocular pressure. (Glaucoma ) and cataract with excessive long term use. | - Shake the suspensions well before use. - Do not use in patients with acute infections. |
Further study
- Collect and read the package literature of eye drops commonly used in your hospital.
- Write an assignment about the different groups of eye drugs, actions and side effects.
- Demonstrate the procedure of administering drop on classmates and correct each other.
Measurement of intraocular pressure using the Schiotz tonometer
Definition of intraocular pressure (IOP)
- Intraocular pressure refers to the pressure exerted by the intraocular contents on the coats of the eyeball.
- It is maintained by the equilibrium between the aqueous humour formation, its outflow and the episcleral venous pressure.
Normal IOP values
- Ranges between 10.5 and 20.5mm of Hg
- Mean IOP = 15.5 + 2.5mm of Hg
- Increase in IOP more than normal values is glaucoma
Measurement of IOP
1. Direct measurement (Manometry)
- Here a needle is introduced into the anterior chamber and is connected to a suitable mercury manometer.
- Disadvantage: Not a practical method for routine IOP measurement.
2. Tonometry or Indirect method:
- It is an indirect method of measuring IOP with instruments called tonometers.
- Types of Tonometer:
- Indentation or Impression tonometers (eg: Schiotz)
- Applanation Tonometers (eg: Gold-mannn Applanation tonometer)
We shall confine ourselves to Schiotz tonometry. Schiotz tonometry devised in the year 1905.
Principle
Schiotz indentation tonometer works on the fundamental fact that the plunger will indent a soft eye more than a hard eye.
Parts of a schiotz tonometer
Schiotz tonometer consists of the following
- Handle for holding the instrument in vertical position on the cornea.
- Foot plate which rests on the cornea.
- Plunger which moves freely within a shaft in the foot plate.
- A bent lever whose short arm rests on the upper end of the plunger and a long arm which acts as a pointer needle. The degree of indentation is shown by the movement of this pointer over a scale.
- Scale
- Weight of 5.5gm is fixed to plunger. Extra weights 7.5gm and 10gm are included.
Chart provided for IOP calculation by Schiotz tonometer (Friednwalds chart)
| Schiotz Scale Reading | IOP in mm of Hg with different plunger body weights | |||
| 5.5gm | 7.5gm | 10gm | 15gm | |
| 3.0 | 24.4 | 35.8 | 50.6 | 81.8 |
| 3.5 | 22.4 | 33.0 | 46.9 | 76.2 |
| 4.0 | 20.6 | 30.4 | 43.4 | 71.0 |
| 4.5 | 18.9 | 28.0 | 40.2 | 66.2 |
| 5.0 | 17.3 | 25.8 | 37.2 | 61.8 |
| 5.5 | 15.9 | 23.8 | 34.4 | 57.6 |
| 6.0 | 14.6 | 21.9 | 31.8 | 53.6 |
| 6.5 | 13.4 | 20.1 | 29.4 | 49.9 |
| 7.0 | 12.2 | 18.5 | 27.2 | 46.5 |
| 7.5 | 11.2 | 17.0 | 25.1 | 43.2 |
| 8.0 | 10.2 | 15.6 | 23.1 | 40.2 |
| 8.5 | 9.4 | 14.3 | 21.3 | 38.1 |
| 9.0 | 8.5 | 13.1 | 19.6 | 34.6 |
| 9.5 | 7.8 | 12.0 | 18.0 | 32.0 |
| 10.0 | 7.1 | 10.9 | 16.5 | 29.6 |
Practical usage of Schiotz tonometer
- Always check the instrument before usage and calibrate
- Wash and dry your hands before working with the instrument.
- Explain to the patients that you will be touching eye with an instrument but they will not feel any pain.
- Administer one drop of lignocaine eye drop to the eye(s) to be tested.
- Allow 2 to 5 minutes for the local anesthetic to act.
- Patient should lie supine.
