Ocular Diseases
Diseases of the Eyelid
Eyelids are movable curtains in front of the eyes. They protect the eyes from strong wind and injurious agents. Each eye has an upper and lower eyelid. The upper eyelid has a fibrous tarsal plate. Small glands are present on the lid, which open along the lid margins. The secretion of the glands lubricates the eye and facilitates smooth movement of eyelids. At the margins of each lid are 2 to 3 rows of hairs which form the eyelashes. The inner surface of the eyelids and eyeball are covered by a thin mucous secreting membrane called conjunctiva. The lower lid remains static in position while the upper eyelid moves with each blink. Lids are kept mobile by LPS (Levator Palpebrae Superiors) and circular muscles. Lids protect eyes from perspiration, FB (Foreign Body) particulate matter from strong light and wind. Eyelids distribute tear film uniformly by constant blinking and this keeps the eye moist and clean. Tears also keep the eye free from infection.
Congenital anomalies of the eyelids
- Crypto blepharon: Rare condition resulting in failure to differentiate into lid structures. Skin passes uninterrupted from forehead over the eyes to cheek
- Coloboma of lid: Small notch to absence of entire length of eyelid especially upper eyelid. This has to be corrected by plastic surgery
- Distichiasis: Two or more rows of eyelashes
- Epicanthus: Crescentic fold of skin running vertically between lids at inner canthus (nasally)
- Telecanthus: Normal interpalpable distance but wide intercanthal distance
- Palpable fissure slants: Upwards and downwards slants of palpable fissure as in Down's syndrome
- Ankyloblepharon: Fusion of the lid margins
- Congenital Entropion inward rotation of the eyelid
- Congenital Ectropion outward rotation of the eyelid
Anomalies of the Eyelid
I. Congenital (defects present at birth)
- Coloboma
- Epicanthus
- Blepharophimosis
II. Anomalies of position of lashes and lid margin
- Entropion
- Ectropion
- Ptosis
- Lagophthalmos
III. Inflammatory disorders
- Blepharitis
- Chalazion
- Hordeolum internum
- Hordeolum externum
IV. Lid Tumors
- Benign
- Malignant
V. Lid Injuries
- Lacerations
- Penetrating injuries
- Chemical burns
Trichiasis
Definition: The direction of eye lashes are changed causing irritation, watering and corneal abrasions.
Cause
- Chronic Blepharitis
- Herpes Zoster infection
- Trachoma
Treatment
Epilation or removing eyelash with forceps.
Phthiriasis Palpebrarum
| Definition | : Small louse and nits seen in root of eye lashes |
| Cause | : Poor hygienic condition |
| Symptoms | : Itching and irritation |
Treatment
- Eye lash clipping
- Removal of nits by forceps
- Delousing the patients
Blepharitis
Definition : It is inflammation of the eyelid margins. (Fig. 8.1)

Causes
- Seborrhea (dandruff)
- Staphylococcal infection
- Poor hygienic conditions
- Uncorrected refractive errors
- Diabetes
Types
| Features | Squamous | Ulcerative |
| 1. Scales | White | Yellow |
| 2. On removal of scales | No bleeding | Bleeding due to scales |
| 3. Caused by | Exfoliation | Staphylococci |
Symptoms
- Itching
- Watering (lacrimation)
- Photophobia
Treatment
- Improvement of general health
- Treatment of dandruff
- Lid hygiene
- Antibiotic eye ointment
- Correction of refractive error
- Screening for diabetes in adults and treating if present
External hordeolum (Stye)
Definition
Inflammation of follicle of the eyelash including the gland of Zeis.
Causative organism
Staphylococcus (a bacterial infection)
Risk factors
- Children and young adults
- Diabetes
- Very sick patients
- Uncorrected refractive errors
Symptoms and signs
- Pain and swelling of the lid margin
- Edema of lids
- Tenderness
Treatment
- Hot fomentation
- Antibiotic eye ointment
- Analgesic
- Treatment of refractive errors, blepharitis, diabetes
Hordeolum Internum
Definition
Acute inflammation of the meibomian gland.
Causative organism
Staphylococcus
Risk factors
Same as hordeolum externum
Symptoms
Same as hordeolum externum but more severe
Signs
- Point of maximum tenderness is away from lid margin
- Pus points on the tarsal conjunctiva
Treatment
Same as hordeolum externum
Chalazion
Definition
Chronic inflammation of the meibomian gland (Fig. 8.2 & Fig. 8.3)
Causes
- Blepharitis
- Chronic conjunctivitis
- Diabetes in adults
- Errors of refraction
Symptoms
Painless nodular swelling in the eye lid
Signs
- Well defined swelling
- Firm and non tender
- Eversion of the lid shows purplish discolouration of conjunctiva
Treatment
- Hot fomentation
- Antibiotic eye ointment
- Incision and curettage
Ectropion
Definition
Rolling in out of the margin of the eye lid. (Fig. 8.4 & Fig. 8.5)
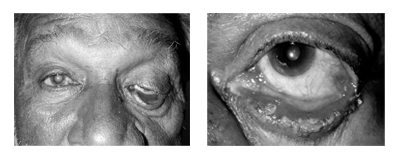
Type
| Senile | - Old age |
| Paralytic | - Paralysis of orbicularis seen in facial palsy |
| Congenital | - Present since birth |
| Mechanical | - Due to weight of swelling in the lower lid |
| Cicatrical | - Chemical burns |
Symptoms
- Epiphora : Because punctum is not apposed to the globe.
- Excoriation of skin around the lid
Treatment
Temporary
- Antibiotic ointment
- Adhesive tape to close the lid at night
Permanent
- Surgical corrections
Entropion
Definition
Rolling in of the lid margin with its lashes (Fig. 8.6 & Fig. 8.7)
Type
| Senile | - old age |
| Spastic | - excessive contraction of orbicularis oculi |
| Cicatrical | - due to scarring (trachoma, chemical burns) |
| Congenital | - present since birth |
| Mechanical | - due to weight of the swellings in the lid |
Symptoms
- Foreign body sensation
- Pain
- Lacrimation
Complications
- Corneal ulceration
- Corneal opacities
Treatment
Temporary procedures
- Adhesive tape : pulling the skin out with strip of plaster
- Cautery : over skin below lashes
- Soft contact lenses
Permanent procedures: Surgical
Lagophthalmos
Definition
Inadequate closure of eyelids when an attempt is made to close them.
Causes
- Facial nerve palsy
- Proptosis
- Patient in coma
- Deformity of upper lid
Complications
- Dryness of conjunctiva and cornea
- Exposure keratitis
Treatment
Temporary
- Artificial tear drops at day time
- Antibiotic ointment at night time
- Closure of lids with adhesive tape
- Soft contact lenses to prevent corneal damage
Permanent
Surgery: Tarsorrhaphy
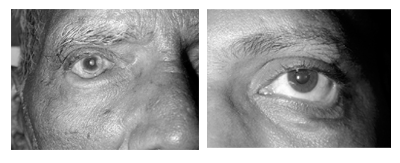
Ptosis
Definition
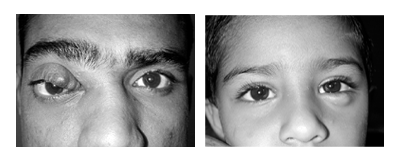
Drooping of the upper eye lid (Fig. 8.8)

Causes
- Old age
- Abnormalities in the development of muscles
- Malfunctioning of the nerves
- Injury or trauma in the eye
- Inflammation, diabetic, stroke, tumors, cancers, zaneurysms
- Mechanical
Congenital
Present from birth
Acquired
| Due to nerve damage | - 3rd nerve palsy |
| Muscle disease | - Myasthenia gravis |
| Mechanical | - Tumors, chalazion etc. pulling the lid down |
| Traumatic | - Following injury |
Treatment
- Neostigmine tablets are given for myasthenia disease
- Surgical correction is done in most cases
Tumors of the Eyelids
Benign
- Papilloma
- Molluscum contagiosum
- Naevus
- Xanthelesma
- Warts
- Hemangioma
- Neurofibroma
Malignant
- Rhodent ulcer (Basal cell carcinoma)
- Squamous cell carcinoma
- Meibomian gland carcinoma
Diseases of the Lacrimal System
Tears are secreted by the lacrimal gland and reach the conjunctival sac through tubes. Tears keep the cornea clean, wet and shining. There is a germicide called lysozyme in it. This protects the eye by killing microorganisms. The tears secreted evaporate to a great extent and the rest get collected in a small space near the nose. From there they reach the lacrimal sac, through two holes called lacrimal puncta and two tubes called canaliculi found in the eyelids near the nose. The lacrimal sac is placed in bony lacrimal fossa (a space in the nose near the eye).
When we cry or when we become emotional or when dust or smoke affects the eye, more tears are secreted. The excess tears reach the lacrimal sac and from there come out through the nose. That is why there is watering in the nose.
If there is obstruction in the canaliculi there will be watering in the eyes. Most importantly, the tears will collect in the lacrimal sac if there is obstruction in the tube connecting the lacrimal sac and the nose. This obstruction may be due to many reasons. If we press with a finger at the site of lacrimal sac the tears collected there will be driven back through the eye. In course of time, it will get infected and tears will turn into pus. This will result in chronic dacryocystitis. Middle aged people are generally affected. Women are more likely to be affected than men. Sometimes, lacrimal abscess will form in the lacrimal sac. There will be swelling and pain in the place where it is located. The abscess will burst and the pus will drain through a fistula. The abscess will heal or may become a lacrimal fistula.
The symptoms of lacrimal sac inflammation are watering of eyes, pus formation, small swelling at the place where the lacrimal sac is located. When it is pressed, the pus will be discharged. As pus with organisms is present near the eye, such patients run the risk of endangering the eye. Even when there is a small scratch injury to the eye, the pus in the sac will infect the cornea causing ulcer. In such conditions there is a possibility of losing eye sight permanently. In such patients sac must be removed first. The immediate danger to the eye is thus eliminated. But, as the path through which excess tears are removed is cut off, watering in the eye will continue. However, this will not affect the eye in any way. Another procedure is to make an ostium in the nose at the place where the sac is situated, and to create a passage between the surface of the nose and the sac so that the tears can flow to the nose. This offers near complete cure. In infants this defect is congenital, due to lack to development of the passage. From birth, they will have excess tearing with discharge. Most cases can be cured by administering antibiotic drops and giving massage at the lacrimal sac. If this does not offer remedy, the block or obstruction is removed by inserting a thin wire through the lacrimal sac and the tube connecting it to the nose (probing of the nasolacrimal duct), after giving anaesthesia. This procedure is called probing. If this fails in some children surgery becomes mandatory. If there is watering in the eye with discharge,an ophthalmologist must be approached to ascertain whether the problem is due to lacrimal sac.
