Ocular Motility and Strabismus
Introduction
Squint is misalignment of the eyes where the two eyes are pointed in different directions. It is manifest if it is visible and latent if it is controlled and not visible. Manifest squint again can be either present all the time (constant) or occasionally (intermittent). A manifest squint is otherwise termed heterotropia. The importance of detecting and treating squint as early in life as possible is to avoid irrecoverable vision loss due to a condition called amblyopia which has been described.
Extra ocular muscles and extra ocular movements
There are fourteen extra ocular muscles, six inserted into each globe and responsible for movement of the eyes, and one inserted into each upper eyelid, responsible for raising it.
These muscles are:
|
1. Rectus muscles |
|
|
Horizontal recti |
Lateral rectus |
|
Medial rectus |
|
|
Vertical recti |
Superior rectus |
|
Inferior rectus |
|
|
2. Oblique muscles |
Superior oblique |
|
Inferior oblique |
|
|
3. Lid elevator muscle |
Levator Palpebrae |
|
Superioris |
Nerve supply
The extra ocular muscles are supplied by the cranial nerves as follows: the sixth nerve supplies the lateral rectus, the fourth nerve supplies the superior oblique, the superior division of the third nerve supplies the medial rectus, the superior rectus and the levator muscle and the inferior division of the third nerve supplies the inferior rectus and inferior oblique.
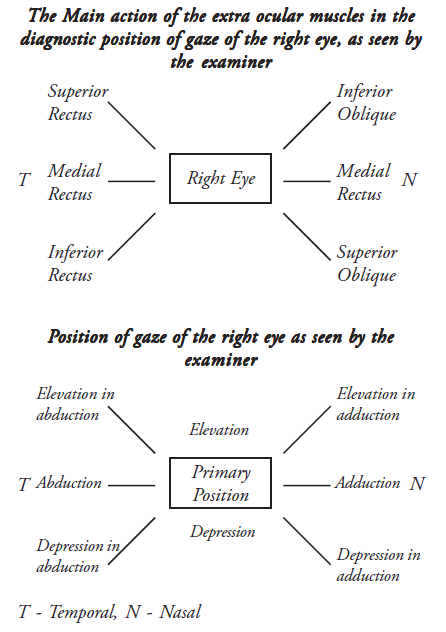
Actions of the extraocular muscles
Movement of the globe is brought about by relaxation and contraction of the extraocular muscles. Each muscle has a main action in one position of gaze which is termed the diagnostic position of gaze and also one or more secondary actions. When the eyes look straight ahead, they are in the primary position. As the eyes move away from the primary position, one or more muscles increase their contraction and others relax to allow movement to take place. The following two figures will show the direction of movement brought about by the various extra ocular muscles.
The main and secondary actions are shown in the table below
| Muscle | Main Action | Secondary Action |
|---|---|---|
|
Latera Rectus |
Abduction |
None |
|
Medial Rectus |
Adduction |
None |
|
Superior Rectus |
Elevation and abduction |
Adduction and intorsion |
|
Inferior Rectus |
Depression and abduction |
Adduction and extorsion |
|
Superior Oblique |
Depression and abduction |
Abduction and intorsion |
|
Inferior Oblique |
Elevation and abduction |
Abduction and extorsion |
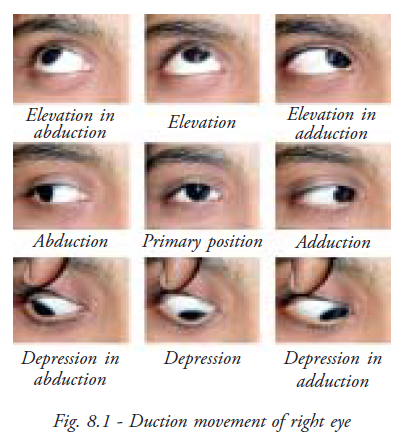
Duction
Duction is a movement of one eye, Abduction being outward movement, Adduction the inward movement (Fig. 8.1).
Supraduction and Infraduction apply to upward and downward movement respectively, but these latter terms are rarely used.
Versions
A version is a conjugate or parallel eye movement in which both eyes move in the same direction (Fig.8.2).
