Microbiology
Microbiology is the study of microorganisms, which includes bacteria, viruses, fungi and parasites. These living organisms are so small that they are invisible to the human eye and can be seen only with aid of microscopes.
Infection is a term which refers to invasion and multiplication of harmful microorganisms in body tissues. Though human beings live surrounded by a sea of microorganisms, only some of these are harmful. Disease caused by harmful microorganisms is termed infectious diseases.It can affect any part of the body including the eye.
The role of OA in dealing with infectious diseases of the eye is to know about various micro organism causing infections, the types of infections caused by them and methods to prevent spread of infection.
This chapter on basic microbiology gives information about the various microorganisms causing infection and the types of infection caused by them. The topic on infection control covers sterilisation and disinfection procedures used in the operation theatre and in the ward.It also covers hand-washing procedures, which help to prevent transmission of disease causing microorganisms from one person to the other.
Basic microbiology
Microbiology is a study of microorganisms, living things which can be seen only with the aid of a microscope. It studies the causative agents of infectious diseases and the methods of protection against such diseases. There are many different species of microorganisms, only a fraction of these cause disease in humans. Disease - causing micro- organisms are called pathogens. These include bacteria, viruses, fungi and parasites.
Bacteria
These are unicellular organisms; i.e. they are composed of one cell only. Reproduction occurs by simple binary fission. This means that each cell divides to form two, both of which divide in turn and so on. In order to multiply, bacteria require a favorable environment. Pathogenic bacteria survive best in the sort of environment that the human body provides. This includes a temperature of 37o C, moisture, supply of food and slight alkalinity. Some bacteria require a supply of oxygen, these are known as aerobes. Others can only survive in the absence of oxygen. These are called anaerobes. Some bacteria have the ability to change into a form, which is extremely resistant to adverse conditions. This resistant form is known as a spore.
Products of the bacteria cause much of the effect of bacterial infection on the body. These harmful products are called toxins; when released they circulate in the blood stream. In a severe infection they cause serious symptoms, collectively referred to as toxemia.
Classification of bacteria
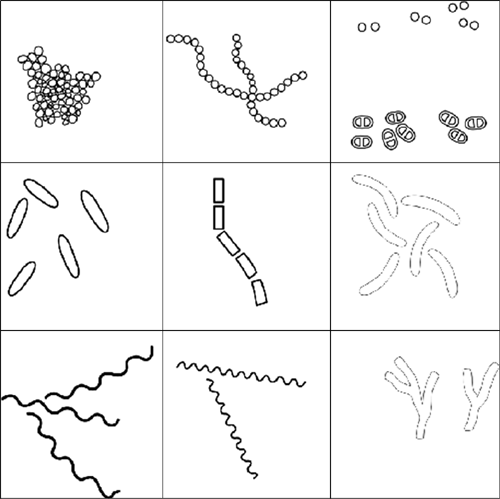
The importance of classification lies in the need to be able to identify bacteria so that the most effective methods can be used to prevent spreading and to treat infections. Shape of bacteria is the most elementary method of classification (Fig. 5.1).
Cocci: These are spherical or oval shaped bacteria.
Bacilli: These bacteria are rod shaped.
Spirochetes: These are corkscrew shaped or spiral bacteria. The coils of the spiral may be either tight or loose.
Vibrio: Comma shaped or curved rods.
Actinomyces: Branching filamentous bacteria.
Another simple method of classifying bacteria is by Gram's staining, which divides them into Gram positive and Gram negative bacteria.
Culture media
Bacteria and fungi have to be grown (cultured) to be identified. For growing this bacteria and fungi, we use a special preparation called media.
Different media are:
- Blood agar (BA) - For growing various bacteria
- Chocolate agar (CA) - For growing various bacteria
- Sabourad's Dextrose Agar (SDA) - For growing fungus
Gram positive cocci
1. Staphylococcus aureus
Gram positive cocci occur in grape like clusters. They are the most common cause of suppurative infections in humans. They commonly colonize on the skin, in glands, and mucous membranes of humans and animals. Staphylococci are common in hospital environment and cause infections like boils, wound infections, food poisoning, pneumonia, septic arthritis, corneal ulcer and endophthalmitis.