Reasons for excess tearing
It is important to know the different reasons for tearing in the eye. With proper treatment excessive tearing can be stopped. Let us first see the obstruction in the lacrimal sac. There are two main reasons for tear secretion. It may be due to (a) excess secretion (b) inadequate drainage.
The tears in the eye go to the sac and from there reach the nose through a tube like structure. If there is obstruction in the sac, tears cannot reach the nose. So, it returns back to the eye and there is watering. If this defect is not corrected germs will collect there, multiply, and discharge will occur. There are two types of surgical procedures to correct this. One is Dacryocystorhinostomy - DCR. As elderly people cannot endure this, the second procedure is done without breaking the nose. Here the sac is removed. This is called Dacryocystectomy (DCT). This will destroy the place where germs collect. There will be no discharge but there will be tearing in the eyes.
This is seen in a few newborn infants too. The discharge must be cleared by massaging the lacrimal sac. This massage must be continued up to one year. Surgical procedure may be adopted later if management fails.
Other causes of tearing in the eye
The cornea is very thin and even a small injury to it or a speck of dust on it will result in redness, irritation and excess tearing. There are other reasons also. They are
- Foreign bodies like speck of dust, sand, and iron sticking onto the corneal surface
- Dust in upper eyelids will cause friction during lid movements (causing injury to the cornea)
- The eye lashes grow inward (Trichiasis)
- Elderly people will have a growth called concretion in the upper eyelid. This also will rub on the cornea and cause tearing.
- Abscess in the inner side of the lids
- Lagophthalmos
- Corneal ulcer
- Rise in intraocular pressure
- Conjunctivitis
- Defective vision. In-patients who do not wear glasses and strain themselves, there will be tearing. Some will have difficulty when the muscles do not function properly while reading. This can be corrected by simple exercises
- Pterygium and pinguecula may grow causing tearing
- Postoperatively sutures may cause irritation
- (Dry eye) tearing will be less. But such patients have a feeling of tearing
Lacrimal apparatus diseases are divided into 2 groups
Diseases of Lacrimal Gland
Infection: Acute dacryoadenitis
Tumors : Adenoma carcinoma, adenoma
Diseases of Lacrimal sac
Infection - Dacryocystitis
Tumors - Very rare e.g.: papilloma
Dacryocystitis
Definition
Acute or chronic inflammation of lacrimal sac. (Fig. 8.9 & Fig. 8.10)

Causative organisms
- Pneumococcus (most common)
- Streptococcus
- Staphylococcus
- Mycobacterium etc.
Causes
- Congenital deformation of the lacrimal drainage system
- Diseases of nose : deviated nasal septum
- Nasal polyps
- Infection spreading from naso-pharynx
- Trauma causing distortion of anatomy and stagnation of tears
Sequence of events
Obstruction at the junction of the lower end of lacrimal sac and the upper end of naso-lacrimal duct Stagnation of tears in the sac Predisposing to infection
| Stagnation of tears in the sac |
| Predisposing to infection |
Dacryocystitis
Types
- Acute dacryocystitis
- Chronic dacryocystitis
- Congenital dacryocystitis
Symptoms
Acute
- Sudden onset of pain, redness and swelling in the sac area
- Watering of the eyes
- Sometimes redness of the eyes
- Congenital - watering of one or both eyes since birth
Chronic
- Watering of the eyes
- Sometimes discharge
- Pus like material coming from lacrimal puncta when pressing over the sac area.
Diagnosis
- Acute : Syringing contraindicated
- Chronic : On syringing, fluid will regurgitate through the same punctum or upper punctum, Mucus or pus may also be seen in the regurgitant fluid.
- Congenital: 1-2 drops of 2% fluorescent dye instilled in the eye and after some time, a cotton swab is introduced in the nostril to see whether the dye has drained into the nose.
Complications
- Chronic conjunctivitis
- Can lead to infection within the eye after surgery in the eye
- Promote bacterial corneal ulcers
- Acute dacryocystitis may progress to orbital cellulitis, lacrimal fistula [skin opening in sac area].
Treatment
I. Acute Dacryocystitis
- Hot compresses: 3-4 times / day
- Broad spectrum systemic antibiotics
- Topical antibiotics: 4 - 6 times / day
- DCT (dacryocystectomy) or dacryocysto -rhinostomy (DCR) done after inflammation subsides.
II. Chronic dacryocystitis
- In younger age DCR is done
- In old age DCT is done
III. Congenital dacryocystitis
- Massaging and antibiotic drop instillation
- Probing : probe is passed down naso-lacrimal duct
- DCR if the above procedures fail to open lacrimal passages after 3 years
Dry Eyes
It is one of the most common problems treated by ophthalmologist.
Definition
There is decreased secretion of tears or deficiency in the composition of tears.
Causes
- Aging
- Hot, dry or windy climates
- High altitude
- Air conditioning
- Cigarette smoking
- Working on computer for long time
- Contact lens wearers
Symptoms
- Itching
- Burning
- Irritation
- Redness
- Blurred vision that improves with blinking
- Excessive tearing
- Increased discomfort after reading, watching TV, or working on a computer
- F.B sensation
Diagnosis
Schirmer test is done
Treatment
No permanent cure, can only relieve symptoms
I. Preservation of existing tears
- Reduction of room temperature
- Humidifiers
- Punctual occlusion
II. Supplementation of tears
| 1. Drops | - Methyl Cellulose |
| - Hydroxy ethyl cellulose | |
| - Hyper mellose | |
| 2. Ointments | - HPMC gel at bed time |
Diseases of the Conjunctiva
The most common conjunctival disease is conjunctivitis which is infective. Others being pterygium, pinguecula and subconjunctival haemorrhage.
Conjunctivitis
Definition
Infection of the conjunctiva
Classification
Infections
Bacterial
- Staphylococus aureus
- Haemophillus
- Gonococcal (Ophthalmic Neonatorum)
- Mycobacterium
Viral
- Adenovirus
- Varicella
- Herpes Zoster
- Mumps
- Influenza
Chalamydial (Trachoma)
- Chlamydia trachomatis
Table : 1
| Conjunctival congestion | Ciliary congestion | |
| i. Site | Fornices | Limbus |
| ii. Color | Bright red | Violet |
| iii. Depth | Vessels superficial | Vessels deep |
| iv. Branching | Dichotomously | Radially |
| v. 1.1000 epinephrine test | Whitens conjunctiva | No effect |
| vi. Disease | Conjunctivits | Iridocystitis, Glaucoma |
Allergic
- Simple allergic conjunctivitis
- Vernal catarrh
Trauma
Infective conjunctivitis
Symptoms
- Discomfort and foreign body sensations due to engorgement of blood vessels
- Sticking together of eye lashes due to discharge
- Photophobia and watering of the eye
- Defective vision due to thin layer of discharge on the cornea
- Haloes around light due to thin layer of discharge on the corneal surface.
Signs
- Discharge : causes sticking together of eyelashes especially when waking up in the morning
- Congestion : should be differentiated from other causes of congestion (redness) (Table:1).
- Subconjunctival hemorrhage: more common in viral conjunctivitis. Rupture of tiny conjunctival vessel.
- Follicles: Round swellings (0.5 - 2 mm) surrounded by tiny blood vessel in the tarsal conjunctiva, more commonly seen in viral conjunctivitis and allergic conjunctivitis.
- Papillae : Round swelling with blood vessels in the centre over the tarsal conjunctiva more commonly seen in vernal conjunctivitis.
- Pre Auricular Lymphadenopathy: Seen in viral, chlamydial infection
Treatment
- Frequent wash with luke warm saline solution to clear crusting and discharge
- Use dark glasses to prevent photophobia
- Broad spectrum antibiotic drops are used
- E.g.,: ciprofloxacin dosage hourly to 4 times depending on severity.
- Ointment: Tetracycline / gentamycin/ Chloramphenicol at bed time
To prevent contamination
- Patient must keep his hands clean and avoid touching around the eye.
- Personal belongings of the patient like towel, handkerchief, and pillow should be kept separately.
- Other family members if infected should be treated simultaneously.
Simple allergic conjunctivitis
Definition
Allergic reaction due to large amount of allergens reaching the conjunctiva
Causes
- Pollen grains
- Certain topical drugs e.g.. Neomycin
- Contact with pet animals
- Dust, cosmetics, chemicals
Treatment
- Removal of allergen
- Antihistamine tablets & drops
- Topical 2% Sodium chromoglycolate to prevent recurrence
- Corticosteroid drops in severe cases
Vernal conjunctivitis
Definition
Hypersensitivity reaction of conjunctiva to exogenous allergens
Causes
| Age | - 6-20 yrs, usually males |
| Seasonal variation | - Prevalent in summer |
| Exciting factors | - Dust, dry heat, pollens |
Symptoms
- Intense itching
- Discharge
- Photophobia, burning and foreign body sensation
Signs
- Cobble stone appearance due to papillary hypertrophy in the palpaberal conjunctiva
- Multiple small nodules around the limbus
- Trantas spots superficial white spots scattered around the limbus.
Treatment
- Cold compresses
- Disodium chromoglycolate 4 times / day reduces itching
- Topical steroids like dexamethasone 4 times daily and tapering dose depending on the severity. Long term use of steroids can cause cataract and glaucoma.
Ophthalmia neonatorum
Definition
Bilateral purulent conjunctivitis occurring in new born within first 3 weeks of life.
Causative organisms
- Gonococcus (Most common)
- Chlamydia
Mode of Infection
- Before birth - very rare
- During birth - face presentation is the most common
- After birth - from soiled linen
Clinical picture
Watering, redness & discharge.
