Visual Fields
The visual field is that portion of space in which objects are simultaneously visible to the steady fixing eye.
Normal Visual Field
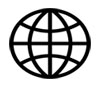
The normal monocular visual field is a slightly irregular oval, which measures, from fixation, approximately 60° upward and 60° inward, 70° downward and 100° to 110° outward.
The field of the two eyes together or the binocular field is a combination of the right and left monocular fields. The whole binocular field forms a rough oval extending to about 200° laterally and 130° vertically.
The extreme extent of the visual field is limited by the nose and the brows, but within the anatomic restrictions imposed by these structures, the normal field may be considered from a practical point of view as being made up of two portions:
- The central field: that portion of the visual field within 30° radius of fixation
- The peripheral field: The peripheral field makes up the remainder of the visual field
Normal monocular fields
|
Superior side |
60° to 70° |
|
Inferior side |
70° to 80° |
|
Nasal side |
50° to 60° |
|
Temporal side |
100° to 110° |
Normal binocular fields
|
Horizontal side |
200° |
|
Vertical side |
110° |
Physiological blind spot
This is an area of absolute scotoma (non-seeing area) within the boundaries of the normal visual field, and it corresponds to the region of the optic nerve head. It is located approximately 15° temporal to the fixation point and about 1.5° below the horizontal meridian. The normal measurement of the blind spot is approximately 5.5mm horizontally and 7.5mm vertically.
Traquair's concept
Traquair's definition of the visual field is that it is an island of vision in the sea of Blindness. The peak of the island represents the point of highest acuity, the fovea, while the 'bottomless pit ' represents the blind spot, the optic disc.
If we refer to Traquair's concept of an island hill of vision, the outline of the various contours of this hill may be projected upon a map as contour lines, which, in the nomenclature of perimetry are termed isopters. The central point from which these isopters are measured corresponds to the visual axis and is known as the point of fixation.
The isopters or contour lines are designated by the size and brightness of the stimulus and the distance at which it is viewed by the observer, expressed as a fraction. Thus isopter for a 1 mm. test object observed by the patient at a distance of 2 meters is expressed by the fraction 1/2000 and designates the specific area of the visual field within which the normal person should be able to see this stimulus.
Principle
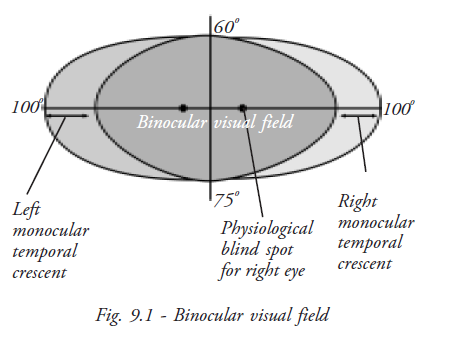
The nasal field represents the temporal retina and the temporal field represents the nasal retina.
The visual pathways
- The end organ: Is the neural epithelium of the rods and cones
- The first-order neurone: Is the bipolar cell with its axons in the inner layers of retina
- The second order neurone: Is the ganglion cell of the retina. Its axon passes into the nerve-fibre layer and along the optic nerve to the lateral geniculate body.
- The third-order neurone: Originates in the cells of lateral geniculate body, and then travels by way of the optic radiations to the occipital cortex (visual centre).
The visual pathways thus consist of:
- Two optic nerves
- An optic chiasma
- Two optic tracts
- Two lateral geniculate bodies
- Two optic radiations, and
- Visual cortex on each side
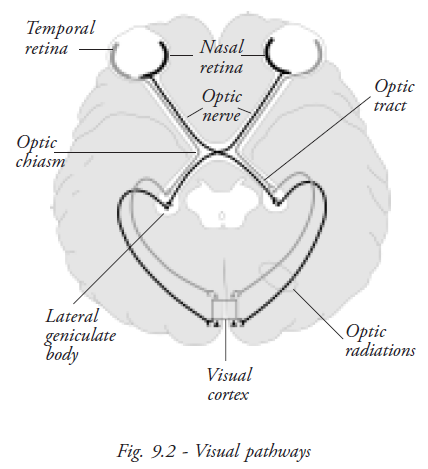
The distribution of the various nerve fibre bundles within the retinal nerve fibre layer
In general, the fibres from the peripheral retina enter the periphery of the optic nerve, and the fibres near the optic disc enter the central part of the nerve.