2. Streptococcus pyogenes
Gram positive cocci arranged in chains or pairs normally present in the human upper respiratory tract - throat, nasopharynx or nose of patients and carriers. Crowding is an important factor in the transmission of infection. Transmission of infection is either by direct contact or through airborne droplets, contaminated dust or fomites. Infections caused are tonsilitis, otitis media and rheumatic fever.
3. Streptococcus viridans
This bacterium is normally found in the mouth (commensal) where it does no harm. It enters the blood stream after dental extraction. Infections caused are dental abscess and subacute bacterial endocarditis where heart valves have previously been damaged.
4. Streptococcus pneumoniae
Pneumococci are Gram-positive diplococci, which are normal inhabitants of the respiratory tract. They are transmitted from one to another by inhalation of contaminated dust droplets or droplet nuclei. Spreading is facilitated by crowding of people. Pneumococcus is one of the most common organisms causing ocular infections like endophthalmitis, dacryocystitis and corneal ulcer. They also cause otitis media, meningitis and pneumonia
Gram-negative cocci
Neisseria (Meningococcus and Gonococcus)
Gram negative diplococci: Transmission is essentially by airborne droplets. They cause serious infections in children and adults. In ophthalmology, conjunctivitis (ophthalmia neonatorum) in newborns is a severe infection caused by gonococcus. They also cause keratitis and endophthalmitis.
Gram positive bacilli
1. Cornyebacterium species
Commonly known as diphtheroids. They are normal commensals living mainly on skin and mucous membranes. Diphtheria is a serious infection caused by them. They also cause membranous conjunctivitis.
2. Bacillus species
This organism produces highly heat resistant spores and is aerobic. They are present in soil, dust, water and air and are common contaminants. Bacillus anthracis causes the deadly disease anthrax. It also causes anthrax of the lid and conjunctivitis.
3. Clostridium species
They produce spores and are anaerobic. This bacterium is found in both animal and human faeces and in soil and dust. Spread is by direct contact of wounds with soil, dust and faeces. Clostridium tetani causes tetanus, clostridium Welchi causes gas gangrene and food poisoning.
Gram negative bacilli
Some bacteria are
- Escherichia coli
- Klebsiella
- Proteus
- Pseudomonas
- Salmonella species
- Shigella
Most of these bacteria are responsible for diarrhea, dysentery, food poisoning, typhoid and wound infections.
Pseudomonas is important in ocular infections because it causes keratitis and endophthalmitis which is difficult to treat. These bacteria are found in human intestines, soil and water. It survives in disinfectant bottles, respirators and humidifiers. It is spread by direct and indirect contact. Infections caused are wound and burn infections, urinary tract infections and septicemia. It is resistant to many antibiotics and is a problem in many hospitals.
Nocardia asteroids
They are usually saprophytes in soil and live freely in nature. Infection is acquired mainly by soil contamination following injury. Common ocular infections caused are conjunctivitis, corneal ulcers and endophthalmitis.
Mycobacterium tuberculosis
Mycobacterium tuberculosis is the causative agent for the disease tuberculosis, which is spread by droplet transmissions (coughing). The disease can be diagnosed by seeing the bacilli in sputum stained by Zeihl Neilson acid fast stain. It appears as pink rods and normally treated with multiple drugs (4 drugs) for 6 -12 months. Because of increase in HIV infection, tuberculosis is also increasing.
Fungi
Fungi have been recognized as causative agents of human disease from very early times. Fungal infections are very common and some of them cause very serious and even fatal diseases. Most fungi are present in the soil as saprophytes and human infections are mainly opportunistic. It is very difficult to treat fungal infections. We have to use antifungal drugs for a very long time.
The different diseases caused by various fungi
- Infections of hair skin and nails known as tineas. It is caused by dermatophytes.
- Candida albicans is common in diabetic patients and patients taking antibiotics or corticosteroid treatment over a long period as it suppresses the normal flora. In ophthalmology, candida causes corneal ulcers and endophthalmitis. It also causes oral thrush, vaginitis and other systemic infections.
- Many other fungi like aspergillus, fusarium, and penicillium are very common especially in ocular diseases like corneal ulcers and endophthalmitis.