Treatment
1) Prophylaxis
- Proper antenatal care of mother. Any vaginal discharge should be treated meticulously.
- Crede's prophylaxis: 1% silver nitrate is instilled into the baby's eyes immediately after birth.
2) Curative
Swab taken for culture and sensitivity
Gonococcal - Ciprofloxacin hourly for 3-5 days
Chlamydial - 1% tetracycline 2 times/day
Pterygium
Definition
It is a triangular growth on the conjunctiva encroaching on the cornea in the horizontal meridian, in the palpaberal fissure, either from the nasal or temporal side of bulbar conjunctiva or from both sides.
Cause
- U-V radiations
- Exposure to hot, sandy and dusty weather
Parts of Pterygium
Head - Apex of triangular fleshy growth
Neck - Constricted portion at the limbus
Body - Remaining bulky part
Symptoms
- Appearance of lesion on nasal or temporal side
- Dimness of vision due to obstruction of visual axis
- Redness and burning sensation.
Signs
- Decreased visual acuity
- Triangular fold of conjunctival fleshy growth encroaching upon the cornea
Treatment
- Stationary pterygium - no treatment (If inflamed - NSAIDS or steroids eye drops)
- Progressive pterygium - excision
- Recurrent pterygium - mitomycin C, Beta radiation
- Pterygium in the pupillary area - Excision of pterygium and keratoplasty
Subconjunctival Haemorrhage
Definition
Spontaneous rupture of conjunctival blood vessels
Clinical picture
Sectoral red patch under the conjunctiva where blood collects.
Causes
- Trauma
- Diabetic and hypertensives
- Sneezing
- Coughing
- Straining
- Lifting heavy weight
- Vomiting
Treatment:
None
Reassurance to the patient
Diseases of the Cornea
Cornea forms one fifth of the front part of the eyeball. It is a clear membrane, like colorless glass. It is circular with slight convexity and inner concavity. It has a diameter of 11mm with a thickness of 0.65mm at the periphery and 0.54mm in the centre. It has five layers. They are:
- Epithelium
- Bowman's layer
- Stroma
- Descemet 's membrane
- Endothelium
Endothelium is made up of a layer of hexagonal cells. It has contact with aqueous humour. Through it cornea gets nutrients and oxygen. Only when it is healthy the refractory nature of the cornea will be maintained.
Cornea is like a window to the eye. The rays of light enroute to the retina pass through it. If the cornea is not clear, the light rays cannot pass through, and vision will be affected.
It is important for us to know the diseases affecting the cornea. When it is affected, scars will be formed and eyesight will get diminished, leading to loss of vision. Even if all the other parts of the eye are healthy, a disease to the cornea will affect vision.
A) Corneal ulcers
- Bacterial ulcer
- Fungal ulcer
- Viral ulcer
- Parasitic ulcer
B) Degenerative Conditions
- Arcus Senelis
- Band Shaped Keratoplasty
C) Dystrophies
- Granular
- Macular
- Lattice
A) Corneal ulcers
Definition
It is defined as a break in the corneal epithelium with added infection
Route of Spread
| Exogenous route | - From outside source |
| Secondary route | - From adjacent structures like conjunctiva, sclera, uvea |
| Endogenous route | - Systemic sources |
Causative organisms
| Bacteria | Fungal | Parasitic | Virus |
| 1.Staphylococcus aureus | Candida Albicans | Acanthamoeba | Herpes simplex |
| 2.Pseudomonas | Aspergillus | Herpes zoster | |
| 3. Streptococcus | Fusarium | ||
| 4. E.Coli | |||
| 5. Klebsciella |
Symptoms
- Lacrimation (watering)
- Photophobia
- Pain
- Defective vision
Signs
- Edema of lids and blepharospasm
- Circum ciliary congestion
Localised area of necrosis - Vascularisation of cornea
- Hypopyon may be present
Investigations
Corneal Scraping
Done under local anesthesia. The material obtained is used for the following investigations.
- Gram and Giemsa stains for bacteria
- 10% KOH wet preparation for fungus
- Culture on blood agar for aerobic organisms
- Culture on Sabouraud's dextrose agar for fungus
| Features | Bacterial ulcer | Fungal ulcer |
| i. History of Injury | Non specific | With Vegetable matter |
| ii. Predisposing factors | Non specific | Immunocompromised, steroids |
| iii. Course | Rapid | Slow |
| iv. Symptoms and signs | Proportionate | Sign out of proportionto symptoms |
| v. Satellite lesions | Absent | Present |
| vi. Margins | Well defined | Feathery |
| vii. Hypopyon | Usually not seen | Usually seen |
Check the diabetic status of the patient Complications
- Perforation - (Hole in cornea)
- Corneal opacities
- Endophthalmitis or panophthalmitis
- Secondary glaucoma
Treatment
a. Control of infections
- Antibiotics are used until the ulcer heals - e.g., fortified gentamycin, Cefazolin, Ciprofloxacin
- Antifungal - e.g.,: Natamycin, Nystatin etc.
b. Rest to the eye
- Cycloplegics: atropine 1% eye ointment 2 times / day gives rest to eye by paralysing the ciliary muscle
- Dark glasses: protect the eye from irritating effect of strong light
c. Relief of pain
- Hot compresses
- Oral pain killers
d. Removal of any septic focus in the neighbourhood
- If sac is infected, it is to be removed without delay
e. Improve general health condition
- By control of diabetes and improving nutrition.
Don'ts in a case of corneal ulcer
- No Bandage
- No Steroid drop
- No Schiotz Tonometer
Viral ulcer (Dendritic ulcer)
Definition
Ulcer with a branched appearance caused by herpes simplex virus (Fig. 8.11).

Symptoms
Pain, watering and photophobia
Clinical signs
- The ulcer appears as star shaped or branched pattern
- Absent corneal sensation
- Enlarged and tender pre auricular lymph nodes
Treatment
- Antiviral drops or ointment (e.g.,: acyclovir eye ointment 3%)
- Steroids to suppress the host response
- Antibiotic eye drops to prevent secondary infection
B. Degenerative conditions
Keratoconus
Definition
Bilateral conical protrusion of central part of the cornea due to thinning
Symptoms
Defective vision due to irregular myopic astigmatism and watering due to rupture of hydrops
Signs
- Munson 's sign: bulging of the lower lid when patient looks down.
- Retinoscopy: scissoring reflex
- Ophthalmoscopy: oil drop sign
- Slit lamp:
- Thinning of cornea at the centre
- Prominent corneal nerves
- Fleischer ' s ring - iron deposits at the base of cone
- Keratometry ('K' reading) showing high astigmatism
Complications
Acute hydrops: rupture of Descemet 's membrane and seepage of aqueous in the corneal stroma and epithelium
Treatment
- Hard contact lens
- Penetrating keratoplasty
Arcus senilis
Normally seen at peripheral cornea
- Corneal degeneration
- Lesion: starts as crescent grey line around 12o clock and 6 o clock. Finally it becomes circular
- Site: periphery of cornea parallel to limbus. There is clear space seen between the lesion and the limbus
- Does not affect vision or vitality of cornea
C. Corneal dystrophies
Definition: condition in which cornea loses its clarity due to deposition of materials in various layers of the cornea
Features
- Usually inherited
- Not caused by outside factors like injury or diet
- Progresses gradually
- Occurs in otherwise healthy people
Symptoms
- Some detected on routine examination
- Some cause visual impairment
- Some cause repeated episodes of pain without visual loss
Types
- Epithelial dystrophy - Map-dot finger print dystrophy
- Stromal dystrophy - granular dystrophy, macular dystrophy and lattice dystrophy
- Endothelial dystrophy - Fuch's dystrophy
Diseases of the Lens
Cataract is a term applied when the human lens loses its transparency and becomes opacified. Hence light cannot pass through the lens in required levels and fall on the retina to produce an image.
1)Cataract
- Congenital
- Acquired
2) Dislocation of Lens
- Hereditary dislocation
- Traumatic dislocation
3) Congenital anomalies of lens
- Ectopia lentis
- Coloboma of lens
- Lenticonus
4) Secondary Glaucoma
- Phacomorphic
- Phacolytic
Cataract
Definition: Opacity of lens (Fig. 8.12)

Classification
A. Congenital cataract / developmental cataract
B. Acquired cataract
- Senile cataract
- Traumatic cataract
- Complicated cataract: Due to some ocular diseases like anterior uveitis, retinal detachment
- Secondary cataract: Due to systemic diseases e.g. diabetes mellitus
- Toxic cataract: Due to drugs e.g. miotics (pilocarpine, steroids)
Congenital cataract
Cause
- Maternal malnutrition
- Maternal infection by virus as in rubella
- Deficient oxygenation due to placental hemorrhage
Symptoms
Mother complaints that infant has:
- White reflex from pupil
- Inability to see properly in bright light
- Abnormal movements of eye as in squint or nystagmus
Differential diagnosis
Congenital cataract should be differentiated from retinoblastoma which is a malignant condition producing white reflex at the pupil.
Treatment
- Lens aspiration
- Lensectomy
B. Senile cataract
Definition: Cataract related to ageing process.
Symptoms
- Painless progressive decrease in vision
- Misty / foggy vision
- Fixed dark spots before the eye
- Uniocular double or distorted images of objects
- Coloured haloes
Signs
- White pupil in the severely affected eye
Types
- Cortical
- Nuclear
- Posterior subcapsular
Cortical cataract
Also called soft cataract.
Stages of development
| i. Immature cataract | : few areas of opaque lens is present |
| ii. Mature cataract | : entire lens becomes opaque |
| iii. Hypermature or the cortex becomes a Morgagnian cataract | : milky fluid and the nucleus is shrunken and yellow. Sinks to the bottom of lens capsule |
Nuclear cataract
- The opacity starts at the nucleus and gets intensified while cortex remains clear. Later stages opacity extends to the cortex also
- Initially tinted dark brown, becomes black.
- Colour is due to deposit of melanin in the nucleus
- Index myopia: Myopia due to increased refractive index of nucleus leads to gradual decrease in distant vision.
- Second sight: Myopia due to cataract neutralises the " plus power " of presbyopia. So a patient using presbyopic glasses for reading is able to read without any glasses when nuclear cataract sets in.