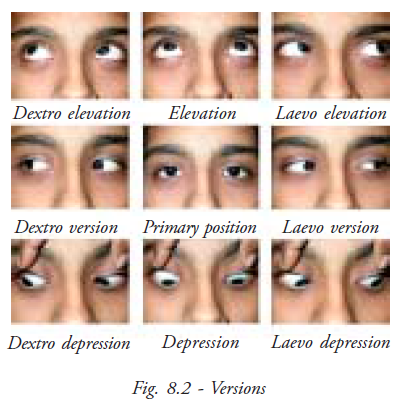
Versions are described as
- Dextroversion, both eyes move to the right
- Laevoversion, both eyes move to the left
- Dextroelevation, both eyes move up and to the right
- Dextrodepression, both eyes move down to the right
- Laevoelevation, both eyes move up and to the left
- Laevodepression, both eyes move down to the left
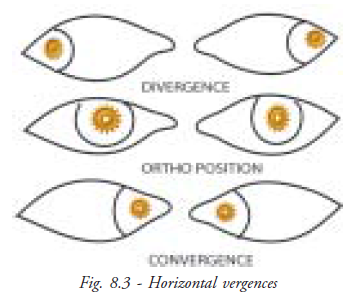
Vergences
A vergence is a disconjugate or non-parallel eye movement in which the eyes move in opposite directions (Fig. 8.3). They comprise;
- Convergence, brought about by contraction of both medial rectus muscles
- Divergence, brought about by contraction of both lateral rectus muscles
Examination of ocular movement
Versions are tested routinely by asking the patient to follow a moving target into the diagnostic positions of gaze, observing the extent of movement of each eye. It is usual to test horizontal movement first, followed by vertical movement and oblique movements.
Procedure
- The patient's head must be kept straight. It may be necessary to hold it, especially when testing a child
- The target must be easy to see and small enough to ensure accurate fixation on it. A small pen torch is ideal, but must not be too bright
- The target should be held about 40 cm from the patient's eyes and should be kept at eye level when testing horizontal versions
- Both eyes must be visible to the examiner. It may be necessary to raise the eyelids slightly to see the eyes as they look down, but the eyelid
- Position must be observed before doing this, because abnormal lid movements are sometimes seen and must be noted
- The target should be moved smoothly at a moderate speed, not too fast for the patient to follow it. It must be moved to the extreme limits of gaze, otherwise small defects of movement can be missed
Results
If both eyes move equally and smoothly in all directions of gaze, to the extreme positions, the ocular movement is said to be “full”.
- Underaction means a limitation of movement seen when the eye is directed into the diagnostic position of gaze
- Overaction means excessive movement of a muscle beyond its extreme limits in the diagnostic position of gaze
- Detection of slight underaction is easier if the movement of the suspected eye is compared with the same movement in the normal eye. For example, if the right eye is the suspected eye then comparing abduction of right eye with that of left eye will bring out even a small underaction of abduction in the right eye
Recording the results
The amount of limitation of movement is classified as slight, moderate, marked or no movement. This is documented with 1 to 4 (-) signs respectively.
Over action which again can be mild, moderate, marked or severe is documented with 1 to 4 (+) sign respectively.
Binocular Vision
Binocular single vision
Binocular single vision (BSV) is the simultaneous use of the two eyes to give a single mental impression in ordinary seeing conditions. The images of the fixation object from each eye fall on the foveas and are fused to give a combined single image.
Components of binocular vision
Simultaneous perception is the ability to see the images projected from each eye at the same
time.
Fusion is the ability to join two like images, one from each eye, and see them
as one fused image.
Stereoscopic vision is the ability to appreciate that the fused image is
three-dimensional.
Patients with manifest squint may have simultaneous perception but lack the
ability to fuse.
Fusion amplitude or fusion range
The fusion amplitude is the measure of the amount of vergence movement which can be maintained. The positive fusion amplitude represents convergence and the negative fusion amplitude represents divergence.
Stereoscopic vision
Stereopsis is the appreciation of depth. True stereopsis is obtained only when BSV is present
Convergence and accommodation
Convergence
Convergence is a disconjugate movement in which both eyes rotate inward so that the lines of sight intersect in front of the eyes. It allows bifoveal single vision to be maintained at any fixation distance.
Convergence is well developed by 2-3 months of age. It is made up of four parts:
Tonic convergence: When a person is deeply asleep or unconscious, the eyes are normally divergent. This is called the position of rest. Tonic convergence brings the eyes from the position of rest to a straight position.
Proximal convergence: It is the response to the individual's knowledge of the nearness of the object.
Fusional convergence: It is induced by the desire for binocular single vision. It is responsible for maintaining BSV when heterophoria is present.
Accommodative convergence: It occurs in response to accommodation. This is the largest component of convergence. Even when accommodation is prevented by old age, accommodative convergence still occurs in response to the stimulus of blurred vision.
Near point of convergence
This is the point closest to the eyes at which convergence can be maintained. It is measured in centimeters (cm) from the corneal surface, most conveniently by apparatus such as the near point rule or RAF ruler. The normal near point is 8 cm.
Accommodation
Accommodation is the ability of the lens to adjust its convexity to the distance of the fixation object from the eyes, so that the image is sharply focussed.
