Refractive Errors and Management
Refractive errors are the most common eye disorders and not a disease. A refractive error means that the shape of the human eyes do not refract the light rays correctly on the retina resulting blurred vision. Emmetropia is a normal refractive condition of the eye in which the parallel light rays from infinity comes to a focus exactly on the retina without any accommodative changes. So the vision is clear at all distances. In case the rays are focused either infront or behind the retina, then it is termed as ametropia. It can be classified as short sightedness or myopia and long sightedness or hypermetropia.
Myopia
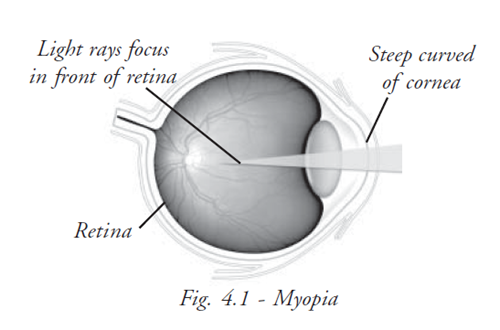
Myopia is one type of refractive error where the parallel rays of light are brought into focus in front of the retina when accommodation is at rest. This is also called short sightedness or nearsightedness. Nearsightedness is an error of visual focusing that makes distant objects appear blurred.
Aetiology
- Axial myopia - is due to increase in the anteroposterior length of the eye ball
- Curvature myopia - is due to increases in curvature of cornea or one or both the surfaces of the lens. Increases of 1 mm causes a refractive change of 6D
- Index myopia - a change of refractive index in the lens results in index myopia
- Positional myopia - this is due to anterior placement of lens
Optical Condition
In myopia, the parallel rays of light fall in front of the retina and cause a blurred image to fall on retina. So the distanct object appears blurred. In order to see clearly the object is brought closer and the divergent rays come to focus on the retina. This makes the far point in the myopic eye at a finite distance. This distance decreases with the increase in the degree of myopia. Therefore the near object is focused without an effort of accommodation. For these reason myopes can suffer from convergence insufficiency and exophoria.
Clinical types of myopia
Congenital Myopia: It is present at birth and may be unilateral or bilateral. Bilateral congenital myopia may be associated with squint. Simple myopia: It is the most common type of myopia, results from the normal biological variation in the development of the eye. The power of glasses increases, usually during the years of study in schools and colleges and then remains steady. This type of myopia is not associated with any degenerative change in the eye. Pathological myopia: In this condition, the myopia rapidly progresses and subnormal visual acuity persists even with correction and there are degenerative changes in the retina. Near-sightedness affects males and females equally, and those with a family history of nearsightedness are more likely to develop it. Most eyes with nearsightedness are entirely healthy, but a small number of people with myopia develop a form of retinal degeneration.
Simple Myopia: It is the most common type of myopia, results from the normal biological variation in the development of the eye. The power of glasses increases, usually during the years of study in schools and colleges and then remains steady. This type of myopia is not associated with any degenerative change in the eye.
Pathological Myopia In this condition, the myopia rapidly progresses and subnormal visual acuity persists even with correction and there are degenerative changes in the retina. Near-sightedness affects males and females equally, and those with a family history of nearsightedness are more likely to develop it. Most eyes with nearsightedness are entirely healthy, but a small number of people with myopia develop a form of retinal degeneration.
Acquired Myopia This occurs due to exposure to various pharmaceuticals, increase in glucose level, nuclear sclerosis, and increase in curvature of the cornea in conditions such as corneal ectasias. The other types of acquired myopia are:
Pseudo Myopia : This type of myopia is called as false appearance of myopia that occurs due to excessive accommodation and spasms of accommodation.This type of myopia usually manifest the execessive amount of myopia and decreased amount of hypermetropia.It could cause severe headache with asthenopic complaints.
Night Myopia : In night myopia, the eye has difficulty seeing in low illumination even though the daytime vision is normal. This occurs due to increase in sensitivity to the shorter wavelengths of light. Younger people are affected more than the elderly.
Space Myopia: This type of myopia occurs when the individual has no stimulation for distance fixation.