Posterior sub capsular cataract (PSCC)
- Opacity formed in front of posterior capsule at the centre and progress towards the periphery.
- Vision much affected during day time or in bright light (Fig. 8.13).
- Surgery indicated at a relatively early stage.

Treatment
1) Extra capsular cataract extraction
- Anterior capsule is removed
- Nucleus is extracted
- Cortical matter is aspirated
- Sutures are applied to close the wound
2) Phacoemulsification
- Anterior capsule is removed
- Cataractous lens is broken into pieces by ultrasonic vibrating instrument and aspirated within the eye itself.
- Scleral tunnel is made so no sutures are used.
3) Intraocular lens implantation (IOL)
- Artificial lens made of PMMA (polymethyl metha acrylate) is inserted,
- Site of implantation
- Posterior chamber in the capsular bag
- When posterior capsule is not intact - sulcus
- Anterior chamber - posterior capsule is deficient
Subluxation / dislocation of the lens
Definition
- Subluxation - displacement of the lens side ways but remains behind the pupil
- Dislocation - displacement of the lens either
- Forward - into the anterior chamber
- Backward - into the vitreous
- Ectopia lentis - congenital bilateral, subluxation or dislocation of the lens
Causes
- Congenital (ectopia lentis)
- Acquired
- Excessive stretching of zonules - trauma
- Degeneration of zonules - pseudo exfoliation
Clinical features
Mono ocular diplopia
- Unequal depth of AC
- Iridodonesis
- Phacodonesis
4. Lens induced glaucoma
Phacolytic glaucoma
| |
| |
| |
| |
| |
Phacomorphic glaucoma
- Intumescent (swollen)
- Shallow anterior chamber
- Secondary angle closure glaucoma
- Fixed dilated pupil
Note: (Pupil should never be dilated)
Glaucoma
The vision lost due to glaucoma cannot be restored. Vision once lost is permanently lost. Glaucoma must be diagnosed early and treated. It is a condition which causes an abnormal increase in pressure within the eye. The front part of the eye between cornea and lens can be divided into two chambers. The chamber between iris and cornea is anterior chamber. It is filled with a colourless, clear liquid called aqueous humour. Aqueous humour supplies nutrients and oxygen to cornea and lens. This liquid flows out through the filters in the anterior chamber angle. The liquid again fills up the chamber. This filling in and draining go on continuously and uniformly. In glaucoma if the outflow is blocked then the intraocular pressure increases. We call this state glaucoma. The pressure is normally between 11mm to 20mm of Hg. If it goes above the limit that is if the pressure increases it affects the optic nerve and gradually causes loss of vision.
Types of glaucoma
- The most common is chronic simple glaucoma or open angle glaucoma. The angle between the iris and the cornea is normal but the drainage filters get clogged from inside. In this type the patient loses his vision slowly without his knowledge. As the loss of vision takes place silently without symptoms, it is called silent thief of sight. First, the peripheral field of vision is lost. In course of time central vision is also affected. Such patients go to the ophthalmologist at an advanced stage.
- The second type is angle closure glaucoma. This disease causes headache, pain, watering and redness of the eye and loss of sight suddenly. The patients will see rainbow like circles, halos, around lamps. They will at once approach the doctor. In chronic cases such symptoms are not observed.
- In addition to these two, there are other types of glaucoma. In congenital types, the infants at birth will have big eyes like those of a calf. This is called Buphthalmos. The cornea will be big. Photophobia, redness and watering of the eye will be observed and the child will keep the face buried in the pillow. Other occasions are when there is trauma, there is inflammation or when the cataract is about to burst.
How is glaucoma diagnosed?
The following tests are conducted
- Slit lamp examination
- Tonometry
- Fundus examination
- Testing visual fields. The latest computerised equipment called computer field analysis is available and it will give accurate diagnosis.
- Gonioscopy
- Visual Acuity
Symptoms of glaucoma
- Frequent headaches in the mornings
- Frequent change of glasses
- Blurred, cloudy, vision
- After watching TV or cinema pain around the eyes
- Rainbow like halos (rings) around lamps
- Gradual loss of field of vision
- Defective night vision
However, one may have glaucoma without any of these symptoms.
Who will get glaucoma?
- At any age; generally above 40
- If some one in the family or any blood relation has glaucoma
- Diabetic patients
- African heritage
- People who change glasses frequently due to myopia
Treatment
There are three treatments available
- Medical treatment: Some patients suffering from glaucoma may be treated with eye drops and tablets. Depending on the severity of the intraocular pressure, one or two types of eye drops are used. Some may require tablets also. It is important that the treatment is continued according to the physician's directions.
- Laser treatment: They are called laser trabeculoplasty and Laser Iridotomy. Patients need not stay long in the hospital but can take up their work the next day.
- Surgery: If the medical and laser treatments are not effective, surgery is the only alternative.
Note the following
- Glaucoma is not a form of cancer.
- Trachoma and glaucoma are two different diseases.
- There is no connection between hypertension and glaucoma.
- There is no connection between glaucoma and block in lacrimal sac.
- Glaucoma is not an infectious disease.
- All people above 40 must get their eyes examined once in two years.
Glaucoma patients should be advised to
Follow instructions of the ophthalmologist.
- Eye drops must be used without fail
- Eye drops must be applied to the eye
- Must not stop treatment without doctor's advice
- People in the family and relatives must get themselves examined
- Must inform about it to other doctors when consulted
- It is not possible to cure glaucoma completely. But it is possible to control it and keep the vision by continuous treatment
Laser treatment for glaucoma
As already explained, when the intraocular pressure increases beyond normal limits, the eye is affected by glaucoma. The aqueous humour fills the anterior chamber. The aqueous humour is the clear fluid that flows through the inside of the eye, nourishing the lens, the iris and the inside of the cornea. This fluid is not the same as tears, which bathes the outside of the eye. When aqueous humour secretes more or when the passage draining it is blocked, intraocular pressure will increase. In Schiotz scale normal pressure should be between 15mm and 20mm Hg.
Glaucoma affects the optic nerve connecting the eye and the brain. The symptoms, as already indicated, are pain in the eye, headache and seeing rainbow - like halos around lamps.
In laser treatment, a hole is made through the iris with a laser. This enables the liquid to flow from the chamber behind the iris to the front chamber. Normally this treatment takes just 5 minutes. It is painless and needs no injections. The patient needs no hospitalisation. Only after microscopic examination of the post treated, one could decide whether more laser treatment is necessary. This treatment is called laser iridotomy.
Laser trabeculoplasty
The liquid in the front chamber passes through minute sieve-like structures and reaches the canal and then onto the blood vessels. Due to ageing, changes take place in the eye and some solid particles get deposited on the sieve like structure. This causes blockage. Because of this, pressure gradually increases. This is the cause for open angle glaucoma. The side vision of the patient will be slowly lost without his/her knowledge. Some patients will have headache, and need to change glasses because of myopia. There are possibilities of one getting open angle glaucoma if there is a family history of diabetes.
In the laser treatment for open angle glaucoma, some parts of the sieve like structure are burnt by directing laser beams. The basic principle is to shrink the muscles by directing laser beams on them. The parts around the burnt out place will open up, allowing the liquid to pass through. In the first treatment usually half of the affected portion is subjected to laser treatment. So two separate treatments are possible for each eye.
When surgery does not help in certain glaucoma cases to reduce pressure, laser treatment helps to open up the closed tubes. When high pressure cannot be controlled by eye drops or surgery, the liquid secreting part is subjected to laser cyclo photocoagulation. Immediately after laser treatment, some eye drops are applied, pressure is reduced and the eye is kept without movement. The patient must wait for an hour. Then the pressure is measured. After ascertaining the pressure is stable, the patient is sent home.
An additional dose of eye drops will be given on the day of the treatment and it must be applied thrice a day for a week to the eye which has undergone treatment. The medicines already given must be continued. There must be an interval of 10 minutes between applying two medicines.
Refractive Errors
Optics of the eye
Emmetropia (No refractive error)
When light rays coming from a distant object are focused on the retina.
Ametropia (Refractive error)
When light rays coming from a distant object are not focused on the retina.
Types of refractive error
- Myopia (near sighted)
- Hypermetropia (far sighted)
- Astigmatism
Myopia
Definition
When light rays coming from a distant object are focused in front of the retina.
Types
- Depending on the mechanism
- Axial myopia : anterior-posterior length of eye ball is more than normal (long eye ball)
- Curvature myopia : Curvature of cornea / lens is more than normal
- Index myopia : Refractive index of nucleus is more than Normal (as in nuclear cataract)
- Clinical
- Congenital myopia: Present at birth
- Developmental Myopia: common. The power increases during adolescence and then remains steady. (< 6D)
- Pathological myopia: The power rapidly progresses and requires frequent change of glass. (> 6D)
Symptoms
- Defective vision for distance
- Discomfort after near work
- Black spots seen floating before eye
- Flashes of light
Signs
- Eyes are prominent
- Retinoscopy error is myopic
- Ophthalmoscopy
- Large disc
- Crescent around the disc
- Tiggroid fundus
Treatment
- Concave lens (as spectacles)
- Contact lens
- Radial keratotomy
- LASIK with excimer laser
Hypermetropia
Definition
Rays coming from a distant object are focussed behind the retina.
Types
Depending on mechanism
- Axial hypermetropia : Anterior posterior length of eye ball is less (short eye ball)
- Curvature hypermetropia: Curvature of cornea / lens or both flatter than normal.
- Index hypermetropia: Refractive index of various media are less than normal.
Depending upon power of accommodation
- Latent hypermetropia : Hypermetropia which is corrected due to tone of the ciliary muscles.
- Manifest hypermetropia : Hypermetropia which is not corrected by tone of the ciliary muscles.
- Facultative Hypermetropia : Hypermetropia which is corrected by contraction of ciliary muscle (act of accommodation)
- Absolute hypermetropia : Hypermetropia which cannot be corrected by contraction of ciliary muscle (act of accommodation)
Symptoms
- Eye strain after near work
- Headache after near work
- Feeling of blurring and dryness in the eye.