Near point of accommodation
This is the point closest to the eyes at which clear vision can be obtained. It is measured in cm from the corneal surface, with each eye separately and with both eyes together. The near point ruler or RAF ruler can be used for this measurement. The normal near point depends on the age of the person tested.
Amplitude of accommodation
This is the total amount of accommodation which can be exerted, expressed in diopters (D). Like the near point, the amplitude depends on the person's age. Accommodation develops in early childhood and is reasonably accurate at 2-3 months when convergence develops. In normal subjects the amplitude is 16D at 16 years, it reduces to 8D at 32 years and at 60 years only one diopter remains.
Classification of squint
Tropia is manifest squint which can be broadly classified as
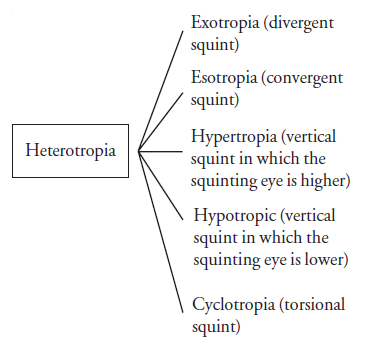
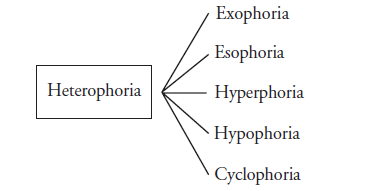
A latent squint is a phoria. Heterophoria includes all types of latent squint.
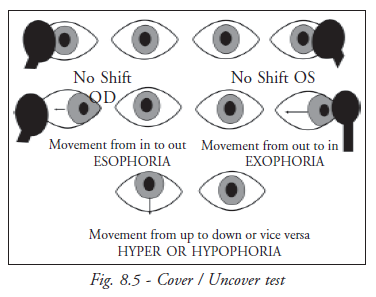
While doing the cover test the eye takes fixation from an outside position towards the nose. This is called exotropia. If the eye moves from an inward position towards the ear to take up fixation it is esotropia. Up to down means hyper and down to up means hypo.
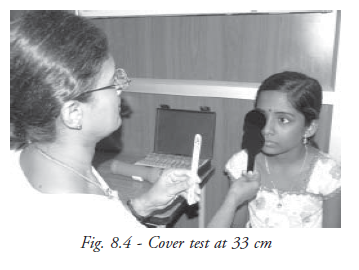
Cover test
The cover test is the main method of detecting manifest and latent squint. It can be done for near (33cms) and distance (6metres) (Fig. 8.4).
It requires:
- An adequate means of completely covering the eye. The best cover is a paddle type occluder
which can be moved easily from one eye to the other
- Alternatively a card may be used
- Fixation targets for near and far fixation
- A vision chart for distance fixation
Method
The cover test is used in two ways, the cover/uncover test and the alternate cover test. Both are necessary and are usually performed in that order
Cover/uncover test
The patient fixes on a spotlight held centrally just below eye level at 33cm (Fig. 8.5). The corneal reflections are noted and compared. The reflection on the squinting eye will be displaced, nasally in exotropia and temporally in esotropia.
In manifest squint / cover test
One eye, for example the right eye is covered, and the behavior of the left eye is observed. The cover is then removed, still watching the left eye. If there is a manifest squint in the left eye, that eye will move to fixate when the right eye is covered. When the cover is removed it will return to its squinting position, unless the patient is able to alternate, when it may remain fixing while the right eye squints. The test must be repeated in all gazes. The examiner must be sure that the patient is fixing on the light. The test is repeated using a target at 6m.
In latent squint / cover / uncover test
One eye is covered and then uncovered as described above, but the behavior of the eye behind
the cover is observed as the cover is taken away. In heterophoria the eye behind the cover
deviates and then straightens as the cover is removed. This is done for each eye . The test
is performed at 33cm and 6m, comparing the amount of deviation seen and noting particularly
the recovery movement to regain BSV. This may be
- Rapid, when the eye straightens immediately after the cover is lifted
- Moderately rapid, when the eye starts to straighten immediately but moves less quickly
- Slow delayed, when the eye remains in a squinting position for a short time before
starting to straighten
The importance of the speed of recovery is that it is a guide to the patient’s ability to keep the heterophoria under control. A rapid recovery indicates good control whereas a slow or delayed recovery suggests that the heterophoria could cause symptoms or could become a manifest squint.
Alternate cover test
In this test the cover is changed from one eye to the other back and forth several times (Fig. 8.6). One or the other eye is covered throughout the test. The direction and amount of movement of each eye is noted as the cover changes.

Because the patient never sees the target with both eyes at the same time, a recovery movement cannot occur, therefore this method cannot differentiate manifest and latent squint. Its purpose is to dissociate the eyes by preventing binocular vision in order to find the maximum angle of squint.