Symptoms
- Blurred vision or difficulty in seeing distant objects (Children often cannot read the blackboard, but easily read a book).They tends to go near the objects to see clearly
- Eye strain
- Headaches (uncommon)
- Squinting tendency
- Close working habits
Tests
A general eye examination or standard ophthalmic exam may include:
- Visual acuity, both at a distance (Snellen’s), and close up (Jaeger)
- Refraction test to determine the refractive power accurately
- Cycloplegic refraction may be required in few conditions to confirm the final prescription
- Color vision test to exclude color defect.
- Muscle balance test
- Slit lamp examination of the eyes
- Measurement of the intra ocular pressure of the eyes
- Retinal examination
Complications
- If a person with nearsightedness has flashing of lights, floating spots, or a sudden loss of any part of the field of vision, it may be a retinal detachment.
- Retinal atrophy patches in the macula cause loss in central vision
Expectations (prognosis)
Early diagnosis of myopia is important, since a person can suffer socially and educationally by not being able to see well at a distance. Any degree of myopia that is occurring in a child under the age of 4 requires immediate observation. In high degree of myopia the prognosis is always guarded. It is usually based on the appearance of fundus and the acuity of vision after correction.
Management
Myopia is easily corrected by concave lens for eyeglasses or contact lenses. The lens diverge the incoming light rays, so that they will be properly focused on the retina.
Surgical treatment
There are also a number of techniques available for reshaping the cornea (the front surface of the eye), in order to reduce its power and thus correct the myopia. One technique (known as orthokeratology or ‘Ortho-K’) uses rigid contact lenses to change the shape of the cornea. Other techniques use surgery to remove tissue from the cornea, leaving it with a flat surface.
There are several surgical procedures that reshape the cornea, shifting the focus point from in front of the retina to on to the retina.
Radial keratotomy is a surgical procedure popular in recent past. Now it is almost completely replaced by LASIK, in which an excimer laser is used to reshape the cornea. Refractive surgeries are recommended for persons aged between 20 and 40 years.
Students exercise
Answer the following
Hypermetropia
Definition
Hypermetropia is an error of refraction in which parallel rays of light from infinity come to a focus behind the retina, when accommodation is at rest.
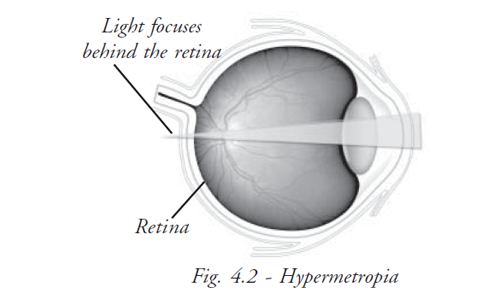
Optical Condition
Whether the hypermetropia is due to a decrease in the length of the eye ball or decrease of curvature of cornea or due to change in refractive index, the optical effect is the same, parallel rays from infinity come to focus behind the retina, and the diffusion circles which are formed on the retina result in a blurred and indistinct image.
Accommodation Eye
Parallel rays are brought to focus on the retina, by the normal lens in the eye becoming more complex. This is called accommodation.
Hypermetropic Eye
Parallel rays of light are brought to focus upon the retina, by increasing the refractivity with a convex spectacle lens. The degree of hypermetropia is given by the power of the correcting lens.
Types of Hypermetropia
- Axial Hypermetropia
- Curvature Hypermetropia
- Index Hypermetropia
Axial Hypermetropia: When the anterior / posterior length of the eyeball is shorter than normal. (Normal axial length is 24mm). A decrease of 1mm in axial length produces a hypermetropia of 3.0D.
Curvature Hypermetropia: When the curvature of the cornea or lens is flatter than normal. An increase of 1mm in its radius of curvature produces a hypermetropia of 6.OD.
Index Hypermetropia When the refractive index of the media is less than normal
- Corneal refractive index - 1.37
- Refractive index of the cortex of lens - 1.38
- Refractive index of the nucleus of lens - 1.40
Clinical types of Hypermetropia
- Congenital hypermetropia
- Simple or developmental hypermetropia
- Acquired hypermetropia
Congenital hypermetropia : This is rare. It is usually associated with other congenital anomalies of the eyeball like microopthalmas.
Simple or developmental hypermetropia: It is the most common type. A newborn baby is hypermetropic but with age, the eye ball grows in size and the hypermetropia is gradually diminished. If the growth of the eyeball is retarded then hypermetropia persists.
Acquired hypermetropia This is found in aphakic conditions, commonly following extraction of the lens. This hypermetropia is usually high about + 10.0 D.
