Professional Etiquette
Dress code
The OA is a member of a health care team. Primary nursing care is a method of patient care delivery in which the OA is responsible and accountable for the entire nursing care of the patient. The OA is to be easily identified by the patients and their attenders. Hence they are to be in uniform. Usually they wear white sari and white blouse in some of the regions in India. The hospital management can choose the colour and pattern of the uniforms. Whatever the colour and pattern, they should dress neatly and properly.
The Purposes of introducing a uniform for the OA are
- To promote a professional impression on customers and the public
- To promote employee, patient, customer safety and comfort
- To frame the professional image required for medical professionals
- To identify people by their dress
Policies
The following standards of dress and grooming are required for all categories of clinical staff providing direct patient care in clinical settings including students and physicians.
- Uniform should be clean and dressed up neatly
- Jewelry worn should be appropriate for the clinical area and present no threat of injury to the employee or patient
- Hair should be neat and tied up
- No flower is to be worn
- No finger ring is to be worn
- Nails should be cut short, clean and no polish is allowed
- Name badge should be worn
- Uniform slippers should be worn
- Always wear a wristwatch with a second hand
- Nothing should be worn related to religion e.g.. Bindi
This dress code should be maintained by all employees
Personal hygiene
Personal hygiene is to be performed as often as necessary to stay clean and comfortable. People who can take care of themselves practice hygiene out of habit. Other hygiene measures may be done regularly before and after meals and at bed time. Infants, children and adults who are disabled may need help with hygiene. Remember to assist a patient with personal hygiene whenever necessary. Personal hygiene is the first step to good grooming and good health. Elementary cleanliness is common knowledge. One of the most effective ways we have to protect ourselves and others from illness is good personal hygiene. In a hospital setup personal hygiene is very important. It includes
- Oral hygiene
- Bathing
- Well combed hair
- Clean face
- Washed dress
- Well clipped nails
- Clean stockings
Oral hygiene
Oral hygiene prevents illness and promotes a healthy mouth. A clean mouth and clean teeth prevent mouth odours and infections, increases comfort and make food taste better. Illness and disease may cause a bad taste in the mouth. Brush teeth regularly.
Bathing
To prevent offensive body odour, it is important to take bath regularly.
Well combed hair
Hair should be clean and styled in an attractive and simple way.
Washed dress
Uniform should fit well and be modest in length and style. Wear a clean and well pressed uniform daily.
Well clipped nails prevent microorganisms from growing and multiplying. Proper care prevents odour and infections. Feet should be washed daily and dried thoroughly between the toes.
Special hygiene measures are necessary during menstrual periods. Hand washing is necessary to prevent infections. Good health and personal hygiene practices will help you to feel well.
Qualities of health care professional
In a health care profession program, we expect our students to further develop the capacity for compassion and the understanding of professional integrity by testing themselves in real life experiences.
The important qualities of a health care professional are:
- The ability to communicate effectively
- An underlying compassion about others
- Unyielding integrity
- Unbending patient advocacy, pleading in support of an issue. Aim of advocacy is to generate public demand.
- Critical thinking skills
- Taking care about listening to the patient, having a sense of humor.
Communication skills
Many learning activities that utilize communication skills, both oral and written, will be provided. Frequent feedback will be provided on communication skills throughout the learning experiences using formal and informal methods.
- Compassion for others through communication skills can be enhanced by role playing patient feedback as well as by mentoring (faculty and staff supervision of student). Important to this learning objective is the foundational knowledge of diversity, and multicultural environments in which the health professional works. Students will have lot of experiences to enhance understanding as well as skill development in translating compassionate care across cultural boundaries.
- Patient advocacy : An effective health care professional needs the knowledge and the competence to handle the complex environment of health care. Starting with ethical reasoning they should be provided with opportunities to learn about the legal, regulatory, and practice management of the profession. Whether the patient presents with chronic diseases, issues of abuse or neglect, or mental health problems, the health care professional has the knowledge and position to support patient needs. Students will have learning opportunities in several settings to increase their understanding and competence in dealing with the health care environment. This ability to interface between the patient and the health care networks will enhance patient advocacy.