Viruses
Viruses are smaller than bacteria and can be seen only by an electron microscope. There are numerous types of viruses which commonly cause infections in humans: poxvirus, herpes virus, adeno virus, hepatitis virus, polio, mumps, measles and rubella virus, HIV virus and rabies virus. All these viruses cause a variety of symptoms ranging from the common cold, and influenza to the fatal diseases such as AIDS, yellow fever, rabies. In ophthalmology, adeno virus and entero virus commonly cause conjunctivitis. Herpes viruses and HIV are important agents of diseases, causing conjunctivitis, keratitis and retinitis. Viruses can enter the human body by the respiratory tract (inhalation), ingestion and inoculation. Viral multiplication is complex and takes place inside living cells. Viruses are very delicate organisms and can be readily killed by simple measures like washing with soap and water, boiling and common disinfections. Special antiviral drugs are needed to control the infections caused by viruses. Many vaccines are also available to prevent viral infections. e.g., polio vaccine, MMR vaccine, hepatitis vaccine.
Parasites
Parasites are not microorganisms but are organisms, which are much bigger than bacteria and fungi. They can be seen with the naked eye. Parasitic infections are very common in developing countries. These infections are caused mostly by eating or drinking food and water contaminated by people's faeces which contain the ova (eggs) of these parasites. Infection can also be acquired by walking barefoot. Some infections like malaria and filaria are caused by mosquito bites.
Some common parasites are
- Entamoeba histolytica - dysentery (amoebiasis)
- Malarial parasites - Malaria
- Filarial parasites - Filariasis (elephant legs)
- Hook worms - Anaemia
In ophthalmology also they cause a variety of diseases like keratitis (caused by Acanthamoeba).
Treatment of bacteria, fungi, virus and parasite
Some of the commonly used medicines to treat the infection caused by the microorganisms are
- Antibiotic for bacterial infections e.g., ciprofloxacin, ampicillin, gentamycin
- Antifungal treatment for disease caused by fungus e.g., amphotericin B, natamycin
- Antiviral treatment for diseases caused by viruses e.g., acyclovir, gancyclovir
- Antiparasitic agent for treatment of diseases caused by parasite e.g., albendazole
Practical skills
Smear preparation
- Collect the things required: spirit lamp, glass slides, Kimura spatula, and topical drops
- Identify the patient and the case sheet
- Ask the patient to lie down and prepare the eyes for scrapping after explaining to the patient about any discomfort encountered
- Assist the doctor by heating the spatula and instilling a local anesthesia before scraping
- Label the slides with the medical record number of the patient
- Fill in the requisition form with all the required details and send the slides to the laboratory for identification immediately after collection
Gram staining procedure
- Materials from the eye are smeared on a glass slide. They are fixed to the slide by heating.
- A primary stain called Gram's crystal violet is added. After a minute it is washed in water.
- Then, Gram's iodine is added for a minute and washed with water.
- Then the smear is decolourised with a decolouriser, which is a combination of acetone and alcohol.
- This process is immediate and then a counter stain called dilute carbol fuchsin is added for 30 seconds, washed and dried.
- The smear is air- dried; a drop of oil is placed and seen through the microscope. Bacteria with violet colour are Gram positive and those which are red / pink are Gram negative.
Processing in the lab
- The OA receives the sample and checks the requisition form if all details have been duly filled in.
- Enter the details in the register and assign a number to all the samples of a particular patient.
- Incubate the media and prepare the slides for staining.
- In case of preoperative cultures, the OA first cleans the eye to avoid contamination and then collects the sample from conjunctiva and streaks on to a sterile blood agar plate.
- Assigns a number to each patient and enters duly all the details in register.
- Instructs the patient about the need of culture collection and tells them about the consequences of a positive bacterial growth.
Definitions
Sterilisation
Sterilisation is defined as the process by which the surface of an article or medium is freed of all microorganisms either in the vegetative or spore state.
Disinfection
Disinfection means the destruction of all pathogenic organisms or organisms capable of giving rise to infection.
Antisepsis
This is used to indicate the prevention of infection by inhibiting the growth of bacteria. Chemical disinfectants, which are applied to skin and mucous membrane to prevent infection, are called antiseptics.