- Rest your fingers only on the bony orbital rim and not over the eye ball.
- Gently separate the lids.
- Ask the patient to hold their hand up and look at the thumb or a finger to give them a point of fixation.
- With the tonometer having no added weights (the instrument weighs 5.5gm) rest the foot plate on the centre of the cornea.
- Look at the scale of the tonometer to find out the degree of indentation. If it indicates 3 or less, put the next heavier weight on the plunger. When the scale reading is > 4 it is an ideal indentation.
- Use the provided Friedenwalds conversion table for estimation of IOP 'S.
- Record the readings for each eye separately in the patient's chart.
Maintanence and sterilisation of Schiotz tonometer
- Keep the instrument covered within the case while not in use.
- Ensure proper functioning of the instrument before each IOP recordings and calibrate.
- Calibration: Place the foot plate on the model cornea provided in each case. Scale reading of zero ensures proper calibration.
- Always sterlize with an antiseptic solution the part of the instrument that will come in contact with the patient's eye.
- Allow three minutes for the alchol (sterlizing agent) to dry to prevent alcohol keratitis.
- After the measurement remove the weights and unscrew the plunger to clean thoroughly.
- The foot plate of the Schiotz tonometer may also be sterlized by flame sterlization.
Attitude
- Communicate well with the patient to reduce anxiety.
- Clear the doubts of the patient by answering all their questions.
- Assist the patient to maintain a comfortable position throughout the procedure
- Handle the equipment with care.
- Communicate the necessary information to the ophthalmologist
Key points to remember
Do's in measuring IOP by Schiotz
- Explain the procedure and its importance to the patient in their own language in a gentle way.
- Always wash and dry your hands before working.
- Be gentle while separating the eyelids
- Take two to three readings when you find the values are abnormally low or high.
- Special care is required in eyes which are swollen from surgery or injury. In patients who are unable to open their eyes voluntarily or when the patient is uncooperative, reassure the patient and resume work gently.
Dont's in measuring IOP by Schiotz
- Do not rest your fingers over the globe.
- Do not do indentation tonometry in a red and inflammed eye or eyes with conjunctivitis, corneal pathology, foreign body or in dry eye
Advantages of Schiotz tonometry
- Simplicity of the instrument
- Good reliability
- Low price
- Reasonable accuracy
- Easy usage
- Easy transportability
Disadvantages of Schiotz tonometry
- Patient has to lie supine
- Operater variability
- Cannot be done in patients with corneal pathology or infections or changes in ocular rigidity.
- Errors in recording IOP
Sources of errors in performing IOP by Schiotz tonometer
- Contraction of extraocular muscles.
- Accomodation
- Ocular rigidity
- Variaitons in corneal curvature and thickness
- Scale reading and faulty technique
Self evaluation
- Prepare a patient for schiotz tonometry.
- Interpret schiotz scale using friednwalds chart.
- Sterlize a schiotz tonometer.
- State the advantages and disadvantages of schiotz tonometer.
Student exercise
I. Fill in the blanks
- The normal IOP ranges from ___________ to _____________.
- Goldmann tonometer is an example of ________ tonometer.
- Extra weights are added to Schitoz tonometer when the scale reading is less than _____________.
II. True or False
- Schiotiz tonometer is a type of indendation tonometer.
- Acetone is used to sterlize schiotz tonometer
- Ocular rigidity can cause false high reading with Schitoz tonometer.
III. Match the following
- Monometry - Indendation
- Schiotz tonometer - Applanation
- Goldmann tonometer - Direct method of measuring IOP
Answer the following
- What is the normal IOP value ?
- What is schiotz tonometer? What are its parts?
- How will you measure IOP using schiotz tonometer?
- How will you sterlise Schotiz tonometer?
- What are the advantages and disadvantages of Schiotz tonometer?
Dressing preparation
Dressing is done post operative for the patient to avoid dust, infection and prevent injury.