- Critical thinking skills: Critical thinking is necessary for a health care professional because they have made a commitment to take responsibility for the life and welfare of others outside their family and friends. Health care professional plays an important role in educating patients and facilitating informed patient consent as well as by gathering data for diagnosis, testing outcomes, treatment, and understanding safe limits of practice.
Medical ethics in hospitals
Medical ethics is the study of moral questions pertaining to the practice of medicine and health care. Physicians' medical ethics have long been governed by the Hippocratic oath, in which physicians declare that they will do everything possible to preserve human life and to maintain high working standards. Licensing boards and national and international associations hold physicians accountable for their decisions in the practice of medicine.
Medical ethics, a branch of ethics, deals with moral validity of decisions in various aspects of medicine. The Hippocratic oath is the most enduring tradition in medicine that has been the guiding ethical code for physicians since ancient Greece, and has eventually become the basis of all medical ethics. In its most compelling portions, it emphasizes the profundity of the medical agreement, the patient dignity, the confidentiality of the transaction and the Physicians' responsibility to guard against abuse or corruption of his or her knowledge and art. It also exhorts the physicians to honour the rules of their profession and expose those who do not follow high standards of conduct.
Ethics address conduct and relate to what behavior is appropriate or inappropriate, as reasonably determined by the entity setting the ethical standards. An issue of ethics in ophthalmology is resolved by the determination that the best interests of patients are served.
Ophthalmologic services must be provided with compassion, respect for human dignity, honesty and integrity. An ophthalmologist must maintain competence. Competence can never be totally comprehensive, and therefore must be supplemented by other colleagues when indicated. Competence involves technical ability, cognitive knowledge, and ethical concerns for the patient. Competence includes having adequate and proper knowledge to make a professionally appropriate and acceptable decision regarding the patient's management.
Rules of ethics
Ethics are difficult to define precisely but important in any professional practice. In general these are the moral and professional values which govern the acts of practice and actions of its practitioners. Almost all professions are bound by a broad set of guidelines which collectively constitute professional ethics. The Rules of Ethics are enforceable.
1. Competence
An ophthalmologist is a physician who is educated and trained to provide medical and surgical care of the eyes and related structures. An ophthalmologist should perform only those procedures in which the ophthalmologist is competent by virtue of specific training or experience or is assisted by one who is. An ophthalmologist must not misrepresent credentials, training, experience, ability or results.
2. Informed consent
The performance of medical or surgical procedures shall be preceded by appropriate informed consent. Patients are to sign the consent letters.
3. Clinical trials and investigative procedures
Clinical trials or investigative procedures shall be approved by adequate review mechanisms. Clinical trials and investigative procedures are those conducted to develop adequate information which would form a base for prognostic or therapeutic decisions or to determine etiology or pathogenesis, in circumstances in which insufficient information exists. Appropriate informed consent for these procedures must recognize their special nature and ramifications.
4. Other opinions
The patient's request for additional opinion(s) shall be respected. Consultation(s) shall be obtained if required by the patient.
5. The impaired ophthalmologist
A physically, mentally or emotionally impaired ophthalmologist should withdraw from those aspects of practice affected by the impairment. If an impaired ophthalmologist fails to do so, it is the duty of other ophthalmologists who know of the impairment to take action with a view to correct the situation. This may involve a wide range of remedial actions.
6. Pretreatment assessment
Treatment shall be recommended only after a careful consideration of the patient's physical, social, emotional and occupational needs. The ophthalmologist must evaluate the patient and assure that the evaluation accurately corresponds to the ophthalmic findings and the indications for treatment. Recommendation of unnecessary treatment or withholding of necessary treatment is unethical.
7. Delegation of services
Delegation is the use of auxiliary health care personnel to provide eye care services for which the ophthalmologist is responsible. An ophthalmologist must not delegate to an auxiliary those aspects of eye care within the unique competence of the ophthalmologist (that is other than those permitted by law to be performed by auxiliaries). When other aspects of eye care for which the ophthalmologist is responsible are delegated to an auxiliary, the auxiliary must be qualified and adequately supervised. An ophthalmologist may make different arrangements for the delegation of eye care in special circumstances, so long as the patient's welfare and rights are the primary considerations.