Principles of aseptic technique are most often used when carrying out a surgical dressing but are equally important in any procedure which is likely to permit the entry of microorganisms into the tissues. i.e. intravenous infusion, catheterization.
Various agents of sterilisation can be classified as physical agents and chemical agents.
Physical agents
- Dry heat: flaming, incineration, and hot air oven.
- Moist heat: pasteurization, boiling, steam under normal pressure, steam under high pressure (autoclave)
- Gas sterilisation
Dry heat
Hot air oven
This method destroys microorganisms by denaturizing of proteins, and increase in the electrolyte contents in the cell. The time period of sterilisation is 1 hour and the temperature attained is 160°-180° c. This method is used to sterilise metal instruments. This is highly effective for ophthalmic instruments. Instrument should be thoroughly cleaned with distilled water and soap before placing in hot air oven.
Practical skill
Method of loading
Allow space between items and the chamber to ensure free circulation of hot air.
Advantage
It is a safe method for glass articles. Dry heat does not blunt the edges of sharp instruments. It is particularly suitable for sterilising eye instruments. Instruments do not become corroded as with repeated autoclaving / boiling.
Moist heat
Boiling
Boiling helps in high-level disinfection. All pathogenic organisms are killed within 10 minutes of boiling at 90-100 degree C. It is not an effective method of destruction of spores, which are highly heat resistant. The instruments should be cleaned properly before immersing in boiling water, as blood, pus, etc. prevents the organism from being killed. Protect the tips of delicate instruments with a rubber tube.
Practical skill
Precaution
Instrument should not be dropped inside the boiler. Place them gently using a Cheatell's forceps. Care should be taken to use only distilled water or clean tap water.
Autoclave
The mechanism is steam under pressure
The principle is that water boils when the vapour pressure of it is equal to its surrounding air. Hence, if pressure inside the vessel increases the temperature at which the water boils also increases. Autoclaving is done at 121 degree C at 15 pounds pressure.
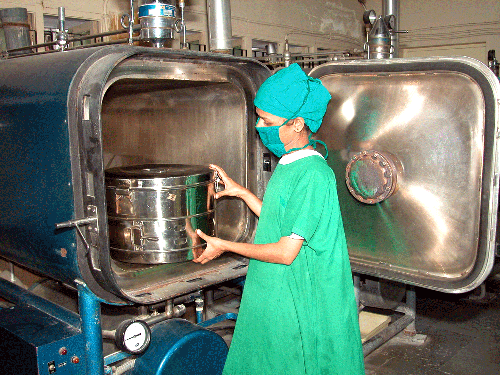
This is a safe method of sterilisation. The steam must penetrate every part and fiber of the item to be sterilised for a specified time at the required temperature. Steam kills organisms by the coagulation of the cell protein. The steam will condense when it meets the cooler surface of the items in the autoclave and the latent heat released on condensation will penetrate and kill the organisms. Materials which may be sterilised by autoclave, include: linen, instruments, rubber, liquids etc. The timing of the autoclave will depend upon the type of materials being autoclaved (Fig.5.2).
Example
- 15 pounds pressure 120 degree centigrade 30 minutes for linen instruments, dressings etc.
- 15 pounds pressure 120 degree centigrade 10 minutes for rubber items i.e., gloves.
- 15 pounds pressure 110 degree centigrade 30 minutes for liquids.
Flash autoclave is a high speed autoclave with a temperature of 180 degree c for 15 minutes. It may be used for cataract instruments in between surgeries.
Practical skill
Autoclaving
Bowie dick test
To check whether the autoclave is functioning correctly a special test run is done which is a shortened cycle. The test is to check the efficiency of air removal from the chamber during the pre-vacuum cycle. About 30 towels are arranged in a pile. Autoclave tape should be placed on the top, middle and bottom towels. The towels are made into a tight pack and the test run performed. The autoclave tape should change colour on all the three towels if it is functioning properly.
