Visual Acuity
Definition
Acuity of vision is defined as the power of the eye to see a smallest object or letter clearly and distinguishably at specified distances.
Visual acuity is the medical term for sharpness of vision. It deals with the sharpness or discrimination of central vision, rather than the extent or clarity of peripheral vision.
Standard of visual acuity
Vision should be tested with and without glasses on a standard chart.
Each eye should be tested independently. A normal eye can easily distinguish two points separated by an angle of one minute to the eye. This is the standard of normal visual acuity. Perfect acuity of vision requires two other basic factors the light sense and colour sense. The acuity of vision is tested by standard vision chart known as Snellen’s chart.
The Snellen’s chart is used almost universally in testing the acuity of vision. The chart consists of Snellen’s optotypes specially formed letters of the alphabet arranged in rows of decreasing letter size. The size of the letters is standardised so that letters in each row will be clearly legible at a designated distance to a person with normal vision.
Snellen’s chart
Principles of Snellen’s chart
The chart consists of a series of letters of diminishing size as seen in the picture (Fig 3.1). Each letter is of such a shape that it can be enclosed in a square. The size of the square is five times the thickness of lines composing the letter. The square subtends an angle of five minutes at a specified distance.
The Snellen’s chart should be at a distance of six metres or twenty feet. The rays of light from that distance are parallel for practical purposes. Half this distance may also be used, but in that case the test types should be seen reflected through a plain mirror, kept at a distance of three metres or ten feet from the patient. This test could be carried out in a room with a length of three metres and a breadth of minimum one and a half metres. If six and half metres of length is available, the chart could be fastened at eye level on a light, uncluttered wall that has no windows near by. The general illumination of the room should not be less than one - fifth the illumination of the chart.

The chart could be placed above the patient’s head. The patient looks at a mirror hung on the opposite wall. The light from the chart travels to the mirror and then reflects from the mirror to the patient’s eyes, and thus an available room space of 3 metres can be converted optically into one of 6 metres.
The letters are so constructed that the angle of one minute is formed when
- First letter is at 60 metres distance
- Second line is at 36 metres distance
- Third line is at 24 metres distance
- Fourth line is at 18 metres distance
- Fifth line is at 12 metres distance
- Sixth line is at 9 metres distance
- Seventh line is at 6 metres distance
- Eighth line is at 5 metres distance
The right eye is tested conventionally first, except where the patient’s complaint is particularly of defective left eye vision ,in which case the left eye is assessed first. The patient reads down the chart as far as he can and then this is repeated with the other eye. Lastly both eyes are tested together. If the visual acuities of the 2 eyes are about equal it is usually found that they reinforce each other so that the binocular vision is slightly better than the uniocular.
Types of visual acuity
- Distant visual acuity
- Near visual acuity
- Pinhole visual acuity
Distant visual acuity
It is the ability of a person to distinguish an object or letter whose rays are parallel and where no accommodation is required. Various distant visual acuity charts are:
In adults
- Snellen’s chart
- ETDRS chart (Log MAR chart)
In illiterates
- E - chart / pictures chart
- Landolt’s broken rings
chart
- Multiple pictures chart
In children
- Cake decorations
- Teller acuity cards
- Allen Picture
cards
- Sheridan Gardiner testing
- Keeler’s preferential looking tests
-
Cardiff ’s charts
Things needed for the test
- Snellen’s chart with rows of letters
- (for
those who can read)
- E chart (for illiterates)
- Trial set
Trial set consists of
- Trial frame
- Retinoscopy mirror
- Convex
(+) spherical and cylindrical lenses
- Concave (-) spherical and cylindrical lenses
- Pin hole
- Occluder
- Red and green glasses
- Prisms
- Slit and
Maddox Rod
- Cross cylinder
Distant visual acuity testing
This procedure measures the patient’s distant vision by testing their ability to read a character at a standard distance from a specified chart. The size of the letter in each row should be clearly legible at a graded distance to a person with normal vision.
Step by step procedure
Patients who wear glasses or contact lenses may be tested with and without optical correction. Test and record the visual acuity in each eye separately, beginning with the right eye.