8. Postoperative care
The providing of postoperative eye care until the patient has recovered is integral to patient management. The operating ophthalmologist should provide those aspects of postoperative eye care within the unique competence of the ophthalmologist. Otherwise, the operating ophthalmologist must make arrangements before surgery for referral of the patient to another ophthalmologist, with the patient's approval and that of the other ophthalmologist. The operating ophthalmologist may make different arrangements for the provision of those aspects of postoperative eye care within the unique competence of the ophthalmologist in special circumstances, such as emergencies or when no ophthalmologist is available, so long as the patient's welfare and rights are the primary considerations. Fees should reflect postoperative eye care arrangements with advance disclosure to the patient.
9. Service with honesty
An ophthalmologist must not misrepresent the service that is performed or the charges made for that service.
10. Procedures and materials
Ophthalmologists should order only those laboratory procedures, optical devices or pharmacological agents that are in the best interest of the patient. Ordering unnecessary procedures or materials or withholding necessary procedures or materials is unethical.
11. Commercial relationships
An ophthalmologist's clinical judgment and practice must not be influenced by economic interest in, commitment to, or benefit from professionally-related commercial enterprises.
12. Communications to colleagues
Communications to colleagues must be accurate and truthful.
13. Communications to the public
Communications to the public must be accurate. They must not convey false, untrue, deceptive, or misleading information through statements, testimonials, photographs, graphics or other means. They must not omit material information without which the communications would be deceptive. Communications must not appeal to an individual's anxiety in an excessive or unfair way; and they must not create unjustified expectations of results. Communications must not misrepresent an ophthalmologist's credentials, training, experience or ability, and must not contain material claims of superiority that cannot be substantiated.
14. Interrelations between ophthalmologists
Interrelations between ophthalmologists must be conducted in a manner that advances the best interests of the patient, including the sharing of relevant information.
15. Conflict of Interest
A conflict of interest exists when professional judgment concerning the well-being of the patient has a reasonable chance of being influenced by other interests of the provider. Disclosure of a conflict of interest is required in communications to patients, the public, and colleagues.
16. Expert testimony
Expert testimony should be provided in an objective manner using medical knowledge to form expert medical opinions. Non-medical factors (such as solicitation of business from attorneys, competition with other physicians, and personal bias unrelated to professional expertise) should not bias testimony. It is unethical for a physician to accept compensation that is contingent upon the outcome of litigation. False, deceptive or misleading expert testimony is unethical.
Nature of negligence in doctor - patient relationship
Negligence in the legal sense is not only applicable to the medical practitioners but it also concerns the harm that any person may have sustained at the hands of the medical practitioner. Taking a cue from this concept it can be said that a successful action against negligence therefore requires 3 elements, and they are:-
- There should be duty of being careful. In medical parlance, it means that the doctor understands that his patient would be affected by his wrong treatment.
- The second part is breach of the above stated duty. Generally, that would imply the doctor managed the case in accordance with the accepted standards of practice at that point of time.
- The third element required to be proved is finding out whether the doctor was negligent. This is a very difficult task to establish that the act of the doctor was directly and proximately related to the harm done to the patient. Most of the time when the patient approaches the doctor he is already sick. Therefore the facts that the patient has become more sick after taking the treatment from the doctor, or the illness remained the same, and he did not get any relief, etc. become very important.
Eye camps and ophthalmic surgeons
The recommendations referred to by the said committee of the Indian Medical Council are as follows:
- The operations in the camp should only be performed by qualified and experienced ophthalmic surgeons registered with the Indian Medical Council or any state medical council.
- The camps should not be used as training ground for post graduate students and operative work should not be entrusted to them.
- There should be a trained lab technician to examine urine, blood sugar etc. It is preferable to have a dentist to check teeth for sepsis and physician for general medical check up.