Signs
- Apparent divergent squint
- Anterior chamber is shallow
- Fundus:
- Disc is small
- Vessels tortuous
Treatment
- Convex lenses
- Contact lenses
Astigmatism
Definition
When light rays from distant objects cannot converge at a point on the retina due to unequal refractive power in different meridians.
Types
1. Regular astigmatism: Refractive error changes uniformly from one meridian to the other. It is further divided into
- Simple astigmatism: one focus falls on the retina and the other focus falls in front or behind the retina.
- Simple myopic astigmatism: when other focus falls in front of retina
- Simple hypermetropic astigmatism: when other focus falls behind the retina.
- Compound astigmatism: when both focal lines fall
- in front of retina - compound myopic astigmatism
- behind the retina - compound hypermetropic astigmatism
- Mixed astigmatism: when one focus falls in front of the retina & other focus falls behind the retina.
2. Irregular astigmatism: Refractive error changes differently in different meridians.
Treatment
Regular astigmatism - Glasses and contact lenses.
Irregular astigmatism - Contact lenses
Presbyopia
Definition
Loss of accommodation power due to aging.
Causes
- Lens matter becomes less elastic
- Weakening of ciliary muscles.
Symptoms
- Difficulty in reading small prints especially in dim light or evenings
- Inability to perform near work. E.g.) threading a needle etc.
- Fatigue or headache while doing near work.
Treatment
Convex spherical lenses are prescribed or added to existing glasses in the following manner.
Squint
Squint is not a sign of luck. It is a state which affects appearance and eyesight.
What is squint? How does it happen?
When we see an object with both eyes at the same time, they work together. Though two images fall on the retina, the sense of sight is transmitted by the optic nerve to the brain where both images are superimposed. We see one object in its dimension and colour. The six ocular muscles connected to the eyeballs are responsible for their movement. This enables one to move the eyeball up or down and sideways. Only if the movements are simultaneous, we can see objects like this. All the 12 muscles must coordinate in this action. If the eyes are not straight, the sensation of the brain will be different between the two eyes. The brain will take the message from the powerful eye and reject that of the other eye. If this is not rectified one will have double vision. And the eye whose image is ignored will have sight slowly deteriorated.
In short, in certain abnormal conditions when one eye fixates at the object and the other eye turns in a different direction, this is called the crossing of the eyes or ' squint '. The squinting eye is often referred to as the lazy eye or the crooked eye. The scientific name for squint is strabismus.
The squint eye may turn in any direction, in, out, up or down. The infant ' s eyes are not developed enough to see clearly and to work together as a team and therefore, they wander about giving at times the appearance of crossing. This should disappear as child grows. If it continues after 6 months, the child needs the attention of an eye specialist. It must be noted that squint in the infant may be an early symptom of retinoblastoma.
Parents must watch their children from infancy to find whether they move the eyes together, or whether there is extraordinary movement. Some children may keep their eyes on one side. The cornea of one eye will appear slightly deflected when the child is tired, or sick and in bright light. The habit of closing one eye, rubbing the eyes often, keeping the objects close to the eyes are other symptoms. Such children must be taken to the eye specialist immediately. 5 percent of the children between 3 and 5 years have one eye defect or another. In India it is estimated that one crore children have eye defects.
Squint affects the sight, personal appearance and personality of the children. A squint child's playmates ridicule him/her and he/she becomes shy and withdrawn.
Plan of treatment
- Glasses to correct the fault
- Patching of the good eye
- Applying eye drops or ointments
- Special types of exercises
- Operation
Patching of one eye
To induce the lazy eye to function properly, the good eye is patched for a few week or even months. This is one kind of treatment. This will help in the correction of double vision. Even when glasses are prescribed for defective vision, they can be worn along with the eye patches. Children must be encouraged by parents and teachers to follow this strictly. They must consult eye specialists often to examine the eye to estimate the progress. For this treatment to be effective it must be started before 3 years. But it can be undertaken at least before 10 years.
Instead of patching an eye, eye drops can be applied to the good eye. Dilate the pupil, reduce its sight and induce the lazy eye. But this is usually not desirable.
Out of the six muscles that control the movement of the eye, one of the pair may be strong and another weak. In such cases the eye will be pulled to the strong side. This also causes squint. Squint can be corrected by surgery.
Classification
| Squint | |
| ↓ | |
| | |
| Latent Squint (Heterophoria) | Manifest Squint (Heterotropia) |
| Non paralytic (Concomitant) | Paralytic (Non-concomitant) |
| Convergent (Esotropia) | Divergent (Exotropia) |
Heterophoria
In this condition the eyes look apparently straight. But when one eye is covered, the covered eye deviates. On removing the cover the eye becomes straight.
Types
| Esophoria | : Eye deviates inwards |
| Exophoria | : Eye deviates outwards |
| Hyperphoria | : Eye deviates upwards |
| Hypophoria | : Eye deviates downwards |
Under normal conditions the 2 eyes are kept in check by power of fusion.
Heterotropia
The eyes are deviated in primary position. Depending on the direction of deviation they are of following types.
| 1. Exotropia | : Deviated outwards |
| 2. Esotropia | : Deviated inwards |
| 3. Hypotropia | : Deviated downwards |
| 4. Hypertropia | : Deviated upwards |
Clinical investigations
- Hirschberg test
- Cover test
- Prism vergence test
- Maddox rod test
- Worth four dot test
- Hess charting
- Diplopia charting
- Synoptophore
Goals of treatment
- Good visual improvement in both eyes
- Straight eyes (cosmetic)
- Eyes working together for binocular vision (functional)
Treatment : 4 O'S
- Optical: Best corrected glasses are prescribed
- Orthoptic exercises
- Occlusion therapy : Strabismus associated with amblyopia is treated by occlusion
- Operation : Most common and successful method done for cosmetic and functional purpose
Amblyopia (Lazy eye)
Definition: Decrease in visual acuity without any diseases in the eye.
Features
- Usually unilateral
- Develops between 6 months to 6 years of life
Types
- Strabismic Amblyopia: Amblyopia present in the squinted eye, as it is not used for seeing objects.
- Anisometropic Amblyopia: Where there is difference in refractive power between both eyes. The eye with very blurred image is not used and this leads to amblyopia.
- Ametropic Amblyopia: In this condition both eyes suffer from high refractive error. This results in blurred image. If it is not corrected in early childhood amblyopia results.
- Amblyopia Exanopsia: Amblyopia develops because the light does not reach the retina during first few months or years of life, as in congenital ptosis or cataract
Treatment
- Removal of any opacity in the media
- Full correction of refractive errors
Occlusion therapy: The normal eye is occluded and child is forced to see with the amblyopic eye. When vision is equalized, surgical correction is done to put the eyes straight.
Diseases of the Retina and Vitreous
Retina is an important part of the eye and it is made of minute structures. It is the inner most layer of the three-layers of the eye. The retina is made of nerve fibres, which end in the optic nerve. There are photosensitive rods (cylindrical cells) and a layer of nerve fibres under it. At the back there is the yellow spot which is very sensitive. For the object to be seen clearly the rays must converge on it. Rods help to perceive the intensity of light and the cone cells help to identify the colour of the object. Rod cells help in night vision and cone cells in day vision. The concavity inside the retina is filled with colourless clear jelly called vitreous which helps to keep the three layers apposed to each other.
When the retina is affected by congenital defects, injury to the eye, other physical ailment or old age, the patient may lose vision (Fig. 8.14).
Diseases of vitreous
Some common problems of the vitreous are
- Floaters
- Vitreous hemorrhage
1. Floaters
They are various kinds of opacities moving in front of the eye. They are due to presence of opacities in the vitreous which cast a shadow on the retina. They are a common complaint and are usually harmless.
Causes
- Blood in vitreous
- Diabetic retinopathy
- Vein occlusion
- Trauma
- Degeneration of the vitreous
- High myopia
- Aging
- Inflammatory exudates
- Retinitis
- Uveitis
- Optic neuritis
Synchysis scintillans- cholesterol crystals in the vitreous
Management
Treatment is that of the cause in most cases.
Vitreous Hemorrhage
Definition: bleeding into the vitreous (Fig. 8.15)

Source of hemorrhage: blood vessels in the retina
Causes
- Trauma to the eye
- Diseases of the blood vessels
- Diabetic retinopathy
- Retinal vein occlusions
- Inflammation of the retinal veins
- Diseases of retina
- Retinal tears
- Retinal detachment
Management
- Blood usually gets absorbed over a few months, hence observation initially
- Vitrectomy: surgical method of removing vitreous if blood does not get absorbed
Diseases of the retina
Some of the common and important diseases are;
- Diabetic retinopathy
- Hypertensive retinopathy
- Retinal vein occlusions
- Retinitis pigmentosa
- Retinal detachment
- Central serous retinopathy (CSR)
- Retinoblastoma
1. Diabetic retinopathy
It is one of the most important ocular manifestations of diabetes. It is now a major cause of blindness in developed countries and is rapidly becoming an important cause of preventable blindness in developing countries.
Definition
It is a change seen in the retina of patients suffering from diabetes mellitus. Control of blood sugar level decreases the risk of developing severe diabetic retinopathy.
Classification
1. Non proliferative diabetic retinopathy Ophthalmoscopic features (Fig. 8.16)
- Micro aneurysms
- Hemorrhages
- Hard exudates
- Retinal oedema

2. Proliferative diabetic retinopathy
Ophthalmoscopic features (Fig. 8.17)
- New vessels at the disc (NVD)
- Fibrovascular bands
- Vitreous detachment
- Vitreous hemorrhage

Investigation
- Urine and blood sugar examination
- FFA (fundus flourescein angiography)
Management
- Medical treatment: good diabetic control,
- Laser treatment: photocoagulation- to stop leaking from retinal vessels and bleeding from new vessels
- Surgical treatment: vitrectomy is done in case of vitreous hemorrhage, traction retinal detachment
2. Hypertensive retinopathy
vascular changes in the retina associated with systemic hypertension
Clinical features
Grade I - mild generalised narrowing of arterioles, particularly of small branches
Grade II - marked generalized narrowing associated with focal narrowing of arterioles
Grade III - grade II changes and also hemorrhages, cotton-wool spots and hard exudates
Grade IV - all changes of grade III plus papilloedema
Management
No special management is required for the retinopathy as most of the changes are reversible with adequate control of blood pressure.