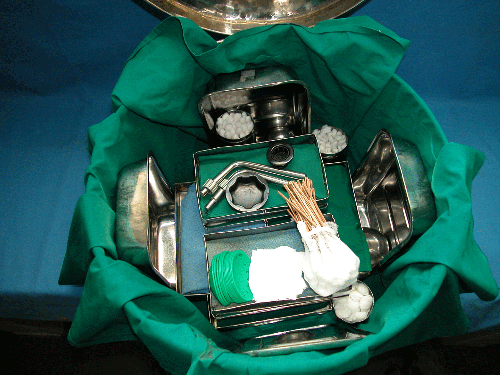
Packing of bins for autoclaving
Instruments should be thoroughly cleaned by washing in warm water. A toothbrush can be used to clean delicate instruments. An ultrasonic cleaner can also be used to clean delicate instrument, it is especially useful for removing the block from cannulaes. Care should be taken when drying the instruments not to damage the tips. Rubber tubing should be used to protect the delicate tips of instruments. Separate each instrument and place them in trays. Place the trays inside the bin after spreading a towel inside (Fig. 5.3). Place one towel with autoclave tape in the bottom, middle and top of the bin. Close the bin and keep the holes open so that the steam can penetrate inside the bin. Linen gowns are folded and packed in such a way that the inside part faces outside to enable surgeons and nurses to put them on without touching the outside. Towels are folded so that the holes of the towel are visible. These items are placed in the bin or in a separate pack with autoclave tape placed as before. Avoid packing items too tightly, to enable penetration of the steam in each and every layer of the items.
Loading an autoclave
Check whether the holes of the bins are open. Do not overload the autoclave, as the steam cannot penetrate easily. Do not load liquids with instruments because the sterilisation time is different. Set the correct pressure and timing. Close the door of the autoclave and switch on.
Unloading
Once the cycle is over, switch off and allow the pressure to come down. Open the door slowly. Close the holes of the bins immediately to prevent microorganisms entering and avoid any contact with unsterile area. Take out the bins, using a clean cloth to prevent burning of your hands. Store the sterile items in their designated place.
Gas sterilisation
Ethylene oxide is effective gas for sterilising instruments and other materials which would otherwise be damaged by heat and chemical disinfectants. For example: vitrectomy probes, cryoprobes, fiber optic light, lens. Sterilisation time is 100 minutes at a temperature of 55 degree centigrade. Complete cycle takes 3 hours.
Practical skill
Preparation for gas sterilisation
Any lubricant should be removed from instruments, as the gas cannot penetrate. All items should be cleaned and dried and any detachable parts taken apart. Make sure items are dried thoroughly before packing as water and ethylene oxide form a harmful gas.
Packing
Double thickness paper (Dennison wrapper) is used for packing. Items can also be packed in a polythene bag. Check that the bag or paper is not damaged before using. Before sealing the items in the bag, make sure there is no air in it to avoid rupture when the vacuum forms in the steriliser.
Loading the steriliser
Items should be loaded in the steriliser carefully to allow free circulation and penetration of gas. Avoid overloading – air space should be provided between the chamber ceiling and the top package. Items should not touch the wall of the steriliser. Then the sterilised articles are kept outside for 24 hours or 8 hours in an aerator. This will remove the irritating quantity of Ethylene oxide.
Chemical agents
Chemical agents cause death of the microorganisms by protein coagulation and breaking of cell membrane.
- Alcohol
- Formaldehyde (Formalin)
- Glutaraldehyde (Cidex)
- Iodine & Chlorine
- Carbolic acid & Lysol
- Ethylene oxide
- Potassium permanganate
- Bleaching powder
Qualities of good antiseptic
- Should kill all microorganisms
- Have speedy action
- Be stable
- Safe and easy to use
- Must not cause irritation
- Must not corrode metals
Chemical sterilisation
This method is used for sharp instruments as boiling can blunt the sharp cutting edges. This should be avoided if heat sterilisation is available.
Dettol, savlon, cidex etc., are the chemicals used for sterilisation of sharp instrument.
1) Glutaraldehyde (CIDEX)
It is used in places where heat sterilization or other methods are unavailable. It kills all microorganisms including spores. The microorganism is destroyed within 3-6 hours of immersion. This method is not recommended because CIDEX is a highly corrosive chemical and inhalation of vapors causes irritation. Further, protective gloves and goggles should be worn while using CIDEX (Fig. 5.4).