- All the medicines to be used should be of standard quality duly verified by the doctor in charge of the camp.
- Eye camps have to be organised, due care and caution has to be exercised by the organisers as per the procedure established by law.
- The poor and rural people cannot be ignored. They should be treated with dignity. They also have a right to life and a right to good medical care.
- Open communication with the patient is essential. Patient's confidentiality must be safeguarded within the constraints of the law.
The OA and the law
Carelessness or negligence on the part of an OA may lead to court action against the OA or the hospital, and damages could be awarded against the OA or the hospital authority. Some examples where the OA has to abide by the law are given below:-
1. Consent for operation
A patient coming into the hospital still retains his rights as a citizen and his entry only denotes his willingness to undergo any investigation or treatment of serious nature or an operation that requires anaesthesia. For the operation the written consent of the patient is a must. A patient may give his own consent if he has attained the age of 18 and is in sound state of mind. For the minor patient the signature of the parents or guardian is normally obtained. In the event of any difficulty, the OA must inform the surgeon and the senior administrative officer.
2. Correct Identity
The OA has a serious responsibility to make sure that all the patients in general ward are given bed numbers and register numbers. It is very important that the correct number is written in all the records and no mistake is made. They are checked again and again. In Operation Theatre, the “scrubbed” OA must check the number of instruments, needles, sponges, packs on the trolley frequently during operations and as operation proceeds, check each item used. They are all counted and the count of each item returned is correct.
3. Medications and drugs
There are two Acts which control the use of drugs in treatment.
1) Poisonous drug Act
2) Food and drug Act
A prescription must bear:
- The patient's name and address
- The date
- Signature of the prescriber
- Total quantity to be supplied in word or figures
4. Accidents or injury
Accidents can arise to visitors or employees of the hospital through negligence. Hospital staff should constantly be alert to the risks entailed and bring them to the notice of person concerned or the proper authority. In case of a pure accident where no negligence or incompetence is involved there is no liability at law.
5. Discharge of the patient against medical advice
Sometimes patient demands a discharge from hospital of their own will. It is the OA's duty to persuade them not to do so. But if the patient insists, the OA should inform the doctor concerned.
6. Patient 's property
The department of health and social security requires all hospitals to inform the patient that the hospital cannot take responsibility for valuables or money. Where it is known that patients have an excess of money or ornaments they should be asked to hand it over against a signed receipt and it may be placed in the hospital locker.
7. Signing of legal document
Most hospitals have a rule against the OA signing the legal documents or witnessing signature during their professional duties.
8. Suspicion of theft
The OA must immediately report any theft or suspicion of theft to senior administrative officer who should look into the matter without delay.
9. Professional secrecy
The OA should not disclose any confidential information obtained because of their position regarding the patient to anyone, even to the closest relatives of the patients or friends. The details of the patient's disease should not be passed on to their employer as this may cause loss to the patient such as removal from service for which the OA may be held legally liable.
Legal responsibility of OA means the way in which they are obligated to obey the law in professional activities. The law is the final authority for regulating activities of all citizens including professional practitioners. Disobedience of the law results in punishment.
Procedures in nursing demanding special care and attention
- To have written orders from the doctor for treatment and care of the patient.
- To administer medicines-giving only as ordered, checking labels and appearance of medicines, charting accurately.
- To administer cold or hot applications to the body especially for patients unable to respond.
- To get permission slips signed for surgery or other treatment.
- To report accidents or errors.
Causes of ethical decline
In any country many factors are responsible for the deterioration of morality in the medical practice.
- A large initial investment is required to set up a clinic, a hospital or a medical institute; and it is thought appropriate to charge heavy fees to the patients as a means of recovering the cost.
- There is an increased awareness in the patient community about their legal rights. Thus doctors have fear of getting charged by consumer and other courts for criminal negligence in treating the patients. Money required to plead the cases may be substantial and hence the hospital charges are high.
- The patient approaches a doctor with mixed feelings of faith and fear, of hope and hostility. This inevitably leads to distorted doctor-patient relationship with high chances of exploitation.