- As explained earlier in the chapter, position the patient 6 metres from an illuminated Snellen’s chart
- Have the patient cover the left eye with an occluder or the palm of the hand. Alternatively, you may hold the occluder over the patient’s left eye. With either method, be sure the eye is fully covered and that the occluder is not touching the eye. Observe the patient during the test, to be sure the patient is not peeping around the occluder. This is especially important with children. If they are asked to cover the eye with fingers, patients tend to read through the gaps
- Ask the patients to read the letters from left to right on every other line down the chart until the patient misses more than half the letters on one of the lines. If a tumbling E-chart is being used, ask the patient to indicate the symbols visible on the smallest line by stating the direction or pointing the fingers in the direction which the E points
- Note the smallest point where more than half of the letters are read correctly and record the corresponding acuity (printed at the left of each line on the standard Snellen’s chart) in the patient’s record, as well as the number of letters missed for example 6/9-2
- If the patient is not able to read even the top letter of the Snellen’s drum, you can stand 3 metres away from the patient, and ask the patient to count fingers. If he is not able to do so, go nearer slowly and note, at what distance he is able to count fingers
- If the patient is not able to count fingers less than half metre, slowly wave your hand close to the patient’s face. If the patient recognises it, it should be recorded as visual acuity is HM. If the patient can not even detect the hand movements, light is shown on the face and if the patient is able to say that light is there or not, it is recorded as PL+ (perception of light). If the patient is able to say from which direction the light comes it can be noted as “accurate PR” (projections of rays). If they are unable to say the direction, you note it as “inaccurate PR”. On the contrary, if the patient could not recognise light, it is recorded as NOPL Same procedure is followed for the other eye.
- Record the acuity value for each eye separately, with and without correction
- Pinhole test is conducted if the patient’s visual acuity is less than 6/6 . This test helps the examiner differentiate poor vision caused by refractive errors or due to an eye disease. Generally vision that can be improved with a pin hole can be improved by spectacle lenses
Interpretation of visual acuity
- Visual acuity is recorded as a fraction. The numerator indicating distance in metres at which the patient can read clearly the smallest possible letters/characters in the chart and the denominator indicating the distance in metres at which a normal person can read the same letters /characters in the chart
- The normal visual acuity is 6/6
- If the patient is unable to read 2 letters of the last line it should be indicated as 6/6-2
- If the patient is unable to read last line at 6 metres but reads the previous lines then visual acuity is 6/9
- If the patient is unable to read last two lines but able to read other letters, the visual acuity is 6/12
- If unable to read last three lines then visual acuity is 6/18
- If unable to read last four lines then visual acuity is 6/24
- If they can read only the first 2 lines the visual acuity is 6/36
- If the patient is unable to read even the first line, the visual acuity is less than 6/60
- If the patient is not able to read even the top letter of the Snellen’s drum, he is asked to count fingers, and the visual acuity is recorded as the distance at which he is able to count fingers (CF3 mts or 3/60)
Snellen’s chart is useful and most accurate in literate people above the age of 6 years. For illiterates and children below 6 years of age other test charts based on Snellen’s principles are useful (Fig 3.2). Test of Albini and Landlot’ broken ring test(C) is most useful in age group above 4-6 years and in all illiterate people (Fig. 3.3). The patient is required to show the direction in which the ring or legs of E are seen by them.
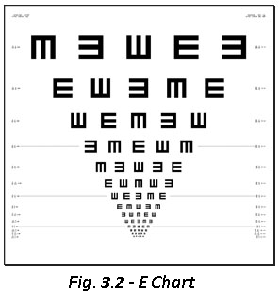
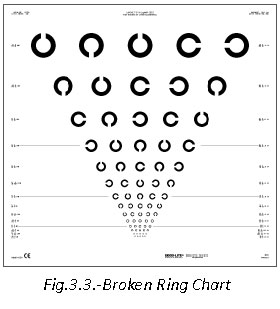
Along with these two tests Beale Collin’s picture test type (which depicts picture of day to day things in a child’s life) or Sjogren’ hand test can be successfully used in small children aged 4-6 years. As in all these tests the size of the symbols suitably corresponds to Snellen’s letters and so the visual acuity is noted in the same manner.