3. Retinal vein eclosion
More common than the artery occlusions, it affects elderly patients in sixth or seventh decades of life.
Risk factors
- Hypertension
- Diabetes
- Arteriosclerosis
Clinical features
- Sudden loss of vision
- Oedema and hemorrhages all over the fundus including the macula
Complications
- Neovascular glaucoma: occurs in 50% of cases within three months (so called 90 days glaucoma)
- Vitreous hemorrhage
- Proliferative retinopathy
Treatment
- Proper control of diseases like hypertension, diabetes etc.
- Laser photocoagulation: for macular oedema and new vessels
Retinitis Pigmentosa
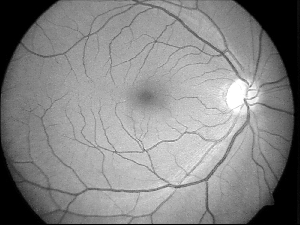
Definition: It is a hereditary condition of the retina affecting the rods (Fig. 8.18).

Clinical features
- Night blindness (nyctalopia)
- Tubular vision: advanced cases
Fundus changes
- Waxy pallor of disc
- Narrowed vessels
- Bony spicule pigmentation
Treatment
- No permanent cure at present
- Supportive treatment
- Vitamin A
- Low vision aids - night vision devices, field expanders etc.
- Visual rehabilitation
- Genetic counselling- no consanguineous marriage (marriage among relatives)
- Affected individuals discouraged to have kids
4. Retinal Detachment
Definition: Separation of the retina from the retinal pigment epithelial layer (Fig. 8.19).

Risk factors
- Myopia
- Retinal degeneration
- Trauma
Symptoms
- Floaters
- Flashes of light (due to excitement of retina by vitreous movements)
- Early stages - field defects
- Sudden painless loss of vision - (in large and central detachments)
Signs
- Direct ophthalmoscopy: shows grey reflex instead of normal pink reflex
- Indirect ophthalmoscopy: detached retina is grey, wavy and moves with eye movements -retinal break is seen
Treatment
Surgery: scleral buckling procedure
Central Serous Retinopathy (CSR)
Definition: It is due to detachment of retina in the macular region due to accumulation of fluid resulting in defective vision (Fig. 8.20).

Causes: not known
Symptoms
- Sudden onset of painless loss of vision
- Central scotoma (dark area)
- Micropsia (objects appears small)
- Metamorphopsia (irregularity of the objects)
Signs
- Ophthalmoscopy
- Mild elevation of macular area
- Foveal reflex is absent
Treatment
- Reassurance to the patient (usually resolves spontaneously without any treatment)
- Long standing cases (more than 4 months) : laser photocoagulation
7. Retinoblastoma
Definition: it is a malignant tumour of the retina occurring in children under 5 years. It is the most common intraocular malignant tumour of childhood. (Fig. 8.21)

Symptoms
- White reflex over the pupil (leukocoria)
- Squint
Signs
Indirect ophthalmoscopy: elevated fungating mass with satellite lesions seen in the retina.
Treatment
- Radiation therapy, chemotherapy
- Photocoagulation
- Cryotherapy
- Enucleation / excentration
Eale 's disease
Eale's disease is one in which young people have haemorrhage in the retina. Eale 's disease is generally found among young persons of 20 to 30 years. 70 percent of them are men. About 70 to 85 percent have both eyes affected.
Diseases of Orbit
The eye along with its surrounding structures like connective tissue, nerves, blood vessels, fat, muscles and glands have the potential to give rise to virtually any known neoplasm anywhere in the body. Certain types of tumors are more common and specific to this organ. A brief discussion of the more important tumors follows.
Common orbital diseases of children
- Orbital cellulitis
- Rhabdomyosarcoma
- Capillary hemangioma
- Dermoid and epidermoid cysts
- Leukemia
- Lymphangioma
- Psueudotumor
- Optic nerve glioma
- Metastatic neuroblastoma
- Neuro fibroma
Common orbital diseases of adults
- Thyroid related ophthalmopathy
- Pseudo tumour
- Cavernous haemangioma
- Lacrimal gland tumour
- Lymphoma
- Lymphangioma
- Meningioma
Proptosis
Definition: forward protrusion of the eyeball beyond the orbital margin.
Causes
Inflammatory
- Acute - orbital cellulitis
- Chronic - pseudotumor
Neoplastic
- Benign - dermoid
- Malignant - rhabdomyosarcoma
Parasitic
- Cysticercosis
- Hydatid cyst
Vascular- retrobulbar haemorrhage
- Orbital varices
- Aneurysm
Systemic diseases
- Thyroid ophthalmopathy
- Leukaemic deposits
Measurement of proptosis: Exophthalmometry
Investigations
- Thyroid function test
- X-ray orbit
- USG
- CT and MRI
- Biopsy
Treatment
- Medical - for orbital cellulitis, thyroid disease.
- Radiotherapy- for secondary deposits and malignant tumours
- Surgical a. tarsorrhaphy: to protect the exposed cornea, b. orbitotomy to remove the tumour
Thyroid ophthalmopathy
It is the most common cause of both unilateral and bilateral proptosis in adults.
Ocular manifestations
- Retraction of eyelids
- Lid lag
- Lagophthalmos - incomplete closure of eye lids
- Infrequent blinking
- Increased lid pigmentation
- Extra ocular muscle palsies
Investigations
- Thyroid function test: T3 and T4 levels
- USG: shows enlargement of extra ocular muscles
- CT scan: enlargement of muscles
- Optic nerve compression can be demonstrated.
Orbital cellulitis
Definition: infection of the fat and cellular tissues of the orbit.
Causes
- Sinus infection
- Penetrating orbital injury
- Thrombophlebitis
- Post operative: following enucleation of the globe
- Dental or naso-pharyngeal infection. Causative organism: streptococcus, staphylococcus, haemophilus
Types
- Preseptal
- Orbital
Symptoms
- Pain and swelling of the lids
- Lacrimation and photophobia
- Diplopia due to limitation of movements
- Impairment of vision at later stages
- Frequently associated with fever
Signs
- Lid oedema and tenderness
- Conjunctival congestion
- Proptosis
- Limitation of ocular movements
- Ophthalmoscopy: features of optic neuritis in severe cases
Complications: cavernous sinus thrombosis
Treatment
- Admit the patient
- Broad spectrum antibiotics systemically
Neuro ophthalmology
Some of the common and important diseases in neuro ophthalmology are
- Optic neuritis
- Papilloedema
- Optic atrophy
- Cranial nerve palsies
Optic neuritis
Definition: Inflammation of the optic nerve
Causes
- Idiopathic
- Childhood infection (e.g.,: measles, mumps)
- Viral infection (e.g.,: encephalitis, herpes zoster)
- Systemic diseases (e.g.,: syphilis, tuberculosis)
- Local inflammations (e.g,: sinusitis, meningitis, orbit)
- Intraocular inflammation
Symptoms
- Uniocular sudden loss of vision
- Pain behind the eye ball particularly while moving
Signs
- Visual acuity may be 6/60 or less
- Pupil: relative afferent pupillary defect
- Colour vision: defective
- Field defect: central, centrocaecal scotoma
Fundus
- Hyperemia of the disc
- Oedema of the disc
- Small hemorrhages on the disc
Treatment: systemic and oral steroids
Papilloedema
Definition: Non-inflammatory swelling of the optic disc produced by raised intracranial pressure.
Causes
- Congenital: e.g.,: aqueductal stenosis
- Space occupying intracranial lesions
- Head injury
- Infection: meningitis and encephalitis
- Malignant hypertension
Symptoms
a. General symptoms:
- Headache
- Vomiting
b. Ocular symptoms
- Visual acuity normal
- Transient blackout of vision for few seconds
- Fields: enlargement of blind spot
Signs
- Blurring of disc margin
- Disc hyperemia
- Dilated vessels
- Hemorrhages on disc
Treatment: Given according to the cause of the disease.
Optic atrophy
Definition: death of the optic nerve fibres characterized by pallor of the disc.
Causes
- Glaucoma
- Trauma
- Retinitis pigmentosa
- Central retinal artery occlusion
- Papilloedema
- Optic neuritis
Symptoms
- Sudden or gradual loss of vision
- Defective color vision
Signs
- Visual acuity impaired
- Relative afferent pupillary defect (RAPD)
Fundus
- Pallor of disc
- Narrowing of blood vessels
Treatment: The specific cause should be treated before the onset of optic atrophy. The damaged part of optic nerve cannot be recovered.
Cranial Nerve Lesions
Third Nerve Palsy
- Ptosis (falling down of upper eyelid) - levator muscle paralysis
- Restriction of adduction- medial rectus paralysis
- Restriction of elevation- superior rectus paralysis
- Restriction of depression - inferior rectus paralysis
Fourth Nerve Palsy
- Double vision on looking down
- Paralysis of superior oblique muscle
Sixth Nerve Palsy
- Double vision on looking to the side of lesion
- Paralysis of lateral rectus muscle
Diseases of the uvea
Uveitis
Definition: inflammation of the uvea (iris, ciliary body and choroid)
Inflammation of iris - Iritis
Inflammation of ciliary body - Cyclitis
Inflammation of choroid - Choroiditis
Classification
- Anterior uveitis (irido-cyclitis) : inflammation of the iris and the ciliary body.
- Intermediate uveitits - inflammation of ciliary body.
- Posterior uveitis: inflammation of the choroid with or without cyclitis.
- Pan uveitis : iritis + cyclitis + choroiditis
Anterior uveitis
Causes
- Bacteria - tuberculosis, leprosy
- Virus - herpes simplex, herpes zoster
- Fungus - histoplasmosis
- Parasite - toxoplasmosis, toxocariasis
- Systemic diseases - joint diseases
- Trauma
Symptoms
- Pain
- Redness
- Defective vision
- Photophobia
- Watering
Signs
- Vision diminished
- Conjunctiva - circumciliary congestion
- Cornea - oedema keratitic
- Keratitic precipitates (KP 's): cells that stick to the back surface of cornea (endothelium)
- Anterior chamber
- Cells : inflammatory cells
- Flare : due to increased protein content of the aqueous
- Hypopyon: large accumulation of inflammatory cells in the lower part of anterior chamber.