Effect of accommodation on Hypermetropia
Total Hypermetropia
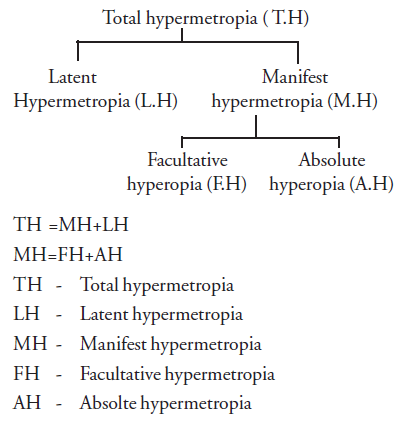
The hypermetropia which is seen after complete paralysis of accommodation, after the application of atropine TH=MH+LH
Latent hypermetropia
It is the amount of hypermetropia which is corrected by normal physiological tone of the ciliary muscle. It is strong in young age and slowly declines with age.
Manifest hypermetropia
The remaining portion which is not corrected by the normal physiological tone of the ciliary
muscle, is called manifest hypermetropia. It is the hypermetropia that remains uncorrected
in normal circumstance. That is when accommodation is not being actively used, or, in other
words it is the total hypermetropia minus the latent hypermetropia. This manifest
hypermetropia is again made of two components.
1. Facultative hypermetropia
2. Absolute hypermetropia
Facultative hypermetropia
It is the part of hypermetropia, which can be corrected by an additional effort of accommodation or excessive strain of the ciliary muscle.
Absolute hypermetropia
It is the part of hypermetropia which cannot be overcome by active exertion of accommodation.
Symptoms of Hypermetropia
- Head ache
- Eye strain
- Distance blurred vision
- Difficulty in doing prolonged close work
Treatment of Hypermetropia
- By prescribing correct convex lenses
- Contact lenses
- Lasik
Scientific Correction of Hypermetropia
Donder’s formula
To be used for correcting manifest hypermetropia.
Formula : Rx=MH+1/3 LH
Donder’s Formula is useful to determine the actual amount of hypermetropic correction in
different cases.
- Even if the patient has mild headache associated with the problems of asthenopia then the
final correction will be based on this formula Rx = MH +1/4 LH
- If the patient has headache and the problem of difficulty in reading and other near vision
tasks then the correction will be Rx=MH+1/2 LH
- If the patient has esotropia then we have to give full correction, Rx will be Rx = MH + LH
Example :
If the patient having vision 6/9 improves with +0.50DSph to 6/6, by fogging method, patient
reads 6/6 with +2.0 DSph and after a cycloplegic refraction patient reads 6/6 with +3.5DSph.
Find MH, AH, FH, LH, and TH
AH = +0.5 DS
MH = +2.0 DS (By fogging method)
And TH = +3.5 DS (By cycloplegia)
MH = AH+FH
FH = MH – AH
= +2.0 DS - +0.5 DS = + 1.50 DS
TH = MH +LH
LH = TH-MH
= 3.5 DS – 2.0DS = +1.5 DS
So final correction by Dondler’s formula
Rx = MH+1/3 LH
= +2+1/3X1.5
= +2+0.5 = +2.5DS
Complication of hypermetropia
Uncorrected hypermetropia leads to esophoria, which later on may develop into esotropia.
Hypermetropia with esophoria - To give full correction
Hyperopia with exophoria - To give under correction
Hypermetropic individuals often have shallow anterior chamber. They have increased
predisposition to develop narrow angle glaucoma.
Astigmatism
Astigmatism is a type of refractive error where the refraction varies in different meridians. Consequently the rays of light entering in the eye cannot converge on a focus point, but form focal lines.
Aetiology
- Corneal astigmatism is the result of abnormalities of curvature of the cornea.
- Lenticular astigmatism is rare. It may be:
- Curvature due to abnormalities of curvature of lens as seen in lenticonus
- Positional due to tilting, or oblique placement of lens as seen in subluxation
- Index astigmatism occurs rarely due to variable refractive index of lens in different meridian
- Retinal astigmatism, due to the oblique placement of macula, is seen occasionally
Types
Broadly, there are two types of astigmatism,
- Regular astigmatism
- Irregular astigmatism
Regular astigmatism
The astigmatism is regular when the refractive power changes uniformly from one meridian to another. Depending upon the axis and the angle between the two-principle meridians, regular astigmatism can be classified into the following three types.