Vision assessment in children
The pre-school vision test or the Allen picture card test consists of seven black and white line drawing of birth day cake, telephone, horseman, teddy bear, automobile, house and tree (Fig. 3.4). These line drawings are drawn on a plastic (10cmx10cm) white cards. The child patient will be shown at a closer distance so that he recognizes and identifies them.
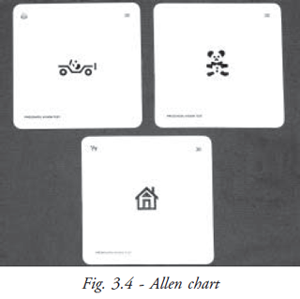
Afterwards with the room fully illuminated these plates are then shown to him from a distance of 6 metres. The distances relate to Snellen’s grading. This test can be successfully used for the age group3 to 4 years.
New York light house flash card test was previously used with children with low vision or amblyopia (Fig 3.5). There are only 3 symbol flash cards with line drawings of open umbrella, an apple and a house. These are printed on separate flash cards. They will be in 7 different sizes from 20/200 to 20/10. The test is done at a fixed distance of 3.60 metres. Fook’s symbol test was familiar geometrical designs as test targets. For example circles, squares, triangles of different sizes drawn on wooden cubes or printed chart formats.

Miniature toy test was previously used with handicapped children and low intelligence patients. It used 2 sets of miniature objects. One set with examiner standing at 10 feet away and the patient is asked to pickup similar objects from his own set. The object chosen are small toy automobile, planes, charts, knives, spoons etc. Sometime the same object like spoons, etc. is in 2-3 size so as to check the grade of vision.
This test can be successfully used in children of age group 2-3 years, but it does not give accurate estimate of visual acuity. In one year old infants who have well developed hand-eye coordination visual acuity can be tested with coins, Block candy test, Ivory ball test, graduated size ball tests etc. The basic principle in the coins or block candy test is simple; the child picks up only those candy beads which he can see easily. Thus when coins or beads of different sizes are shown to him, he picks those he can see. This test gives very approximate estimate of visual acuity for near.
In ivory ball test – 5 ivory balls of ½ inch to one and half inch diameter sizes are rolled and spinned to a distance of 20 feet. The child is expected to fetch the balls which he can easily see. In graduated size ball test the balls are rolled in front of the child and examiner notes the quality of fixation reflexes in relation to the size of balls.
Infant’s relative behavioral response to occluding of one eye gives a significant amount of estimate whether vision is grossly defective in one eye as compared to the other. It is observed how a child responds when their right eye is covered and then their left eye is covered. If the child fusses or becomes more violent in one situation then the other – it means that vision in the seeing eye is defective as compared to other.
Cake Decoration
Small colored sweet balls of 1mm diameter are used to decorate cakes (Fig 3.6).This is used to check the visual acuity of children. Twelve months old children can pick up small objects and eat. Child is shown the cake decoration in examiner’s or mother’s hand and encouraged to pick up and eat them. The test is then repeated with only 1-2 sweet sugar balls after covering either eye alternatively. Ability to see the sweet indicates the vision of 6/24 at the testing distance.
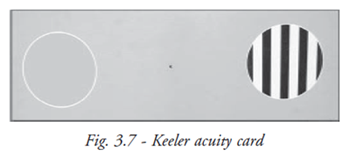
Keeler acuity test (preferential looking)
This test is based on the principle that a child prefers to look at pattern and not plane surface (Fig. 3.7). The child sits comfortably on the mother’s lap. The child is shown a coarse grating card at 38cm. The examiner looking through a peep hole, make the decision as to whether the child is looking at the grating. The finest grating that the child prefers to look is taken as acuity limit.
Cardiff Visual Acuity Test (vanishing optotype)
The cards have six shapes which are easily recognisable (house, fish, dog, duck, train) positioned either at the top or bottom half of a card (Fig 3.8). The cards are caliberated to give visual acuity of equivalent of 20/20 to 20/200 at 1 metre viewing distance. When the child is comfortably seated the cards are presented at eye level at a distance of 1 metre. The examiner watches the eye movements towards the shape. If the child is looking at the shape, then the next card is presented. This procedure is continued until no definite fixation is observed. The test is performed at 1metre distance but altered to ½ metre if the child is unable to see the first card.