- Pupil - small and irregular (sluggish pupillary reaction)
- Synechiae
- Sticking of iris to the lens capsule (posterior synechiae)
Treatment
Mydriatics: e.g., Atropine eye drop or ointment (1%)
Steroids
- Topical : dexamethosone - 1 drop hourly to 4 times per day - eye ointment at bed time
- Subconjunctival - 0.5 ml per day dexamethasone
- Oral - 1mg prednisolone per kg per day and tapered as condition improves, Painkillers - paracetamol or ibuprofen
Complications
- Band keratopathy
- Complicated cataract
- Retinal detachment
- Optic neuritis
Posterior Uveitis (Choroiditis)
Symptoms
- Defective vision
- Floaters - seeing black dots
- If central area is involved
- Metamorphopsia (distortion)
- Micropsia (objects appear smaller)
- Macropsia (objects appear larger)
- Photopsia (flashes of light )
Signs
Requires indirect ophthalmoscopy to detect the various abnormalities in the retina and choroid.
Treatment
It depends upon the cause. It is better to refer the case for investigation and treatment in a well equipped eye center.
Loss of sight due to malnutrition
The eye specialists of countries like India, Srilanka, Bangladesh, Nepal, Indonesia and Thailand encounter many children with nutritional blindness. Many countries in Africa and South America also have large incidence of such cases. The deficiency of vitamins affects the eye, and it is estimated that about half a million children become blind every year as a result of this deficiency.
Reasons for children losing eye sight
- Vitamin A deficiency
- Infection in the mother 's vagina during child birth
- Injury due to hits from sticks, crackers
Children below five years are affected by vitamin A deficiency. The effects are seen in the eye in the form of dryness, is called Xerophthalmia which means 'dry eye'. Night blindness or inability to see in dim light is one of the early manifestations of the disease. There are structural changes in the eye. Conjunctiva becomes dry and wrinkled. Pearly grey, elevated patches called Bitot's spots may be seen. In severe deficiency the cornea is also involved resulting in complete loss of vision.
Night blindness is recorded as early as 1600 B.C and the liver of the sheep was given to treat it. Now we know that liver has Vitamin A. Jacques Gilmo described the condition in 1585. A Dutch man at the same time wrote a poem about night blindness and liver given as cure.
Inadequate diet, diarrhoea, measles and diseases of lungs aggravate Vitamin A deficiency. Vitamin A deficiency is noticed in most economically backward families.
Causes for Vitamin A deficiency
Poverty, ignorance and faulty food habits are responsible for vitamin A deficiency. Inadequate intake of food rich in vitamin A is the main reason. When pregnant women have the deficiency, their children have less vitamin A in their liver. It must be noted that 95 percent of Vitamin A is stored in the liver. When the child is breast fed, the child gets poor supply of Vitamin A from mother's milk. Again the deficiency occurs when supplementary food is delayed after four months. When the infant has diarrhoea, measles and other infections of lungs, Vitamin A in the body gets depleted. Further protein-energy deficiency and other infections affect absorption and storage of Vitamin A in the body leading to deficiency.
Signs of Vitamin A deficiency
Night blindness
The first manifestation of Vitamin A deficiency is night blindness. This is caused by damage to the cylindrical light sensitive rod cells in the retina. Patients with this defect cannot see in dim light, and at night. The disease can be noticed when the child falters in the dim light or when he is not able to eat properly. They must be given treatment at once.
Bitot spots
This symptom was first noticed and explained by the French doctor Bitot in 1863. Conjunctiva becomes dry and wrinkled. Pearly grey elevated patches are seen. The number of children below age five affected by this is less; it is high in school age children.
Dry conjunctiva
The conjunctival epithelium becomes dry due to lack of tears. When the disease becomes acute, cornea loses its brightness and will be bluish white.
Corneal ulcer
There are other reasons for corneal ulcers. But if it is due to the dryness of cornea, the layer of the cornea will be partly or fully damaged. This results in lesions, making cure difficult.
The cornea becomes soft and dissolves. The liquid inside will come out as the eye ball shrinks.
Lesions or scars appear in the cornea when there is injury or infection. Children with Vitamin A and protein deficiency are more susceptible.
These signs and symptoms need not take place in that order. If it is accompanied by infection like measles, cornea becomes ulcerated.
Treatment
As soon as Vitamin A deficiency is noticed in children between 1 and 6 years, Vitamin A of 200,000 IU must be orally administered. It must be repeated next day and after one month.
For children below 1 year or weighing below 8 kilo, the same treatment is given with a reduced dose of 100,000 IU.
Prevention of Vitamin A deficiency
Vitamin A is a fat-soluble vitamin and is present in animal foods such as butter, eggs and liver. It is stored in the liver and used by the body whenever required. When the child has an attack of diarrhoea, measles etc., administering 2 lakhs IU of Vitamin A will prevent deficiency. Likewise breast feeding mothers must be given a similar dose of Vitamin A. The children will get it. Mothers must be given Vitamin A within a month of child birth. When the child finds it difficult to see sunlight, it must be given vitamin A supplement. The breast milk immediately after child birth is rich in vitamin A and it must be given to infants. Breast feeding for 6 months ensures a good supply of it. Vitamin A is found in green leafy vegetables, drumstick leaves, carrots, curry leaves, mint and coriander leaves, yellow pumpkin, papaya, radish, tomatoes and mangoes, milk, eggs, fish, liver, fish liver oil etc. Papaya is rich in Vitamin A. There are false beliefs about eating it. Children and mothers can eat it without fear. Children below five years must be given one glass of milk a day.
50 grams of leaves will give enough Vitamin A for adults. Children below six get enough Vitamin A if they are given 50 grams of any leaves cooked in any form liked by them. After cooking it will fill a tablespoon. It can be mixed with other items of food. Small children can be given papaya and mangoes rich in carotenes or milk, egg and liver rich in retinol.
Vitamin A is fat soluble. For Vitamin A to be absorbed a small quantity of fat is required. Some oil or fatty food must be added to the diet daily.
Headache
Headache is a common symptom, the cause of which can be as simple and harmless as a muscle tension headache or as serious and dangerous as haemorrhage or tumour in the brain. In clinical practice psychological ' tension ' headache is seen most frequently.
Pain sensitive structures in the head
Within the cranial cavity the membranes covering the brain, arteries and veins are sensitive to pain. The brain is not sensitive to pain! Pain in the head is felt through the 5th, 9th and 10th cranial nerves. All the layers of the scalp are pain sensitive and headache arising from the muscles or blood vessels are very common.
Diagnostic approach
History
Most information is derived from determining
- The first attack or previous attacks
- Whether onset is acute or gradual (days or weeks)
- Whether attacks have recurred for many years (chronic)
- Site of headache
- Accompanying symptoms
- Precipitating factors
Headache in children
All the causes of adult headache (except retrobulbar neuritis, glaucoma, temporal arteritis and cervical spondylosis) may cause headache in children. In this age group, the most common type of headache is that accompanying any febrile illness or infection of the nasal passages and sinuses.
The complaint of headache by a child should not be taken lightly: the younger the child, the more likely the presence of an underlying organic disease. Fever may not only represent a mild ' constitutional ' upset, but may also result from meningitis, encephalitis, brain abscess or tuberculoma. The presence of neck stiffness and / or impaired conscious level indicates the need for urgent medical care.
Although intracranial tumours are uncommon in children, when they occur they tend to lie in the midline (e.g., medulloblastoma, pineal region tumours). As a result, obstructive hydro-cephalus often develops acutely with headache as a prominent initial symptom.
In a child with unexplained headache, CT scan should be performed
- if the presentation is acute
- if the severity progressively increases
- if the school performance declines or other symptoms such as a sudden change in personality
- if the head circumference increases
- if the child is under 5 years of age
Headache : Specific causes
A. Tension type headache
This is the most common form of headache experienced by 70% of males and 90% of females at some time in their lives.
Characteristics
Diffuse, dull, aching, band-like headache, worse on touching the scalp and aggravated by noise; associated with tension but not with other physical symptoms.
Duration
Many hours - days
Frequency
Infrequent or daily; worse towards the end of the day. May persist over many years.
Mechanism
Muscular, due to persistent contraction, e.g., clenching teeth, head posture, furrowing of brow.
Treatment
Reassurance
Attempt to reduce psychological stress
Anxiolytics
Anti-depressants
B. Migraine
Migraine is a common, often familial disorder characterised by unilateral throbbing headache.
Onset
Childhood or early adult life
Incidence
Affects 5-10% of the population
Female male ratio
The female / male ratio is 2:1
Family history
Positive in 70% of all sufferers
Two recognisable forms exist:
1. Migraine with aura (Classic migraine)
An aura or warning of visual, sensory or motor type followed by headache throbbing, unilateral, worsened by bright light, relieved by sleep, associated with nausea, and occasionally vomiting.
2. Migraine without aura (Common migraine)
The aura is absent. The headache has similar features but it is often poorly localised and its description may merge with that of tension headache.
The aura of migraine may take many forms. The visual forms comprise flashing lights, zig-zags (fortifications), scintillating scotoma and may precede visual field defects. Such auras are of visual (occipital) cortex origin.
The headache is paroxysmal, lasting from 2 to 48 hours and rarely occurring more frequently than twice weekly.
Mechanism
Whether migraine is primarily a vascular or neuronal disorder remains controversial. Chemical neuro transmitters, 5 hydroxytryptamine (5 HT) synonym: serotonin and noradrenaline seem responsible for controlling the diameter of extra-and intracranial blood vessels.
Specific types of migraine with aura
Basilar
It is characterised by bilateral visual symptoms, unsteadiness, dysarthria, vertigo, limb paraesthesia, even quadriparesis. Loss of consciousness may ensue and precede the onset of headache. This form of migraine affects young women.
Hemiplegic
Characterised by an aura of hemoplegia which unusually persists for some days after the headache has subsided. Often misdiagnosed as a stroke. Recovery is the rule.