Materials required for preparing wiper
- Clean round basin
- Distilled water
- Clean cotton
Practical
Dressing tips
- Before preparing the bandage look around and see whether the place is neat and tidy.
- They should clip the nails before the preparation of bandage.
- Wash the hands thoroughly with soap and wipe on a clean towel.
- Spread a clean bed cover and sit on it comfortably
I. Wiper preparation method
- Pour the distilled water in a basin.
- Immerse the clean pieces of cotton into the water
- Take a small round ball (marble size) of cotton from the water.
- Roll the cotton into a square shape.
- Take some more cotton and keep it on the square cotton and roll it gently in a length wise direction so that a clean wiper is prepared.
II. Cotton bandage preparation method
- Spread a mat in a clean room
- Take the gauze piece from the packet and spread it on the mat.
- Cut the gauze into nine pieces
- Take the cotton roll and keep it in the right hand. Place the cotton into the gauze piece and wrap it tightly.
- Cut the cotton wrapped gauze into 4 rectangular pieces (measurement can be the length of your pointer finger).
- The other wasted cotton pieces should be utilized to prepare small balls of cotton used for wiping the patient's eye at the time of instilling drops.
- From 1 roll of cotton 120 cotton bands could be prepared.
III. Bandage tying cloth- preparing method
Materials required for preparing bandage strips
- Clean Mat
- Scissors
- Bandage cloth roll packet
Method
- Spread a mat in a clean room
- Take a roll of bandage and fold it into two at forearm measurement
- Trim the ends of the bandage.
- Keep one end long and the other end short and cut to the size of the ear.
Note: We can prepare 8 strips of bandage from one bandage roll.
Points to remember in preparation of wiper, bandage strip and bands
- Right place (where there is less pollution, no people walking here and there)
- Right size / measurement
- Right method
Points to Remember
All the procedures and methods involved in dressing preparation technique must be followed carefully.
Bandage tying
Bandaging of the eye
A bandage is applied to prevent movement of the eyelids, to assist in healing of corneal abrasions and after operations.
Method
Ask the patient to close both eyes gently and place eye pad and shield over the affected eye. Standing in front of the patient, start with a turn round the cheek on the affected side and take the bandage one turn round the head, placing the patients ear through the hole in the bandage continue with turns round the cheek. Finish with one turn round the head and tie the bandage securely on the forehead. Ask the patient if the bandage feels comfortable before leaving him.
Take two pads
- Fold the first pad in half. Then place it over the eye with one hand and hold it in place.
- With the free hand, apply the second pad over the first.
- Place the plastic shield over the two cotton pads. Apply a single piece of tape at an oblique angle just above the brow of the opposite eye.
- Firmly press the tape against the skin medial to lateral so that 6 to 7 centimeters of tape contact the skin above the cheekbone and forehead.
- A long piece of bandage cloth measuring 1m x 10 cm can be tied over it.
- It should be tied just tight enough to secure the pad properly. The knot should come on the forehead and it should be neatly trimmed. (Knot on the side interferes with the sleeping posture of the patient).
Do's
- Explain the procedure and gain the co-operation from the patient.
- Handwashing should be done prior and after applying a bandage.
- Apply the bandage with gentleness
Don't
- Don't apply wet bandage
- Don't apply bandage on wrong eye
- Don't use unsterile dressing
- Don't apply too tight or too loose
- Don't cover other eye with the bandage
Student exercise
I. Fill in the blanks
- One can cut _________ pieces in a bandage roll
- One can prepare ____________ number of cotton strips from a cotton roll.
II. Say True / False
- When you spread a gauze piece it can be cut into 3 pieces
- Cotton wipers must be prepared from cotton dipped in distilled water
- From a roll or cotton 5 cotton bands could be prepared
III. Answer the Question
- What are the materials required in the preparation of cotton wiper, cotton band and gauze stripe?