Horizonto-vertical astigmatism In this type the two principal meridians are placed
at right angles to one another and those are in the horizontal (180 +/- 20) and vertical
planes (90+/- 20). It is of further two types
With the rule astigmatism: When the vertical meridian is more curved than the
horizontal meridian, this is known as with the rule astigmatism. Sometimes it is
physiological due to pressure of the eyelid on the cornea. Up to 0.50D we can ignore the
error, as it does not cause many symptoms.This can be corrected either by a – (minus)
cylinder x 180 or + (plus) cylinder x 90.
Against the rule astigmatism: The horizontal meridian is more curved than the
vertical meridian. This is known as inverse astigmatism or against the rule astigmatism. It
cause more symptoms and should be corrected for minimal error. This can be corrected either
by – (minus) cylinder x 90 or + (plus) cylinder x 180.
Oblique astigmatism: When principle meridians are at right angles, but are not
vertical and horizontal.
Bi-oblique astigmatism: When principle meridians are not at right angles but crossed
obliquely.
Refractive types of regular astigmatism
Depending upon the position of the focal lines in relation to the retina, regular astigmatism is further classified into three types,
Simple astigmatism:
Here the rays are focused on the retina in one meridian and in front or behind the retina on
the other meridian, as in simple hypermetropic (Fig 4.3b) or simple myopic (Fig 4.3a)
astigmatism.
Compound astigmatism
Here neither of the two foci lies upon the retina but are placed in front or behind it. The
former is known as compound myopic (Fig. 4.4a), the later as compound hypermetropic
astigmatism. 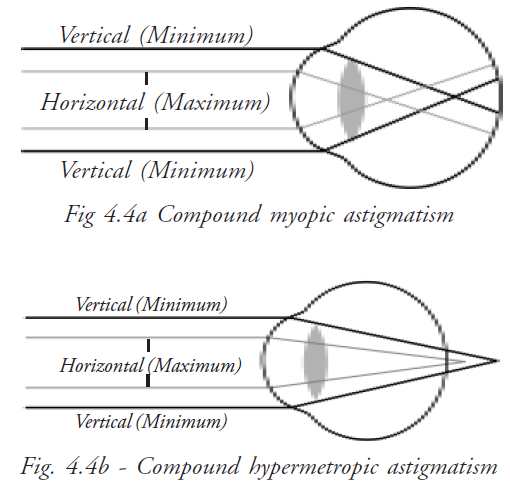
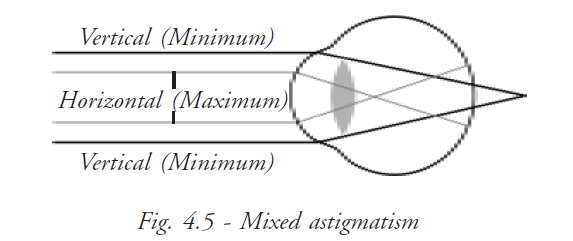
Mixed astigmatism
One focus is in front of and the other behind the retina, so that the refraction is hypermetropic in one direction and myopic in the other (Fig. 4.5).
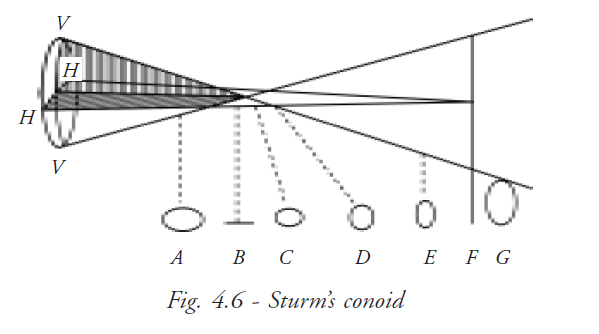
Appearance of image in astigmatism - Sturm’s conoid
Sturm’s conoid is a series of images formed by astigmatic surface, which have two meridians of different curvature. The more curved meridian refracts rays greater than the less curved meridian. Rays refracted by more curved meridian come to focus earlier than those refracted by less curved meridian. It forms two focal lines (B and F). Distance between these two focal lines is known as focal interval (BE). Circle of least diffusion is formed when rays refracted by both meridians have equal and opposite tendencies. At this point the most clear image is formed. Images in between and beyond the focal lines are blurred and elliptical (Fig. 4.6).