Precautions
- The examiner must give the patient time to fix steadily before removing the cover or changing it to the other eye
- The eye must be covered long enough to allow dissociation to take place and uncovered long enough to allow for possible recovery. If it is performed too quickly the correct diagnosis may be missed
Information obtained from the cover test
- The presence of a squint
- Whether it is manifest or latent
Manifest squint
- The type: exotropia , esotropia or vertical squint
- Whether it is constant or intermittent, unilateral or alternating
Latent squint
- The type of phoria
- The distance at which the phoria increases, for example, an exophoria may be larger for near than distance or larger for distance than near
- The degree of compensation, detected from the speed of the recovery movement
Measurement of the angle of squint (Tropia )
Methods using corneal reflections
Hirschberg
This test is a method of estimating the angle of manifest squint from the position of the corneal reflections in the squinting eye (Fig. 8.7). It is assessed at 33cm. The patient fixes on a light held centrally at eye level at this distance and the corneal reflections are noted in both eyes. The reflection in the fixing eye will be central or slightly nasal in the large majority of cases. The reflection in the squinting eye will be displaced nasally in exotropia and temporally in esotropia. Each mm of displacement from the center of the cornea equals approximately 15 diopters of squint. The angle of squint is calculated by assessing the number of mms.
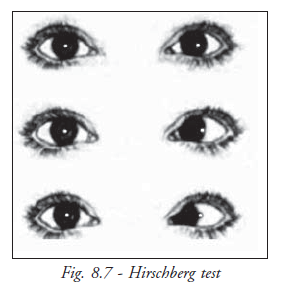
If for example, the reflection is midway between the center of the pupil and the limbus (the junction of the cornea and the sclera), the angle is approximately 40D (20). If it is at the limbus, the angle is 90D (45). This method is useful when the angle cannot be measured by prism cover test, usually when the angle is very large or the patient cannot cooperate.
Methods of measuring the angle of squint using neutralisation of movement
Prism Cover Test
The prism cover test is the first choice method of measuring manifest and latent squint using loose prisms or prism bars) (Fig. 8.8).
It requires:
- Prisms, usually in the form of horizontal and vertical prism bars. Loose prisms can also
be used
A cover test is first performed to find
- The type and direction of squint
- The fixing eye in manifest squint
- Fixation in the squinting eye
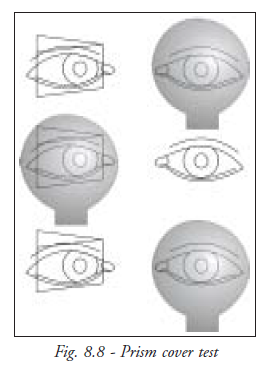
Method
The patient fixes on an easily seen picture or letter at 33cm (Fig. 8.9). The prism bar is placed in front of the squinting eye in manifest squint or in front of either eye in latent squint. The apex of the prism is placed in the direction of the squint, base in for exodeviations, base out for esodeviations and base down in hypertropia. An alternate cover test is performed, slowly enough to give the patient time to fix through the prism, watching the movement of each eye as the cover is changed. The prism strength is adjusted until there is no movement, giving the measurement of the angle in prism diopters. The procedure is repeated using a distant target.
The prism cover test is recorded as, for example:
|
PCT |
near 45D base out with glasses or 45D ET with glasses |
|
distance 35D base out with glasses or 35D ET with glasses |
Examiner’s precautions
- Loose prisms are easier to interpret than a prism bar. The prism must be held upright with the back surface parallel to the plane of the face
- Prism must be kept straight. If it is tilted to one side the prism strength is changed
- The patient must look through the center of each prism
- The alternate cover test should be performed fairly slowly to give the patient time to fix on the target
- One or the other eye must be covered all the times to dissociate the eyes and to prevent binocular vision
Measurement of angle of squint (phoria)
Maddox wing
The maddox wing is used to measure heterophoria at 33cm (Fig. 8.10). The patient looks through two eye pieces at a metal plate at the base of the instrument. The plate is marked with two scales, one horizontal and the other vertical, both marked in prism diopters.
A vertical white arrow points to the horizontal numbers and is used to measure horizontal phoria. Horizontal red arrow points to the vertical numbers and is used to measure vertical phoria. This arrow should be seen parallel to the horizontal numbers. If it is tilted cyclophoria is present. The arrow can be straightened by moving it up or down against a small vertical scale on the right side of the metal plate. The scale is marked in degrees to measure the amount of cyclophoria.
The right eye sees the horizontal and vertical scale and the left eye sees the vertical arrow pointing to the horizontal scale and a horizontal arrow pointing to the vertical scale. The eyes are therefore dissociated and any latent squint becomes manifest in order to measure the full deviation.