- Many doctors do not (or cannot) offer the best line of treatment to the patients, some are ill trained, They are not fully aware of recent advances in the treatment and management of the disease. Additionally, poor clinical sense and lure of income from costly investigations lead the doctor to ask for unnecessary pathological and radiological tests.
- Many doctors do not have standard treatment facilities in their own clinics or hospitals. Instead of referring the patients to an institute where such facilities are available, the treating physician dose not inform about such facilities for fear of 'losing the patient's.
The basis of ethics, according to Swami Vivekananda is to become more and more selfless: ";Whether men understand it or not, they are impelled by that power behind to become unselfish. That is the foundation of morality. It is the quintessence of all ethics, preached in any language, or any religion, or by any prophet in the world. "; Be thou unselfish";, ";Not ";I";, but 'thou'";- that is the background of ethical codes.";
Patient communication
There is great development in the medical field. The discovery of new equipment and treatments are many. Only effective communication can differentiate the services rendered by the hospitals.
Ineffective patient communication is one of the indicators that creates a bad impression about a hospital. If it is not taken seriously, it may lead to closure of the unit. Good patient communication is itself one of the economic and marketing strategies on which the organisation may rely continuously for its increased market share and growth.
Various tools and methods should be taken into consideration for effective patient communication:
Meaning of "communication":
This word is derived from the Latin word ";communis"; which means ";common";.
In words of Allen ";Communication is the sum of all things one person does when he wants to create understanding in the mind of another. It is a bridge of meaning. It involves a systematic and continuous process of telling, listening and understanding.";
Meaning of "patient communication":
It is a process through which a hospital provides its patients the required information on the types of services, specialists and facilities available through various tools and techniques.
Methods for patient communication
Telephonic communication
This plays an important role as a proper communication tool. Through this the good image of the organisation can be protected. Receptionist / Operator or whoever attends the calls should respond in a polite manner, give clear and concise information to the person on the other side for their queries or doubts and for fixing appointments with consultants.
If the need arises the operator should involve the doctors in clarifying the doubts of the patients instead of giving wrong information about the medicine or treatment .
Doctor - patient communication
The clinician communication towards the patient is very important.
Ineffective communication between doctors and patients often reduces the accuracy of a clinician's diagnosis though time constraint is usually the main reason.
Nevertheless, numerous studies indicate that doctor-patient communication is the single most effective predictor of patient adherence to treatment plan. Hence the effective doctor-patient communication is a necessity and should not be an option.
According to the Bayer Institute for Health Care Communication, a doctor's role in communicating effectively with patients can be broken down into the following tasks:
- Engagement
- Empathy
- Education
- Enlistment
Engagement
It is a connection between the doctor and patient that continues throughout the encounter and sets the stage for partnership.
For successful engagement the doctor should show interest in the patient as a person, should use the patient's language rather than medical jargon.
Empathy
This is being sincere towards a patient by having direct eye contact and listening to the patient's information. This makes the patient feel that they are acknowledged by the doctor.
Education
It is providing increased knowledge and under standing to the patients about the disease for which they come and at the same time decrease their fears.
Enlistment
It is inviting the patient by the doctors to collaborate in decision-making regarding the problem and the treatment plan.
Counselling
Meaning
- It is a helping process
- To raise awareness about the diseases
- To facilitate patient in informed decision-making about the treatment plan
- To increase compliance to treatment that includes follow-up treatment
- To moderate patient's expectation
- To rise with increased new services
The counsellor interacts with the patients and first tries to understand their actual problems. Then according to the type of service to be provided to them, they explain about that service in detail. For example, for cataract surgery the counselor explains the meaning of cataract, its impact on the eye, the necessity for surgery, the surgery cost, the facilities that would be available during surgery period, etc.
Thus, counseling is one of the tools for effective patient communication as it is an art to understand people's feelings and convince them to go about the required treatment plan.
The required counselling skills are
- Listening
- Giving information
- Making suggestions
- Challenging
- Supporting
Notice boards
This informs the patients of the policies, procedures, rules, events of a hospital. This is helpful for those patients who are literate.