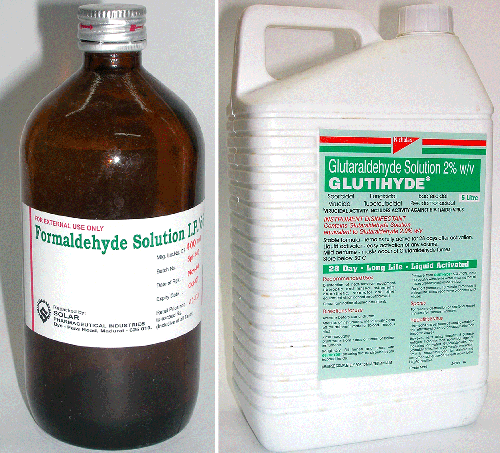
2) Formalin
This is used for fumigation of operation theatres. It destroys all microorganisms. It is available in tablets and liquids. Apart from fumigation it is used for sterilisation for metal instruments and glass. The sterilisation time is 12 to 48 hours and the doors should be sealed and left unopened. The main disadvantage is that formalin is an irritant to eyes and skin and it is carcinogenic. Eye protective equipment should be worn.
3) Alcohol
Ethanol and iso-propanol are commonly used. They destroy microorganisms by protein denaturation, but have no action on spores. 60 - 70% alcohol is generally preferred. It is used for hand washing, disinfection of thermometers, indirect ophthalmoscopy and metal instruments. Iso-propanol is preferred as it is more bactericidal. The time period of sterilisation is 10 minutes, it is an advantage to use alcohol because it is highly inflammable, and evaporates quickly. Methanol is highly effective against fungus but is toxic and flammable.
4) Sodium hypochlorite
It is used for destruction of bacteria, spores and viruses. Sodium hypochlorite is used as a disinfectant in the concentration of 0.4%. The items must be immersed in a container for 10 minutes and washed with sterile water before use. It is used for disinfecting indirect ophthalmoscopy lenses, but the disadvantage is that it is highly volatile and corrosive. It acts as bleach.
5) Povidone Iodine
This is mainly used for surface sterilisation. 10% solution is used for soaking surgical instruments, and facial skin preparation .This is the most popular and easily available disinfectant. It is less expensive and does not have side effects. It is sold as Betadine. A 5% solution is used for hand scrubbing and 0.5% solution is used for eye drops. It destroys bacteria, spores, and fungi. It is used on all metal instruments and for disinfecting sutures. The time period of disinfection is 10 minutes. Povidone Iodine drops are used as an antiseptic before surgery. It is instilled into the conjunctiva to decrease infection. The disadvantage is that it stains dresses, surfaces, and instruments and makes gloves sticky and evaporates if the bottle is not closed tight.
6) Dettol
It is used at 2 to 5% concentration as a hand wash. It destroys microorganism by causing cell lysis. A few drops of dettol mixed with water is used for cleaning rooms.
7) Lysol
This is a mixture of carbolic acid and soap solution. It is active against a wide range of organisms. They are good general disinfectants but are toxic to man. Sharp instruments like needle knife are disinfected for four hours.
Guidelines for OA in relation to asepsis
Outpatients
- Viral conjunctivitis is caused by virus. As patients with conjunctivitis spread the disease, they must not be kept in the waiting room. They must be attended to and sent to the doctor immediately
- After testing infected patients, the nurses must wash their hands well and also the instruments
- Handle sterilised apparatus carefully. Keep sterilised swabs and bandages closed
- Use new disposable syringes
- Keep tonometer clean
Operation theatre
The work of the OA in the operation theatre is very important.
- They must see that patients and assistants follow the rules of the theatre and caution them accordingly.
- They must keep sterilised articles properly labeled and stored away from any contamination.
- They should avoid unnecessary movement and conversation in the operation theatre to keep the risk of infection to a minimum.
- The OA must never be afraid of accepting mistakes or mishap, and must be ready to reveal it to the superiors. This honesty will save the sight of the patient. For example, when a sterilised apparatus falls on the floor by mistake, it must be taken away with the permission of the surgeon. If, on the other hand, it is not reported to the surgeon for fear of reprimand, it will affect the sight of a patient.
- If a OA has a wound, or is suffering from infectious diseases like fever or cold, she must avoid working in the theatre.
