Ocular Emergencies
Ocular Emergencies
Ocular emergencies may be broadly classified as
1. True emergencies, must be attended to within minutes
- Chemical injuries of eye
- Central retinal artery occlusion (CRAO)
2. Other emergent conditions
- CRVO
- Corneal FB
- Corneal abrasion
- Corneal ulcer
- Perforating injuries
- Blunt injuries
1. True emergencies
Chemical injuries
These may be an acid, alkali, or organic solvent.
- Alkali injuries are more dangerous because of easy and deep penetration into the eyes. Common causes of alkali injuries are limewater injury as found in plaster cement or white wash solution, and laboratory accidents (Fig. 13.1).
- Acid injuries may follow laboratory accidents, attempted crimes, battery blast injuries.
- Organic solvents - household items like alcohol, cleaning fluids, gasoline, kerosene

Emergency management in chemical injuries:
- Record visual acuity
- Thorough irrigation of the eye
- Antibiotics
- Cycloplegics
- Steroid eye drops
- Vitamin C tablets
Central retinal artery occlusion
In this condition the blood supply to the retina is cut off leading to the death of retinal cells. This eye condition is similar to cardiac arrest. Hence early treatment helps in regaining vision.
| Symptoms | : Sudden painless loss of vision |
| Signs | : Diffuse pallor of retina, cherry red spot at macula |
- Rule out risk factors like hypertension and diabetes
Emergency management in CRAO
- Ocular massage (has greater effect if done with in 6 hours)
- Paracentesis
- Vasodilator medicines
- Interventions after 12 hours means visual prognosis is very poor
2. Other emergency conditions
Emergencies in cornea
a. Corneal foreign body
Common foreign bodies in cornea are (Fig. 13.2)
- Dust - blown by wind
- Stone, metal and glass - while hammering, chiseling and lathing
- Paddy husk, wood, vegetable foreign bodies in agriculture laborers
Management
- Removal under local anesthesia
- Superficial foreign bodies can be removed with irrigation
- Antibiotics
- Pad and bandage
b. Corneal abrasions
Superficial injuries of the cornea without infections
Management
- Antibiotic ointment
- Cycloplegics
- Pad and bandage
c. Corneal ulcers
Breech in the cornea with infections is called ulcer. Ulcer may be bacterial, fungal, viral, parasitic, or immune related.
Management
- Eye shade
- Specific antimicrobial agents
- Cycloplegics
- Pain killers
d. Gonococcal conjunctivitis
Common in newborn babies. Risk of corneal perforation is greater.
Management
- Penicillin eye drops
e. Perforating injuries of cornea
Here sharp objects lacerate the full thickness of the cornea.
Management
- Immediate pad and bandage
- Surgical repair
Emergencies in glaucoma
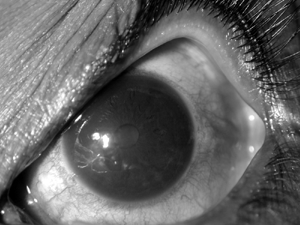
Acute attack of angle closure glaucoma
Obstruction to the flow of aqueous humor following narrowed angle structures results in sudden raise of intraocular pressure resulting in acute angle closure glaucoma.
Signs and symptoms
- Severe pain
- Increased intraocular pressure
- Conjestion of the eye
- Corneal oedema
- Shallow anterior chamber
- Pupillary sphinter atrophy
- Glaucomatous optic nerve head cupping
- Nausea and vomiting
Management
- Pilocarpine eye drops
- Timolol eye drops
- Pain relievers
- Oral diamox tablets
- Interavenous mannitol (if needed)
- Laser peripheral iridotomy
- Check BP before starting mannitol as it may cause hypotension
- Ask for history of asthma before giving Timolol drops. It should be avoided in asthma patients.
Absolute glaucoma with pain
End stage glaucoma with high intra ocular pressure produces pain due to stretching of the layers of eye ball.
Management
- Measures to reduce pain
- Measures to reduce introcular pressure
Lens induced glaucoma
a. phacomorphic glaucoma: increase in size of the cataract lens obstructs the flow of aqueous humor and increases intraocular pressure.
Management
- Measures to reduce intra ocular pressure
- Cataract extraction with intraocular lens implantation
b. Photolytic glaucoma: rupture releases lens materials at the angle of anterior chamber, increasing the intraocular pressure.
Management
- Topical steroids
- Measures to reduce intra ocular pressure
- Cataract extraction with intraocular lens implantation
Pupillary block glaucoma
Blockage at the pupil causes reduced flow of aqueous humor from the posterior chamber to the anterior chamber resulting in increase in intraocular pressure. Pupillary block may follow obstruction by lens, IOL, vitreous, organized inflammatory exudates, etc.