Precautions
Time must be allowed for full dissociation to take place.
The patient should wear glasses if they usually wear them for reading. It
is sometimes easier to place lenses in the slots provided in the instrument’s eye
pieces, especially if bifocal spectacles are worn.
Maddox rod
The Maddox rod is a subjective method of measuring latent and some manifest squint. It is usually coloured red and consists of a number of parallel ridges which act as cylinders, converting a point source of light, a small spotlight, into a line image at 90 to the axis of the cylinders. The patient fixes on the spotlight with one eye and sees the line with the other eye. Fusion is impossible because the images are dissimilar, the eyes are therefore dissociated. The angle of squint is measured by using prisms to move the line until it passes through the light. The Maddox rod is generally used at 6m but can be used at other distances.
Method
- To measure horizontal phoria
The rod is placed in a pair of trial frames with the ridges horizontal, giving a
vertical red line. The patient fixes on a spotlight at eye level and is asked where they
see the line. In esophoria, it will be on the same side as the rod, in exophoria it will
be on the opposite side. A prism bar is placed in front of the rod, base out for
esophoria and base in for exophoria, and the prism bar is moved increasing the strength
of prism slowly until the patient sees the line passing through the light
- To measure vertical phoria
The ridges are placed vertically in the trial
frames to give a horizontal line. The deviation is measured using a base down prism in
front of the rod to measure hyperphoria or base up to measure hypophoria.
Methods of measurement of convergence, accommodation and fusion amplitude
Near point rule (Royal air force ruler)
The near point rule (NPR) provides a convenient method of measuring convergence and accommodation (Fig. 8.11). It consists of a square metal rod 60 cm long with a face rest attached to one end. The top surface of the rod is marked out in cm to measure the distance from the patient’s eyes.
The amount of accommodation in diopters (D) and an indication of the accommodation normally available at different age ranges are shown on the other slides. Targets for testing convergence and accommodation are mounted on each side of a sliding carrier which is moved along the rod. The targets consist of a vertical black line with a central fixation dot, used to measure convergence, and near test type and reduced Snellen’s letters used to measure accommodation.
Method
The patient should be positioned with the selected target in a good light and with their eyes visible to the examiner. It is advisable to test convergence using a pencil or similar target before starting the test. Their near vision should also be known.
To measure convergence
- Objectively (i.e. according to the examiner’s observations) the slide carrier is moved along the rod starting at a distance judged to be within the patient’s convergence range, e.g. 20-25cm. The patient is told to fix steadily on the central dot on the line and the carrier is moved slowly towards his eyes. The observer notes:
The near point of convergence (NPC), which is the distance at which one eye is seen to diverge. The test is repeated two or three times, noting if the NPC remains the same, improves or deteriorates. The diverging eye should be noted.
- Subjectively (i. e. according to the patient’s observations)
The patient is asked to say when he notices the line become double or when he sees it move to one or the other side. This happens when the image is suppressed; the line moves to the side of the dominant eye. The subjective measurement is a more sensitive measurement; provided the patient is cooperative, he will notice movement of the line before the examiner sees movement of the diverging eye. The NPC may therefore be farther away when tested in this way: for example, NPC objectively 10cm, NPC subjectively 12cm.
It is usual to measure convergence objectively first and then make use of the patient’s observations( subjective) on retesting. The normal NPC is 10cm or better; it should be easily maintained at this distance.
Recording convergence
|
Examples: |
NPC 8cm, easily maintained |
|
NPC 12cm with effort, LE diverges with L. suppression |
|
|
NPC 12cm, RE diverges with diplopia; can rejoin with effort. |
To measure accommodation
The aim is to measure the near point of accommodation (NPA) and compare it with the normal for the patient’s age. The NPA is the closest distance at which clear vision is possible.
Accommodation can be measured with each eye separately and binocularly (when binocular single vision is present and convergence is sufficiently good). For this reason convergence should always be tested before measuring accommodation. The measurement is made with glasses if these are normally worn for close work.
Uniocular measurement
One eye is occluded and the patient is asked to read the smallest print they can see clearly. The type is moved slowly towards them until they notice that the print has started to become blurred. The test is repeated several times to assess if the NPA remains the same or deteriorates on repeated testing. The other eye is occluded and the test repeated, preferably using a different near test type.
Binocular measurement
The method is as described for uniocular measurement but with both eyes open.
Results
The NPA is recorded in centimetres uniocularly and binocularly if applicable. Usually the measurement is approximately the same uniocularly and binocularly. If the uniocular measurements are significantly better than the binocular measurement, it is probable that blurring with both eyes open is due to failure of convergence rather than failure of accommodation: The uniocular measurements are then taken into consideration rather than the binocular measurements. The normal NPA depends on the patient’s age.