Ophthalmoplegic: characterised by extraocular nerve palsies, usually the 3rd, rarely the 6th. These may result from dilatation of the internal carotid artery with stretching of the 3rd or 6th cranial nerve within the cavernous sinus.
Precipitating factors in migraine
- Dietary: alcohol, chocolate and cheese (contain tyramine)
- Hormonal: often premenstrual or related to oral contraceptive (fluctuation in oestrogen)
- Stress, physical fatigue, exercise, sleep deprivation and minor head injury
Diagnosis
Clinical history with
- Occasional positive family history
- Travel sickness or migraine variants (abdominal pains) in childhood
- Onset in childhood, adolescence, early adult life or menopause
Differential diagnosis
- Partial (focal) epilepsy (in hemiplegic or hemisensory migraine)
- Aneurysm compressing 3rd cranial nerve
- Transient is chaemic attack (in hemiplegic or hemisensory migraine)
- Arteriovenous malformation- give rise to well-localised but chronic headache
- Hypoglycemia
Management
- Identification and avoidance of precipitating factors
- Prophylaxis: - pizotifen (5HT2 receptor blocker)
- Propranolol (beta adrenergic receptor blocker)
- Methysergide (5 HT 2 receptor blocker)
- Treatment of acute attack
- Simple analgesics (eg. aspirin)
- Sumatriptan (a selective 5HT1 agonist)
- Ergotamine
C. Cluster headache (Histamine cephalogia)
Cluster headaches occur less frequently than migraine, and more often in men than women, with onset in middle age.
Characteristics
Severe unilateral pain around one eye, associated with conjunctival injection, lacrimation, rhinorrhoea and occasionally a transient Horner's syndrome.
Duration
10 minutes to 2 hours
Frequency
Once to many times per day, often wakening from sleep at night. Clusters of attacks separated by weeks or even many months. Alcohol may precipitate the attacks.
Mechanism
Serum histamine levels rise during the attacks, hence ' histamine cephalgia '.
Treatment
Antihistamines give disappointing results. Ergotamine and sumatriptan may give relief. In some cases prednisolone is used.
D. Giant cell (Temporal) arteritis
Giant cell arteritis, an autoimmune disease of unknown cause, presents with headache in the elderly. This is severe and throbbing in nature and overlies the involved blood vessel, usually the superficial temporal artery, although the condition may affect any extra - or intracranial vessel.
Palpation reveals a thickened, tender but non-pulsatile artery.
Neurological symptoms
Strokes, hearing loss, myelopathy and neuropathy may result.
Jaw claudication
Pain when chewing or talking due to ischaemia of the masseter muscles is pathognomomic and occurs in a high proportion of patients.
Visual symptoms are common, with blindness (transient or permanent) or diplopia.
Associated systemic symptoms: weight loss, generalised muscle aches, polymyalgia rheumatica in one-fifth of cases.
Duration
The headache is intractable lasting until treatment is started.
Mechanism
Large and medium-sized arteries undergo intense giant cell formation, with fragmentation of the laminae and narrowing of the lumen, resulting in distal ischaemia as well as stimulating pain sensitive fibres. Occlusion of important end arteries eg. the ophthalmic artery, may result in blindness; occlusion of the basilar artery may cause brain stem or bilateral occipital infarction.
Diagnosis
The ESR is usually high. Blood film shows anaemia or thrombocytosis. C-reactive protein and hepatic alkaline phosphatase are elevated. Biopsy of 1 cm length of temporal artery is often diagnostic.
Treatment
Urgent treatment, prednisolone 60mg daily, prevents visual loss or brain stem stroke, as well as relieving the headache. If complications have already occurred eg. blindness, high dose parenteral steroids are given.
E. Headache from raised intracranial pressure
Characteristics
- Generalised
- Aggravated by bending or coughing
- Worse in the morning on awakening; may awaken the patient from sleep
- The severity of the headache gradually progresses
Associated features
- Vomiting in later stages
- Transient loss of vision (obscuration) with sudden change in posture
- Eventual impairment of conscious level
Management
Further investigations like CT scan, MRI scan of the brain are essential.
F. Headache due to intracranial Haemmorhage
Characteristics
- Instantaneous onset
- Severe pain, spreading over the vertex to the occiput; or described as a " sudden blow to the back of the head "
- Patient may drop to knees or lose consciousness
Associated features
- Usually accompanied by vomiting
- Focal neurological signs suggest a haematoma
Management
Further investigations like CT scan and lumbar puncture are essential.
G. Non-neurological causes of headache
Local causes
Sinuses
Well localised. Worse in morning. Affected by posture, eg. bending. On X ray are sinuses opacified.
Treatment
Decongestants or drainage.
Ocular
Refractive errors may result in muscle contraction headaches; they resolve when corrected with glasses. Glaucoma does not produce headache without other symptoms, e.g., misting of vision, haloes. Cupping is seen on fundoscopy.
Dental disease
Discomfort localised to teeth. Check for malocclusion. Check temporo mandibular joints.
Systemic causes
Headache may accompany any febrile illness or may be the presenting feature of accelerated hypertension or metabolic disorders, e.g., hypoglycaemia, hypercalcaemia.
Many drugs produce headache
- Through vasodilatation e.g., bronchodilators, antihistamines
- On withdrawal e.g., amphetamines, benzo- diazepines, caffeine.
Key points to remember
- Inflammed condition of the eyelids should be treated by hot fomentation.
- In all abnormal conditions of the eye lid corneal damage may occur.
- In corneal ulcers the condition of the sac and diabetic status of patient should be assessed.
- No bandage should be applied in corneal ulcer or conjunctivitis.
- In allergic conjunctivitis and post-operative follow-up cases, patient should be given proper advice if steroids are used, as they can get glaucoma if used long term.
- While dispensing spectacles for refractive errors, the pupillary center and the optical center must be aligned correctly.
- Amblyopia should be identified and treated before 8 years after which there will be not much improvement
- All diabetic retinopathy patients should come for regular follow up.
- Optic neuritis has good visual recovery if treated appropriately with steroids.
- Thyroid ophthalmopathy is the most common cause of proptosis in adults.
- Schiotz tonometry should not be done in active corneal lesions and conjunctivitis.
- Dilating drops should not be applied in shallow anterior chamber and phacomorphic glaucoma.
Choose the correct answer
1.Rolling in of the eye lid is
| a. Trichiasis | b. Entropion |
| c. Ectropion | d. Ptosis |
2. Lacrimal probing is indicated in
| a. Congenital dacryocystitis | b. Acute dacryocystitis |
| c. Chronic dacryocystitis | d. Lacrimal fistula |
3. Ophthalmia Neonatorum is caused by
| a.Toxocara | b. Gonococcus |
| c. Endogenous protein | d.Toxoplasma |
4. Dentrite (branched) appearance is seen in
| a. Fungal ulcer | b. Bacterial ulcer |
| c. Nutritional ulcer | d. Viral corneal ulcer. |
5. Presbyopia commonly occurs at
| a. 30 yrs of age | b. 40 yrs of age |
| c. 50 yrs of age | d. 60 yrs of age |
6. Synechia denotes
| a. Cells | b. Flare |
| c. Keratie precipitates | d. Adhesion |
7. Retinal detachment is common in
| a. Emmetropia | b. Hypermetropia |
| c. Myopia | d. Presbyopia |
8. Ptosis is caused by paralysis of
| a. Optic nerve | b. Occulomotor nerve |
| c. Facial nerve | d. Trochlear nerve |
9. Proptosis is
| a. Dropping of upper lid | b. Forward protrusion of the eye |
| c. Inward displacement of the eye | d. retraction of upper lid |
10. Which is the most common surgical procedure in cataract extraction
| a. Intracapsular | b. Extracapsular |
| c. Phacoemulsification | d. Couching |
11. Which of the following anti-glaucoma medicines constricts pupil?
| a. Timolol | b. Acetazolamide |
| c. Pilocarpine | d. Mannitol |
B. Fill in the blanks
- Cataract is treated by _______.
- 10% KOH wet preparation is done to detect _______ in corneal ulcer.
- The condition of eye with refractive error is known as ________.
- Decrease in visual acuity without any disease in the eye is ________.
- ______ is inflammation of the choroid, ciliary body and iris.
- ________ is the most important ocular manifestation of diabetes.
- Retinal detachment is separation of _______ form the _______ layer.
- Papilledema is swelling of the optic disc due to _______.
- ______ is the most common cause of both unilateral and bilateral proptosis in adults.
Change one or more words to make them true
- Measurement of proptosis is done by tonometry.
- Antibiotics are used in the treatment of optic neuritis.
- Retinoblastoma is benign tumor of the retina.
- Flare in uveitis is due to increased cholesterol content in the aqueous.
- Strabismus amblyopia is difference in refractive power between both eyes.
- Keratoconus is thickening of central part of cornea.
- Ciliary congestion is seen in conjunctivitis.
- For chronic dacryocystitis in younger age DCT is done.
- Inadequate closure of eye lid is called ptosis.
- Acute inflammation of meibomian gland is called chalazion.
Match the following
- External hordeolum - Concave lens
- Vernal Catarrh - Reassurance to patient
- Subconjunctival - Cold compresses hemorrhage
- Myopia - Hot compresses
- Presbyopia - Convex lens
- Squint - Cover test
- Anterior Uveitis - Hard contact lens
- Retinitis pigmentosa - Occlusion Therapy
- Amblyopia - Low vision aids
- Keratoconus - Mydriatics
Find the odd man out
- Entropion, ectropion, ptosis, chalazion
- Pterygium, pinguecula, keratoconus
- Myopia, hypermetropia, presbyopia
- Esotropia, exotropia, amblyopia
- Diabetic retinopathy, hypertensive retinopathy, retinal vein occlusion, retinoblastoma.
Give reasons for the following
- Lagophthalmos in facial nerve palsy.
- Discharge from the eyes in dacryocystitis.
- Foreign body sensation in conjunctivitis.
- Night blindness in retinitis pigmentosa.
- Flashes of the light in retinal detachment.
Answer these Questions
- What is the difference between ciliary congestion and conjunctival congestion?
- What are the 2 things you should not do in a case of corneal ulcer?
- What are the precautions you take in care of conjunctivitis to prevent its spread?
- What are the stages of cataract?