Management
- Measures to reduce intra ocular pressure
- Mydriatics
- Laser iridotomy
- Surgical intervention if necessary
Emergencies in cataracts and post cataract surgeries
1) Traumatic cataracts: they are lens opacification following penetrating or blunt injuries of the eye with or without rupture of the lens capsule.
Management
- Evaluation of the amount of cataract by slit lamp examination
- Evaluation of other associated ocular injuries
- Posterior segment evaluations by indirect ophthalmoscopy or by ultrasound scan
- Plan for cataract extraction with or without intra ocular lens implantation
2) Post operative wound leaks: it is clinically evident by weak surgical wound, shallow anterior chamber, leak of aqueous humor, with or without reduced digital tension
Management
- Immediate pad and bandage
- Surgical intervention if necessary
3) Post operative iris prolapse: usually follows weak surgical wound
Management
- Immediate pad and bandage
- Repeat surgical intervention
4) Post operative endophthalmitis: it is a dreadful condition following introcular surgeries characterized by infection of internal ocular tissues.
Signs and symptoms
- Sudden visual loss
- Pain
- Exudates in anterior chamber
- Exudates in the pupillary area
- Loss of fundal red reflex
- Ultrasound Bscan helps in diagnosis
Management
- Intensive antimicrobial treatment following culture and sensitivity
- Painkillers
- Intravitreal antimicrobial agents
- Vitrectomy
Emergencies in Orbit
Orbital cellulitis: inflammation of orbital tissues is called orbital cellulitis. It causes intense pain and swelling. Risk of extension into the brain is common especially in diabetics and immune compromised patients.
Management
- Oral and parental antibiotics
- Pain killers
- Cautious usage of steroids if necessary
- Imaging techniques like CT scan in non responding cases
- Orbital trauma (fracture of orbital walls)
Management
- Pain killers
- X-rays
- CT scan
- Surgical intervention if necessary
- Abscess in and around orbits: an abscess is a localised collection of pus. Abscess around the orbit usually lid abscess or lacrimal abscess
Management
- Pain killers
- Antibiotics
- Incision and drainage
- Daily cleaning and dressing
- Pan ophthalmitis: inflammation of all layers of eyeball following infection.
Management
- Pain killers
- Antibiotics
- Eviseration
Emergencies in Neuro Ophthalmology
Optic neuritis: inflammation of the optic nerve is called optic neuritis. Inflammation of the optic nerve head is called papillitis and inflammation of retro orbital portion of the optic nerve is called retrobulbar neuritis.
Signs and symptoms
- Sudden loss of vision
- Pain with extra ocular movements
- Pupil abnormalities: relative afferent pupillary defect (Sluggish pupillary reflex compared the normal eye due to an optic nerve defect)
- On swinging torchlight from normal to abnormal eye, the pupil will dilate instead of constricting
Management
- Oral and parental steroids
- Traumatic optic neuropathy: usually follows road traffic accidents in young males
Signs and symptoms
- Sudden loss of vision following injury to the eye brow
- RAPD
Management
- Oral and parentral steroids
- Cerebro vascular accidents: results in bleeding into the brain which may cause visual loss. Usually occurs in old age, diabetes and hypertension. Vital signs should be monitored. Air way maintenance, BP, pulse monitoring.
Management
- CT brain
- Neurologist referral
Head injury
Management
- CT brain
- Neurologist referral
Papilloedema:
Non inflammatory oedema of the optic nerve head secondary to increase in intra cranial pressure. Also seen in conditions of malignant hypertension and pseudo tumor cerebri.
Signs and symptoms
- Headache
- Transient obscuration of vision
- Visual acuity and colour vision usually normal
- Visual fields show enlarged blind spot
Management
- Record blood pressure
- CT Scan brain
- Neurologist opinion
Emergencies in retina
- CRAO (described earlier)
- Retinal tears: breaks in the peripheral retina
Signs and symptoms
- Flashes of light
- Floaters - inform the ophthalmologist immediately
- Indirect ophthalmoscopy reveals the breaks
Management
- Laser barrage
- Periodic follow up
Retinal detachment
separation of neuro sensory retina from the retinal pigment epithelium. It is common in high myopia.
Signs and symptoms
- Sudden or progressive loss of vision
- Field defects
- H/O seeing floaters and flashes of light.
- Management : surgical repair.
Practical exercises
1. Irrigation of the eye
It is necessary to irrigate the eye when some chemical substance falls on it.