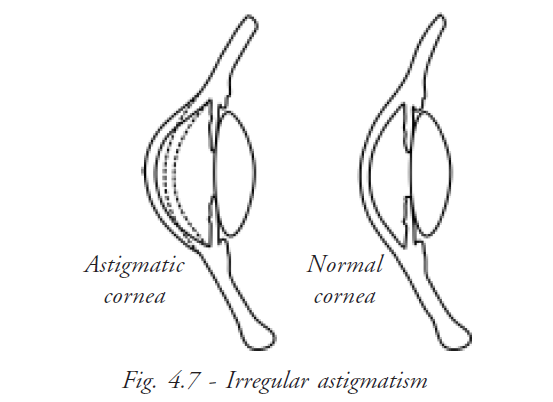
Irregular astigmatism
Irregularities in the curvature of the cornea cause Irregular Astigmatism. The principal meridians are not at right angles. Every meridian in the cornea has a separate type of refraction; we can never correct the error by spectacles. This type of astigmatism is called irregular astigmatism (Fig. 4.7).
Symptoms
- Defective vision
- When they look at a straight line either it is blurred or the line can be tailed off at the end
- Headache is an important complaint
- Giddiness
- Torticollis - permanent tilting of head
Tools used in evaluation of astigmatism
- Keratoscopic examination by placidos disc
- Retinoscopy by concave mirror/streak
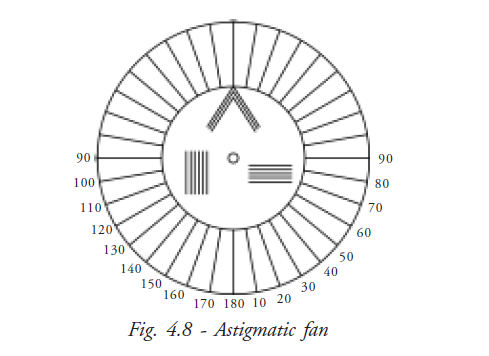
- Use of astigmatic fan or Maddox rod
- Stenopaeic slit or pinhole
- Keratometry
- Jackson cross cylinder
Astigmatic fan
Astigmatic fan is a construction of vertical lines at a different angle meridian from 0 to 180 degrees. When a patient with astigmatic error looks at the fan some lines seem to be clearer than others, which help to detect the axis of astigmatism (Fig. 4.8).
Jackson’s cross cylinder
The cross cylinder is a sphero-cylinder lens in which the power of the cylinder is twice the power of the sphere and of the opposite sign. It is used to refine power and axis of cylindrical power.
Stenopic slit
The stenopaeic slit can be used to determine the refraction and principle axis in astigmatism. The slit aperture acts as an elongated ‘pin hole’, only allowing light in the axis of the slit to enter the eye.
Placido’s disc
This is a flat disc bearing concentric black and white rings. A convex lens is mounted in an aperture in the center of the disc.
Treatment
Regular astigmatism
Optical correction
- Spectacle (concave – convex cylinder lens)
- Contact lens (toric lens - prism balastic lens)
Surgical
- Keratomiluesis
- Excimer laser
Irregular astigmatism
Hard/semi-soft contact lens
- Keratoplasty in central area of conical cornea
- Excision of scar + replacement by graft
Summary
Astigmatism is a type of refractive error where no point focus is formed on the retina. Two main types of astigmatism are regular and irregular astigmatism. ‘With the rule’{ – (minus) cylinder x 180 or + (plus) cylinder x90} and ‘against the rule’ {– (minus) cylinder x 90 or + (plus) cylinder x 180} astigmatism are the types which are of more interest as we can understand patient symptoms. Refractive types includes simple, compound and mixed astigmatism. Optics of astigmatism can be explained by sturm’s conoid. To find the axis of astigmatism we can use stenopic slit, placido’s disc, astigmatic fan and some techniques of retinoscopy. We can use JCC to refine power and axis of astigmatism. Cylindrical and spherocylindrical lenses can be used to correct astigmatism. Contact lens and surgery are the other options.
Key points to remember
- Minimum cylinder, maximum comfort
- Give minus cylinder for more comfort
- For high cylinder, it is better to do keratometry
- Refine axis and power before finalizing prescription
- Check binocular comfort subjectively
Student exercise
Answer the following
- 1. What is astigmatism? What are the possible causes of astigmatism?