The duties of a ward OA
- The OA must supervise whether house- keeping staff cleans the patients' rooms
- Keep the bed sheets clean
- All waste materials must be immediately removed from the ward
- Keep patients with infectious diseases and those who have undergone surgery in separate rooms
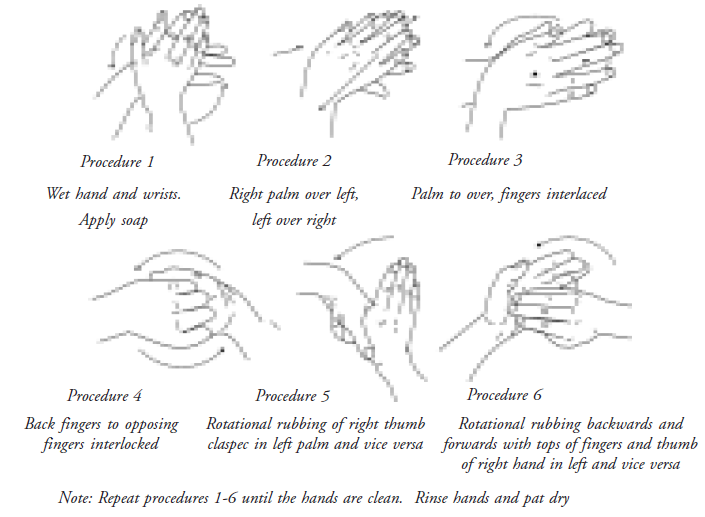
Hand washing
Steps in hand washing
- Wet hands with sufficient water
- Rub the palms together vigorously using soap
- Rub particularly between fingers and finger tips and use nailbrush if possible
- Join hands together so that thumbs and wrists touch each other
- Avoid splashing and wash thoroughly
- Dry on a clean towel, which must be changed daily
Importance / purpose of hand washing
- To prevent cross contamination
- To prevent the spread of microorganisms while having contacts with patients
Materials necessary for hand washing
- Alcohol based hand rub
- Antimicrobial soap
- Antiseptic agents such as chlorhexidene, iodine, chlorine
- Detergents etc.,
Duration of hand washing
- Before handling the patients - two minutes scrub
- In between patient handling - 30 secs
- After handling highly infectious patient-60 seconds
Situation for hand washing
Hands should be washed
- Before any clinical procedure
- Before and after handling infectious patients, food items
- When entering and leaving sterile areas
Skill
- Practical demonstration of hand washing and hand scrubbing
- Communication skill
Attitude
- Awareness of infection
- Vigilance against cross contamination
- Honesty
The most important principles of asepsis are
- Hands must be washed at the beginning of the procedure and at any time during it when an unsterile article is touched.
- OAs with infected skin lesions or throat lesion should not carry out any procedure involving aseptic technique.
- Dressing trolleys should be cleaned in the prescribed manner.
- OAs must always have their hair tied up so that it doesn't fall on the sterile field.
- Soiled dressing must be removed carefully from the wound, to prevent scattering of organisms into the air.
- Used dressings should be put straight into a bag provided for the purpose and later incinerated (burnt).
- Neither the wound nor any part of a sterile item which will come into contact with it should be touched by hand. A strict no touch technique should be adhered to. If any sterile item is contaminated by touching an unsterile area, it should be immediately discarded.
- Unnecessary talking and movement should be avoided.
- Minimum exposure to wounds and minimum disturbances to clothing and linen also minimise infection.
- As most of the infections are caused by droplet spread, one must cough with mouth closed or cover the mouth.
Summary
This unit covers the basic elements of microbiology, sterilisation and essentials of hand washing. Hospital is a place that attracts bacteria, virus and fungi. This section insists on an infection free zone. It is important that they should know the connection of micro organisms and infection control in an eye hospital. The OAs are responsible for providing good sanitation, and preventing the transmission of disease causing micro organisms from patient to patient or from patient to doctors and paramedical personnel. The OA should realise that the infections could happen due to the contaminated, unsterile, disinfected needles and linen if they are not properly disposed of. They should be very careful to wear sterile gloves especially at the time of collecting samples like blood, staining, so that the paramedical personnel / doctor may not get infected through body fluids or contaminated objects. The paramedics and the doctors must be very careful in handling patients with HIV / AIDS and Hepatitis - B patients.