Precautions
The centimetre scale refers to the distance from the patients eyes: it is read from the
back limit of the carrier and not from the actual target distance.
Testing accommodation is purely subjective.
Fusion amplitude (fusion range)
Convergence, divergence and vertical vergence can be measured with prisms, most easily
with the horizontal and vertical prism bars. Convergence is measured with base out
prisms, and is the positive fusion amplitude. It forms the greater part of the total
horizontal fusion amplitude. Divergence is measured with base in prisms and is the
negative fusion amplitude. Vertical vergence is measured using a vertical prism bar.
The fusion amplitude is usually measured at 33cm but should also be
measured at 6m when indicated.
To measure the positive amplitude
The prism bar is placed base out in front of one eye. The patient fixes on a target held
centrally, just below eye level at 33cm. An accommodative target, such as a picture or
Snellen’s letter, or, preferable, a light is used. The observer watches the patient’s
eyes as the prism strength is slowly increased. The eye behind the prism should converge
and the other eye should remain fixed on the target. The bar should be moved slowly
enough for convergence to take place, ensuring that the patient is looking through the
center of each prism. The patient is asked to say when the target becomes double. The
observer notes when one eye diverges. If diplopia is present the patient should be
encouraged to fuse the images, as the prism is increased. It is sometimes helpful to
move the target closer to their eyes to stimulate accommodation, which may be followed
by convergence; the target can then be returned to 33cm and the prism strength increased
until convergence can no longer be obtained.
Sometimes convergence fails because the patient does not understand
what the patient has to do; it should be explained to them that they have to converge
their eyes, just as they would if the target was moving towards them.
To measure the negative amplitude
The base in prism bar is placed in front of one eye. The eye behind the prism should move out and the other eye should remain fixed on the target as the prism strength is slowly increased. The observer should see one or the other eye move in when the limit of the negative amplitude is reached. The patient will probably see double when binocular single vision can no longer be maintained.
To measure the vertical amplitude
The vertical amplitude is measured only when hyperphoria is present. A vertical prism bar is placed base down in front of one eye. The prism strength is slowly increased until binocular single vision can no longer be maintained. The prism bar is then reversed so that the prism is base up and the process is repeated. The eye behind the prism will move in the direction of the prism apex in order to maintain binocular single vision, but the amount of movement is small and can be difficult to see. The patient should be asked to say when they see double and can no longer fuse the images.
Precautions
The patient must have binocular single vision in order to measure the fusion amplitude
with prisms
They should be encouraged to rejoin the images when diplopia occurs and should be
allowed time to do so
The normal fusion amplitudes for near and distance in prism diopters are shown in the
table
|
Convergence |
Divergence |
Vertical vergence |
||
|
Near |
Dist |
Near |
Dist |
Total |
|
35/40 |
15 |
15 |
5/7 |
6 |
Investigation of binocular vision
Worth’s lights (Worth’s 4- dot test)
This test consists of four round lights, one red, two green and one white, as shown in Fig. 8.12 which are viewed through red and green glasses or goggles. The colours are complementary, so that the red and white lights are seen through the red glasses and the green and white lights through the green glasses. Only white lights are visible to both eyes simultaneously. The test is designed for use at 6m; scaled down lights are available for use at 50 cm and at 33cm. The test is done to obtain information about binocular vision. If the red light is infront of the right eye, the possible responses are:
- 4 lights, indicating binocular single vision, which can be normal
- 2 red lights, indicating left suppression
- 3 green lights indicating right eye suppression (as in the diagram)
- 5 lights, 2 red and 3 green, indicating a manifest squint without suppression. Normal retinal correspondence is likely
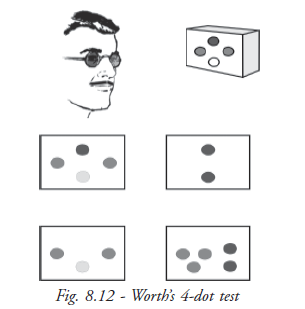
Method
- The patient should view the lights at eye level. The red and green glasses should be in
place before the lights are shown. The patient is asked how many lights they see, then
questioned about the colours of the lights. The results are recorded as, for example,
Worth’s 4dot
Worth’s 3 (R. suppression)
Worth’s 5 (uncrossed/crossed) - Further information about binocular vision can be obtained if 5 lights are seen. If for example there is an esotropia and the patient has uncrossed diplopia of the lights, a base out prism can be used, preferably in the form of a prism bar, to find out if fusion of the lights is possible. The prism strength is adjusted to move the lights together. A patient with fusion should see 4 lights. The prism can be increased or decreased by 2 or 3 diopters and the lights should stay fused. If the patient has no fusion, he will see 5 lights, changing from uncrossed to crossed as the prism strength is increased. This information is important when planning treatment for squint