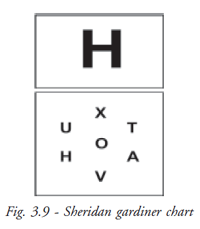
Sheridan gardiner test (matching test)
This test uses letters which children can recognize and copy at an early age. The letters V T O H X A U are used and are shown to the child one at a time on flip card (Fig. 3.9). The child is given a key card showing all the letters and he has to point the letter he sees. After explaining the procedure to the child the test can be done at 6 metres or 3 metres. Sheriden Gardiner test is the most accurate of the illiterate vision test in children.
Basic torch examination
After examination of visual acuity it is important to do a general torch examination to record and note position of the orbit, eye balls, relative position of ocular structure, and any gross abnormality in these should be noted. With closer attention the following points are recorded.
- Position and size of eye balls and orbital socket
- Position of eye lids, shape, size, contour, margins, palpebral fissure and eye lashes
- Position of the puncta in upper and lower lid near nasal canthi of both eyes
- Position and texture of conjunctiva, presence of abnormal redness, discharge at canthii, follicles and papillae especially on the palpebral conjunctiva
- Surface and texture of cornea, its shape, size, presence of surface opacities and irregularities, etc
- Depth of anterior chamber, floaters in aqueous (if any)
- Iris – position, colour, pattern, texture
- Pupils position, shape and pupillary reflex - direct and consensual
- Reflex from lens in pupillary area, presence of any opacity in pupillary area
Testing methods of near visual acuity
It is the power of the eye to clearly see and distinguish smallest object or letters from a normal readign distance. For practical considerations the normal reading distance is considered to be 40 cms.
When the distance vision has been tested, the visual acuity at reading distance is investigated. Snellen’s constructed a set of letters of graded sizes and thicknesses on the same principles as his distant types, and this is the most scientifically accurate test. In this type the letters in the 6/6 line subtends an angle of 5 minutes at an average reading distance. This may be called the “Snellen’s equivalent’’ for near vision. Such a test however has never become popular and graded sizes of letters of pleasing types have been habitually employed. The first test of this kind was suggested by Jaeger in 1867. The Jaeger card has print samples of different sizes. The card is held at 32 cms. The results of visual acuity tests are used to prescribe eye glasses or other corrective measures.
How to perform the near acuity test?
Patients who wear glasses or contact lenses should wear them for the test. The near vision should be checked with and without glasses.
- Instruct the patient to be seated ,/li.
- After the patient is comfortably seated, printed test card is given to them
- Ask the patient to hold the test card at the distance specified on the card, usually 40 cms
- Have the patient cover the left eye with an occluder or the palm of the hand
- Ask the patient to read with the right eye the line of the smallest characters legible on the card
- Repeat the same procedure with the other eye occluded
- Record the near acuity value for each eye separately
Pinhole visual acuity
The pinhole disc is a small circular disc with a small central opening that reduces the peripheral rays and allows the central rays to reach the retina. This opaque disc has 1.2mm hole in the middle. A 0.55 mm hole actually reduces visual acuity due to diffraction. 1.32mm pinhole is the best. The standard trial pin hole is 1mm in size.
The pinhole permits the most central rays to enter and provide a good image, just as the pinhole camera gives a fine image without a lens system. The pin hole serves to differentiate visual loss caused by refractive errors from poor vision resulting from disease of the eye. In the latter condition vision will not improve when a pinhole disk is placed before the eye.
Colour Vision
The colour of any object is determined by the wave length emitted or reflected from the surface. White light is a mixture of wavelength of the visible spectrum. Colour is perceived by three populations of cone photoreceptors in the retina which are sensitive to light of short (blue), middle (green), or long (red) wave length.
A congenital colour vision defect occurs if a cone pigment is absent or if there is a shift in its spectral sensitivity. Hence, deuternopia, protonopia, and tritenopia indicate absence of green, red and blue cone function, and deuteranomaly, protonomaly and trianomaly indicate a shift in the corresponding cone sensitivity. The X chromosome carries the blue pigment gene. 8% of men and 0.5% women have a defect of the red / green system; the most common is deuternomaly which occur in 5% of men and 0.3% of women. Triton defects are rare.