Equipments needed
- A bottle of sterilized normal saline
- Kidney tray
- Local anaesthtic (4% xylocaine eye drops)
- A towel to protect the patient's face
- Sterile cap to protect ears
- Sterilized swabs
- Receiver tray
Procedure
- Explain the procedure to the patient and ask them to lie down
- Put a towel around the patient's shoulder and a cap over the patient's head covering the ears
- Wash and dry your hands
- Apply local anaesthetic drops
- The kidney tray is held firmly, against the patient's face.
- Separate the lashes with fingers. Instead of irrigating the eye first, practice on the cheek
- Saline should be poured continuously and uniformly. Ask the patient to look up and down and sideways. In order to expose the conjunctiva fully wash all parts of the conjunctival sac. Straighten the upper eyelid. Use the entire amount of liquid given to irrigate.
- After irrigating the eye, dry the eyelashes with the sterilized swab. Remove the tray and see that the patient is comfortable.
- Record the procedure and remove the udrf materials.
Note
- Repeated syringing with isotonic saline in to the conjunctival sac can be done.
- For alkali injuries irrigation for at least 30 minutes and for acid injuries at least for 20 minutes is recommended.
- Time factor is important; the time between the fall of the chemical agent and irrigation determines prognosis of vision.
2. Vitals monitoring
In conditions of cerebro vascular accidents, head injuries and papilloedema following the space occupying lesions of brain, essential monitoring of blood pressure, pulse, temperature and respiration is mandatory.Notification and urgent call of the doctor in case of deterioration has to be done. (usually there will be decline in BP and decline in pulse rate.)
3. Ocular massaging
It is helpful in conditions of central retinal artery occlusion when patients presents earlier than 48 hours of manifestations.
Procedure of giving ocular massage
- Can be given digitally or with a three mirror gonioscope
- Over the closed leds use fingers to give moderate pressure over the globe intermittently
- Initially give pressure for 10 seconds then release pressure for 5 seconds
- Continue alternate pressure and release of pressure for a maximum period of 20 minutes
- Meantime an ophthalmologist should be called and other modes of reestablishing retinal blood flow should be initiated
Key points to remember
Do 's
- Take the patient's medical history in detail
- Check visual acuity to establish a baseline measure
- Ask questions to help to identify the nature of a foreign body if one is suspected and gather details of the accident
- In case of chemical burn, collect the data regarding the name or type of chemical involved, the extent of exposure to the chemical
- Notify the ophthalmologist or other staff immediately.
Don't 's
- Unnecessarily touch or handle an eye that has a laceration or rupture
- Apply pressure to the globe while attempting to open the lids
- Administer drops or other medications without authorization from the physician and instruction on the proper methods.
- Use previously opened bottle of eye drops for a patient who may have a penetrating eye injury (always use a new unopened, sterile bottle)
- Touch the dropper of the container
Student exercise
Fill in the blanks
- True emergencies are ______ and ______.
- Ocular massage in CRAO is effective within _________ of onset.
- Lens induced glaucomas are _______ and ____________.
- Retinal detachment is a separation of ________ layer from _______ layer.
- Seeing flashes of light and floaters are suggestive of ________ following trauma .
Choose the most appropriate answer
1. Which of the following is not a treatment of chemical injury to eye?
| 1. Irrigation | 2. Antibiotics |
| 3. Cyclopedias | 4. Ocular massage |
2. Following are the symptoms of an acute attack of angle closure glaucoma except
| 1. Severe pain | 2. Congestion of blood vessels |
| 3. Corneal edema | 4. Floaters and flashes of light |
3. Phacolytic glaucoma is due to
| 1. Blockage at pupil | 2. Increase in size of cataractuous lenses |
| 3. Rupture of cataractuous lenes | 4. Shape of the layers of eyeball |
4. Ocular massaging is useful in
| 1. Chemical injuries | 2. Phacolytic glaucoma |
| 3. Endophthalmitis | 4. CRAO |
5. Irrigation of eye is the treatment of
| 1. Chemical injuries | 2. Phacolytic glaucoma |
| 3. Endophthalmitis | 4. CRAO |
Exercise
- What is the first step in management of a patient with chemical injuries of the eye?
- Name two of the most common ocular emergencies and how to handle them
- What are the do's and don'ts to remember in case of ocular emergencies?
- Distinguish between emergencies and non- emergency conditions of the eye.
- Review the emergency procedure guidelines with your senior staff member.
- Write an assignment about the different ocular emergencies, various drugs and procedures used to handle them.
- Set up a time to role play patient screening and emergency exercises with experienced members of the office staff
- Demonstrate the procedure of irrigation