Sign boards
This shows the route to the patients for the particular unit/department they want to go.
The signs should be clear, bold and dark enough to be easily seen by the elderly patients also.
Information boards
The information boards give basic information on various diseases like refractive error, glaucoma, cornea ulcer, cataract etc., its prevalence and incidence rates within the state and in our country, its impact over the body and curative and preventive measures to be taken by the patients.
Information machine
Touch Screen is a machine that gives the history and founder of the organisation, the organisation's culture and its values, its layout, the type of services available, the facilities, the specialists available, the charges for the various treatments, the symptoms, cause, curative and preventive measures of some diseases, the details of the courses being conducted by the hospital.
Leaflets / brochures
It gives a gist of the purpose, achievements in various fields, discoveries / research studies in different clinical subjects, the various health programmes and type of services being provided by the hospital.
Annual reports
This gives the details of any new health program or new clinical departments started, the number of surgeries performed through various camps, the training programme conducted to staff of different clinics, the welfare activities for its staff and any other social welfare activities being conducted by the hospital in that particular year.
Press releases
It includes the new activities started, any achievements through different surgeries etc. It helps not only in publicizing the activities but also in mobilizing the like minded persons for their activities in the form of volunteers, the sponsors, the consultants from both the government and NGO's.
Advertisements
This is giving ads in local newspapers, in both government and private television channels, etc. Through hoardings, illumination boards about the type of services and the facilities of a hospital, the public can be informed about the hospital activities.
Patient communication is a vital process in any hospital. It should develop and maintain a proper system for long-run purpose. This can be understood from the sayings by Mahatma Gandhiji.
"; A Customer is the most important visitor on our premises.
He is not dependent on us; we are dependent on him.
We are not doing him a favor by serving him; he is doing a favor by giving us an opportunity to do so";.
Internal communication
The prime responsibility of the administrator of any hospital is to get things done through people. Proper communication through proper channel should be carried on. The method of communi- cation differs from one person to another. To avoid misunderstandings, conflicts, disagreement between persons of various departments of an organisation, communication is essential.
A proper communication system of a hospital reflects its strength in achieving both the short term and long term goals of a hospital.
Though communication plays a very important role in all areas of the hospital, its importance facilitates the proper care of a patient through OA services. A lack of communication between the OA and the doctors, between the OAs themselves can lead to the death of a patient.
Hence communication is a vital management tool, a proper and careful handling of which benefits the individual and an organisation in achieving the mission of a hospital.
The types, process, methods and barriers of communication within an organisation:
Need for communication
- To coordinate the activities across various departments in a hospital
- To help in decision making process
- To maintain good relationship among people.
Process of communication
The main elements of communication process are:Communicator
The process begins here. The communicator is one who sends the message to the receiver. In hospital the communicators may be the top managerial persons, the administrator, the department heads.
Message
It is the information which a communicator sends to the receiver.
Medium
It is the link that connects the communicator and the receiver. Example: telephones, computers etc.
Receiver
It is the person who receives the message from the sender.
Feedback
It is a process of informing the sender by the receiver the understanding of the message sent to them.
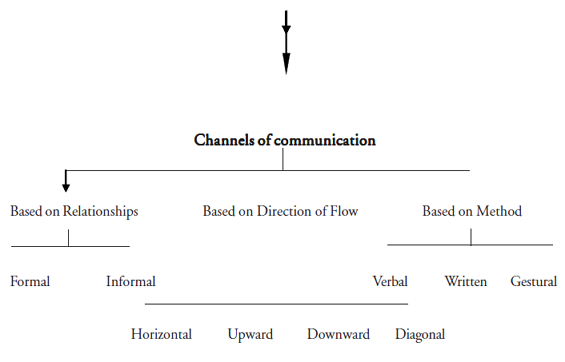
Channels of communication
Formal communication
It is established formally by the management. It is used for communicating the official messages within or outside hospital.
Informal communication
This is also "; Grapevine "; communication. It takes place during informal or social relations among people of various departments in a hospital. It spreads rapidly in the form of rumors and gossips.