- 2. What do you understand by ‘with the rule’ and ‘against the rule’ astigmatism?
- 3. What are the refractive types of astigmatism?
- 4. What is JCC? Write its uses.
- 5. What are the possible ways to correct astigmatism?
Presbyopia
Presbyopia is an age related progressive loss of the focusing power of the lens. This results in difficulty in reading and seeing near objects.
Causes, incidents, and risk factors
- The focusing power of the eye, which depends upon the inherent elasticity of the lens, gradually decreases in old age.
- This causes inability to read at normal reading distance (33 cm to 40cm)
- People usually notice the condition around age 40; after they realise that they need to hold reading materials further away in order to focus.
Signs and tests
A general eye examination will be performed including measurements to determine a
prescription for glasses or contact lenses.
Tests may include:-
- Visual acuity
- Refraction
- Muscle integrity
- Slit lamp
- Retinal examination
Symptoms
- Inability to focus near objects
- Likes to read in brilliant illumination when the pupil will be forced to constrict
- Eye strain
- Headache
Factors affecting close work
- Pupil size - Smaller pupils increase the pinhole effect, which increases the depth of focus
- Lighting - Small print is easier to read in bright light. The contrast is improved and the reflected light may constrict the pupil, improving the depth of field
- Print size and print distance - large print is easier to read
- Task requirements - An accountant will need better near vision than a garbage worker
- Secondary task considerations - A person wants to increase the near working distance in one pair of glasses rather than buy two pairs of glasses
- Body type and position - some people, particularly those with long arms, like to hold reading materials further away than others do. In this case the add power will be less
- Previous correction - Many people don’t tolerate an increase in add power greater than 0.75D at any one time
- Low ametropia - Uncorrected low hypermetropes complain of reading difficulty at an earlier age than uncorrected low myopes.
- Health and medications - Diabetics typically need near correction at an earlier age and need stronger add power than is normal for their age group.
| Age | Expected Add Power |
| 38 yrs | + 0.75 DS |
| 40 yrs | +1.0 DS |
| 45 yrs | + 1.50 DS |
| 50 yrs | + 2.0 DS |
| 55 yrs | +2.5 DS |
| 60 yrs and above | +3.0 DS |
Variations of accommodation with age
| Amplitude of accommodation | Age | |||
| Early Age | 36 yrs | 45 yrs | 60 Yrs | |
| 14 D | 7 D | 4 D | 1 D | |
| Near Point | 7 cm | 14 cm | 25 m | 1m |
Evaluation of presbyopia
Treatment
Presbyopia can be corrected with appropriate lenses, so that his accommodation is reinforced and the near point is brought within the useful working distance.
- Know the working distance of the patient for proper addition
- Refraction
- Determine the amplitude of accommodation
- Supplement this by lens - allowing him a sufficient reserve of accommodation
For example
Emmetropic working distance - 25 cm
Requires amplitude of accommodation - 4 D (100/25)
Near point receded at - 50 cm
Accommodation - 100/50 = 2D
Keep 1/3 reserve for comfort - 1/3x2 = 0.66
Available accommodation ( 2/3 of amplitude) = 1.3D (2-0.66)
Required lens = 4-1.3 D=2.7 DS
Key points to remember
- Presbyopic spectacle should never be prescribed mechanically based on age
- Lenses must be comfortable
- Vision for the particular work for which their spectacle is intended must be kept in mind
- Start with an addition of +0.75D
- Better to under correct than over correct
- Lenses that bring the near point closer than 28cm are rarely tolerated
- Demand for higher correction than convergence should be added with base in prism
- Patient with early cataract can read with +3.50 D or + 4.0D addition
- Usual discomfort for presbyopic optical correction is due to over correction
Types of corrective spectacle for presbyopia
- Single vision reading glasses
- Bifocals - where glasses are given for near and distance
- Trifocals - where glasses are given for distance, intermediate and near vision
- Varifocals - progressive addition lens
- Monovision correction- one eye is corrected for distance and the other eye for near
Student exercise
Answer the following
- Define presbyopia
- What are the symptoms of presbyopia?
- Describe the treatment for presbyopia
- Mention the important points to be noted while prescribing spectacles for presbyopia
- What are the types of spectacles that could be prescribed for presbyopia?