Congenital color defects characteristically affect particular parts of the colour spectrum. Acquired colour defects occur through out the spectrum but may be more pronounced in some regions.
For example, acquired optic nerve disease tends to cause red- green defects. An exception occurs in glaucoma and in autosomal dominant optic neuropathy which initially causes predominantly blue- yellow deficit; it has recently been found that visual field loss in glaucoma is detected easier if perimetry is performed using a blue light stimulus on a yellow back ground. Acquired retinal disease tends to cause blue yellow defects. Clinical tests of colour vision are designed to be performed in illumination equivalent to afternoon daylight in the northern hemisphere.
The following tests are done to detect colour vision defects and they are;
- Fransworth Munsell (FM) 100 hue test
- D-15 test
- Ishihara pseudo isochromatic test plates specific test for congenital red-green defects
Colour vision tests
The impaired ability to perceive colour is most commonly an inherited condition, passed from the mother to a male child. Optic nerve or retinal disease may also cause defects in colour vision. For the majority of patients with impaired colour vision, the colour red appears less bright than for normal individuals, preventing accurate perception of colour mixtures that include red. While a deficit in colour vision is not usually disabling, it can hinder individuals from pursuing certain specialised careers.
Evaluation of color vision is often performed with pseudo isochromatic colour plates. (Insert the picture) Each eye is tested separately. Patients are instructed to look at a book of these plates, which display patterns of colored and grey dots .Patients with normal colour vision can easily detect numbers and figures composed of and embedded in, the multicolored dots. Patients with colour vision deficits cannot distinguish the numbers and the figures. Various combinations of colors are used to identify the nature of the colour vision deficit. The 15-hue test, or Farnsworth-Munsell 100 hue test, provides a more precise determination of colour vision deficits. The test consists of 15 pastel-colored chips of similar brightness but subtly different hues, which the patient must arrange in a related colour sequence. The sequence is obvious to patients with normal vision, but patients with colour deficiencies make characteristic errors in arranging the chips.
Attitude
- Explain to the patient what you are going to do and how they can co-operate for the visual acuity test
- In cases, like injury / infection / redness / corneal ulcer, check the patient carefully and try to send them as early as possible, to the doctor
- Special attention should be given to children and patient with mental depression, while assessing visual acuity
- Listen carefully to the patient while they speak out their health problems and treat them with patience and compassion in case they do not cooperate
Summary
In this unit the OA has learned the different types of charts used to test the visual acuity of all age groups. It is given in detail the procedure to be followed and how the readings or findings are to be recorded.
Key points to remember
- Wash your hands thoroughly after testing any infected patient
- Occluder is a hand held paddle used to cover one eye during a test
- Visual acuity test should be performed with a bright illuminated chart
- Pinhole paddle; a hand-held paddle with small viewing holes, used to determine whether spectacle lenses are likely to improve vision.
- Projector; required if a projected image of the test chart is to be used.
- Mirror; required to obtain the correct optical distance between the patient and the chart when the physical distance is too short.
- Snellen’s chart is for those who know the alphabet or numbers.
- The tumbling E chart is for the illiterate patients
- Charts with silhouetted pictures to identify - Allen chart
- Letter matching tests (20 to 10 feet) – the children need not know the letter but they need only to match whatever letter you point to.
- Teller acuity cards - with vertical black and white stripes (gratings) to test the visual acuity of infants and preverbal toddlers (the examiner watches for a shift in gaze through a pinhole in the card)
Common abbreviations for visual acuity measurement
| V,VA | - Visual acuity | |
| OD | - Oculus dexter (right eye) | |
| OS | - Oculus sinister (left eye) | |
| CC | - Cum correction, with correction (eye glasses or contact lenses | |
| SC | - Sine correction, without correction (eye glasses or contact lenses) | |
| Ph | - Pinhole | |
| HM | - Hand motion | |
| PR | - Projection of rays | |
| PL | - Perception of light | |
| FCF | - Finger counting close to face | |
| NOLP | - No light perception |
Student exercise
Answer the following
- What is visual acuity?
- What is the principle of the Snellen’s chart?
- List the types of distance acuity charts?
- List the various charts used for paediatric vision assessment?
- Define color vision?
- List the types of test done to detect defects in color vision?