Horizontal communication
This is transmission of information among the positions of the same level. Example-communication between the managers of different departments.
Upward communication
This is flow of information from lower-level employees to higher-level employees. Example: suggestions from staff to management.
Downward communication
This is flow of information from higher level to lower level employees.
Example: circulars, orders from medical director to OA.
Diagonal communication
Flow of messages between persons who are in positions at different levels of the hierarchy and in different departments.
Example: communication between computer technician and the storekeeper in a hospital.
Verbal communication
It is communicating the messages orally. It is easy to communicate and economic but it is dangerous as it does not have any document proof of communication.
Example: informing (over phone by the administrator) about the staff-management meeting to the staff at various levels.
Written communication
It is communication in written form. It is the best way of communication as it contains the written document as proof for future verifications.
Example: work instructions, circulars, memos etc.
Gestural communication
It is communicating through gestures. Example: nodding the head by the staff to indicate that the message told by their department in-charge has been understood.
Barriers of communication
Language
It is very important in communication. The words used by the communicator should be apt and simple to understand by the receiver.
Filtering
As the message travels through many levels of hierarchy in an organisation, it gets distorted when it actually reaches the final person.
Poor listening
This is due to poor concentration in listening by the message receiver.
Over loading of information
This is providing more information than the capacity of the listener.
Status
This exists between manager-employee pairs. The manager should not deal with the employees with ego.
Guidelines for an effective communication
1. Appearance - It should be simple and smart
2. Posture - Should not show any signs that may indicate insincerity in communication
3. Eye contact - Should see the listeners by face-to-face and not seeing the floor or ceiling
4. Facial expressions - It should communicate the response towards the communication
5. Voice - It should not be in a feeble tone. It should be a majestic voice
6. Involvement - Communicator should involve themselves completely towards the subject matters for communication.
7. Questions - Asking some questions towards the listeners to check whether they have understood the message delivered.
8. Visual Aids - It is better to use posters, video clippings etc. to explain the discussion
Guidelines for improving organisational communication
- Share important information
- Get information out quickly
- Stress benefits
- Don't be afraid to present opposing controversial view points
- Don't overload people with information
- Bring in experts to handle subjects you are not compatible with
- Ask managers at all levels to help spread the word within the organisation
- Follow-up communication with reinforcing materials and information
- If you are uncomfortable talking in front of groups, seek training
Ten commandments for good communication developed by the American Management Association
- Clarify before attempting to communicate
- Examine the purpose of communication
- Understand the physical and human environment when communicating
- Consult with others, where appropriate to obtain their support in planning communication
- Consider the content and overtones of the message
- Whenever possible, communicate something that helps or is valued by the receiver
- Follow-up your communication
- Communicate messages that are of short-run and long-run importance
- Be sure your actions support your communication
- Be a good listener
The effective communication process is an on going process, upon which the efficiency of internal communication system can be analysed. Thus an effective internal communication system helps in achieving organisational goals.
Summary
The OA is to be in the prescribed uniform inside the hospital premises. This will enable the patient and the attendar to identify the OA easily and ask for any help. The OA wears a clean and well pressed uniform which will give the OA a dignified look. As a health care professional the OA should possess some important qualities. They have to practice them in day to day activities. The OA should be aware of the law that governs medical professionals and should abide by the rules. This will enable them to executive their duties effectively and bring good reputation to the hospital.
Key points to remember
- The OA should be in a clean and well pressed uniform.
- Personal hygiene of the OA is to be impeccable.
- As a health professional the OA should have compassion for the patient.
- The OA should develop good communication skills.
Student exercise
Answer the following
- What are the purposes of wearing uniforms in the hospital?
- Write a short note about the consent form for operation.
- What are the procedures in nursing care, demanding special care and attention?
- Write a short note on personal hygiene.
- What are the qualities of a health care professional?
- What is the need for communication in the hospital?
- What are the barriers of communication?
- Mention the guidelines for an effective communicator.
- Write the ten commandments of good communication developed by the American Management Association.