Precautions
- The patient, especially a child, should not be allowed to see the lights until they are wearing the glasses. If they know that there are four they may say that is what they see
- If the patient claims to see 4 or 5 lights, the examiner must make sure that all are lighted up. Occasionally it is possible to see lighted dots as black shapes
- If the patient sees 5 lights they should be asked if they see them all at the same time. Occasionally patients with alternating squint see 2 or 3 lights rapidly interchanging and will say they see 5
- BSV can also be tested with other instruments like Synoptophore and Bagolini striated glasses etc
Tests to measure stereoacuity
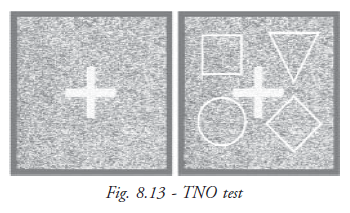
TNO test
Method
The test is done at 40cm. The patient wears the red and green glasses, on top of their own spectacles. They are shown the first plate, containing a butterfly in a field of random dots and asked how many butterflies they see. They should be asked to point to them to make sure they see the “hidden “butterfly. If they are correct, they can progress through the following plates until they are no longer able to see the stereoscopic target. The range of disparity is 480 to 15 seconds of arc. The result should be recorded as the smallest disparity the patient can see, for example “TNO 30’ ” (Fig. 8.13).
Convergence deficiency, accommodative deficiency and heterophoria and their treatment
Convergence deficiency and insufficiency signs
- Headaches, usually in the frontal area, and eye strain, caused by the effort needed to converge
- Blurred vision and intermittent diplopia for near, caused by failure of convergence
Diagnosis
Convergence deficiency is diagnosed:
- From the patient’s history of symptoms associated with close work
- By measuring the near point of convergence, easiest using a near point rule, repeating the measurement several times to see if the near point remains the same or if it moves further from the eyes on repeated testing
- The near point of accommodation, which can also be measured on the near point rule. The near point is the distance closest to the eyes at which clear vision can be obtained. Accommodative deficiency or weakness can result in very similar symptoms to those described for convergence deficiency. Accommodation should be measured in each eye in turn and with both eyes together. If uniocular accommodation is normal for the patient’s age and only binocular accommodation appears defective, this suggests that blurred vision is caused by defective convergence rather than defective accommodation
- The prism fusion amplitude or range. The positive amplitude will be poor in convergence deficiency, making it hard to maintain convergence
- By the cover test: The usual finding in convergence deficiency is slight exophoria for near, without significant deviation in distance. However, convergence deficiency can be associated with exophoria and, less commonly with esophoria. The speed of recovery to BSV should be recorded and the heterophoria measured using the prism cover test for preference
- By refraction: Small astigmatic or hypermetropic errors can cause similar symptoms to those already described, therefore the patient must be refracted and the refractive error corrected if necessary. Convergence should be reassessed after the spectacles have been worn for a few weeks
Treatment
Convergence deficiency is usually treated successfully by exercises to improve the near point and the positive fusion amplitude. The patient can be taught to do the exercises in the clinic and then practice them at home.
For diplopia: the patient must be able to appreciate diplopia when their convergence fails. Many patients can do this already, but a few suppress when one eye diverges. Diplopia can be taught using red and green glasses and a spotlight, which is moved closer to the eyes until one eye diverges: usually the patient will see 2 coloured lights; if not they can be shown where to look for the second light. Once they see two, the coloured glasses can be removed and they can try to see the lights without help. Most patients can do this without difficulty.
One pen exercise: Once the patient knows when his convergence fails, they can try to improve the near point by practicing convergence, bringing a pencil slowly towards their eyes, trying to keep it single. When diplopia occurs they can move it back a little and try to rejoin the images, then resume converging. They should be told to practice this several times 3 or 4 times each day. They should be warned that their symptoms may increase to begin with but should gradually improve as convergence gets easier.
Dot card
The dot card is used to improve convergence and can easily be made in the clinic. It consists of a strip of stiff cardboard about 30cm long with a line drawn down the centre of the card. A series of small circles is spaced out along the line, allowing 1-1½inches between each.
Method of use
The patient holds the card resting on the middle of his nose, tilted slightly downward. To exercise convergence the patient looks at each dot in turn, making sure that he sees it as a single dot, starting with the farthest dot, until he can no longer converge well enough to fuse the two dots. He should do this fairly slowly, returning to a slightly farther dot when his convergence fails and repeating the exercise.
As convergence improves, the patient should be able to change fixation quickly from a near dot to a far dot and back again.