The medical personnel should note that the sterile techniques apply even to opening and closing of eye drops / ointments. Special precautions must be taken by the paramedical personnel in case they have common cold or fever so that they do not infect the patient. To ensure safety of medical personnel and patients, hand washing becomes the base in disinfection procedures.
Key points to remember
- Pneumococci and pseudomonas are common bacteria which cause serious eye infection
- All bacteria can be identified by gram staining procedure and culture. This helps in the treatment of the patients
- Viruses like adeno virus, herpes virus, fungi like aspergillus and parasites also cause many eye infections
- Always use clean water for hand washing
- Dry hands thoroughly to prevent bacterial contamination
- Give importance to finger tips, nails and the space between the fingers
- Do not bring the hands below hip after washing because there may be risk for contamination
- Be careful not to touch anywhere after washing hands
Student exercise
A. Fill in the blanks
- Some common parasites are _________, ________ and ________.
- Diseases caused by S.pneumoniae are________ , _________.
- ___________ and ___________ causes gas gangrene and food poisoning.
- In ophthalmology _________ and _________ commonly cause conjunctivitis.
- Some bacteria require oxygen for growth, these are known as _________.
- The temperature of sterilsation in hot air oven is __________.
- __________ , ___________ can be sterilised by autoclave
- The principle of autoclave is __________.
- ___________ is the most common chemical agent used for sterilisation.
- Hot air oven is used to sterilise_______.
- The test used to check whether autoclave is functioning properly is called ______.
- The only gas-sterilising agent commonly used is _______ .
B. Choose the correct answer
1. SDA culture medium is used to grow
| a. Bacteria | b. Viruses |
| c. Fungi | d. Chlamydia |
2. Of the following, which is not a microorganism?
| a. Hook worm | b. Viruses |
| c. Fungi | d. Bacteria |
3.Common fungal infection in diabetic patient is caused by
| a. Candida albicans | b. Pseudomonas |
| c. Aspergillus | d. Fusarium |
4. Bacteria is _________.
| a. Unicellular | b. Multicellular |
| c. Bicellular |
5.Operation theatre sterilsation with formalin needs:
| a. 24 hrs | b. 48 hrs |
| c. 72 hrs | d. 84 hrs |
6.Which is best to get rid of infection?
| a. Cleaning | b. Drying |
| c. Sterilsation | d. High level disinfection. |
7.The temperature and pressure for sterilising rubber item is _____.
| a. 15 lbs at 120° (30m); | b.15 lbs at 120°(10m) |
| c. 15 lbs at 110° (30min) |
C. Match the following
- Streptococcus - Dysentery
- Ciprofloxacin - Adeno virus
- Entamoeba - Gram-positive bacilli
- Conjunctivitis - Antibiotic
- Antiseptic - Making micro organisms free
- Contamination - Ensuring microorganisms free condition
- Sterilisation - Introduction of microorganisms into sterilsation material
- Asepsis - Kills microorganisms
D. Answer the following
- What are the different types of pathogens?
- What is the procedure for gram stain?
- How do bacteria cause the infection on the human body?
- What are the diseases caused by bacteria, virus, fungus and parasite?
- Name the gram positive and gram-negative bacteria?
- List the various chemical sterilising agents?
- Specify the temperature of each method of sterilisation along with the time period required.
- Which is the best method to get rid of any infection in case of any emergency? Explain in detail?
- What type of disinfectant will be used based on the type of contaminant?
- Write the advantages and disadvantages of each method of sterilisation?
- What are the materials necessary for hand washing?
- What are the purposes of hand washing?
- List the steps of hand washing?
- Define hand asepsis and hand hygiene?
Practical skill
- Discuss different organisms and the diseases caused by them.
- Demonstrate the technique of collecting specimen.
- Carry out the procedures of packing of instruments.
- Carry out the methods of asepsis.
- Individual class demonstration of loading the autoclave.
- Know the exact method of sterilisation for each of the instruments.
- Demonstration of handling the instruments.
- Preparation of the instruments before sterilisation.