The dot card is useful for patients with convergence deficiency to use at home in conjunction with stereogram cards, always practising the crossed position last to relax convergence.
Precautions
The patient must be given very clear instructions about the exercises they are to do at home, including the length of time he should spend on each and the number of times he should practice each day. He must demonstrate how to do each exercise before he leaves the clinic.
Accommodation weakness or insufficiency
Accommodative weakness gives rise to symptoms, especially if the patient does a lot of close
work. These comprise
- Blurred vision, either for all close work or occuring after reading for some time
- Headache and eyestrain associated with close work
Diagnosis
- History and symptoms: the type and duration of the symptoms must be noted. Accommodative problems should always be suspected if the main symptom is blurred vision for near in a person under presbyopic age. The ophthalmologist will want to know about the patient’s general health and if he is on any medication, as illness and certain drugs can sometimes cause the problem
- Measurement of the near point of accommodation, both uniocularly and binocularly, repeating each several times, using different test type if possible. The near point may come closer when the test is repeated. The diagnosis can be confirmed by using low power convex lenses (+1.0 or +0.50D). If accommodative deficiency is present, the print will become clear with the lenses. If a near point rule is not available, measurement can be made using a ruler and a reading test type
- The near point of convergence should also be measured. Poor convergence is sometimes associated with poor accommodation
- Refraction should be carried out, looking particularly for small degrees of hypermetropia or hypermetropic astigmatism
- Heterophoria should be detected by cover test and measured
Treatment
- Any hypermetropia or astigmatism should be corrected. Correction of even a small amount of hypermetropia can help relieve the symptoms. The near point should be reassessed after the glasses have been worn for a few weeks
- Poor general health should be improved if possible
- Temporary convex lenses can be prescribed if there is no refractive error. Often one D or even 0.5 D is enough
- Convergence can be improved if necessary. It should first be reassessed with any glasses ordered as it can then improve spontaneously. In other cases improvement of convergence also results in improved accommodation
Heterophoria
Symptoms of heterophoria occur if the patient is unable to control the phoria easily. They comprise headache and eyestrain caused by the effort to maintain BSV and intermittent diplopia and blurred vision due to failure to control the phoria.
Diagnosis
- Cover test, noting the type and amount of heterophoria and the speed of recovery to BSV
- Measurement of the amount of heterophoria, preferably by prism cover test, alternatively the Maddox rod can be used for near and distance
- Measurement of the near points of convergence and accommodation
- Measurement of the prism fusion amplitude
- Refraction should be carried out and any significant refractive error corrected. The effect of spectacles should be assessed before considering further treatment, because the patient’s symptoms may resolve once they are worn
Treatment
Orthoptic exercises
Heterotropia
- Some types of exotropia are treated with orthoptic exercises
- Some types of esotropia are associated with some amount of hypermetropia. When hypermetropia is corrected the esotropia disappears
- Esotropia is seen when the spectacles are removed. Constant tropias are to be treated surgically
Summary
This unit deals with squint or strabismus, which is mostly identified at the childhood. There is a misconception that squint is a sign of good fortune, but untreated squint will lead to lazy eye or amblyopia. Loss of vision is preventable if squint is detected and treated before two years of age. As the child grows older, it becomes more difficult to treat squint and establish binocularity. Cosmetically straightening the eyes is possible at any age.
There are no known preventive measures for squint, but misaligned eyes can be straightened and loss of vision from amblyopia can be prevented if treatment is begun early. The OA should know the different types of squint and their treatment. The OA must be able to identify the type of squint and must know to choose the appropriate examination to measure the level of vision and squint and make the task easy for the ophthalmologist.
Key points to remember
- If BSV is absent, there is no possibility of presence of fusion and stereopsis
- If convergence weakness is identified, check accommodation uniocularly
- Exophoria is an indication of fusion weakness
- While checking ocular movements, both eyes must be visible to the examiner
- While checking cover test, the examiner must give the patient time to fix steadily before removing the cover or changing it to the other eye.
- Testing accommodation is purely subjective
Student exercise
True / False
- Esotropia is a vertical deviation of eye ( )
- Lateral rectus muscle is supplied by 3rd nerve ( )
- Normal positive fusional range is 30 – 40 prism ( )
- Version is conjugate or parallel eye movement ( )
- Tropia is a constant squint ( )
Fill up the blanks
- Medial rectus muscle is supplied by _______________ nerve.
- The actions of superior oblique muscles are _______________, ____________.
- Phoria is detected by _____________.
- Convergence and accommodation are measured by ____________.
- BSV is checked by ______________ test.
Answer the following
- Define squint.
- List the names of the extra ocular muscles.
- Describe how to check binocular vision.
- What are the instruments used to check binocular vision and fusion?
- How will you find squint?