The fibres from the macular area forms the papillo-macular bundle, which has a separate course, partial decussation occurs where the nasal fibres cross at the chiasm.
The fibres of the temporal half enter the chiasm and pass to the optic tract on the same side, and then to the lateral geniculate body. The fibres from the nasal half enter the chiasm, decussate, and then pass to the optic tract of the opposite side, then to the lateral geniculate body.
The third-order neurons pass by the optic radiation into the corresponding occipital lobe. It follows that a lesion of the optic radiation, optic tract, or occipital lobe will cause blindness of the temporal half of the opposite side. Projecting this outward, such lesion will cause loss of vision in the opposite half of the visual field, a condition known as hemianopia.
Abnormal Visual Field
Three basic defects of visual fields are:
- Contraction
- Depression and
- Scotoma
Contraction
True contraction is relatively rare. To satisfy the definition of contraction, the area of the visual field that is defective must be totally blind to the stimuli, no matter how bright or how large a target is presented in that area. The edge of the defect must be the same regardless of the intensity of the stimulus.
Contractions may have various forms;
- General peripheral
- Partial peripheral
- Sector
- Partial hemianoptic
- Total hemianoptic and
- Scotomatous. They may be either monocular or binocular.
Depression
The great majority of visual field defects, both peripheral and central, are caused by depression and may be very marked (but not absolute) or very slight. It may involve only the extreme periphery or only the minutest portion of the fixation area. It may take an almost infinite variety of forms.
Visual field depression may be divided into
- General depression and
- Local depression.
General depression
General depression of the visual field is one in which all the isopters are smaller than normal and some of the internal isopters are missing. In fact the central isopters are the first and most severely affected.
Local depression
Local depression of the visual field is the most common type of defect. It may take many forms, including scotoma.
Scotomas
A scotoma is an area of partial or complete blindness within the confines of a normal or a relatively normal visual field (i.e.). it is a defective field surrounded by a normal field.
Types of scotoma
Absolute scotoma: An absolute scotoma will have the same field defect size regardless of the target size and brightness.
Relative scotoma: Relative scotoma has field defects that change with the target size and have sloping borders that indicates an active or on going field defect.
- Positive scotoma: Patient complaints of non-seeing area (e.g.) Central scotomas
- Negative scotoma: Examiner detects the non-seeing area (e.g.) blind spot enlargement
Scotomas may be unilateral or bilateral.
Basic terminologies
Horizontal meridian: Horizontal line through fixation which divides superior and inferior visual fields.
Vertical meridian: Vertical line through fixation which divides left and right visual field.
Isopter: Line connecting points of equal visual sensitivity
Scotoma: Area of reduced visual sensitivity
Arcuate or Bjerrum scotoma: Arching visual field defect within the area between 10 to 25 degrees in the superior and inferior field Central scotoma: Defect involving fixation
Ceco-central scotoma: Defect encompassing the physiologic blind spot and fixation.
Para-central scotoma: Defect close to but not involving fixation
Altitudinal: Complete loss of either superior or inferior field nasal to the physiologic blind spot
Hemianopic / hemianopsia: Defect respecting the vertical meridian.
Quadranopic / quadranopsia: Defect respecting the vertical meridian involving only one quadrant.
Homonymous: Defect occupies the same side of visual space in both eyes.
Congruous: Bilateral hemianopic defects which are essentially identical; the fields can be superimposed on one another. Congruity indicates a more posterior location of the lesion.
Incongruous: Hemianopic defects which are not identical. Incongruity indicates an anterior lesion location.
Field defects in various parts of the visual pathways
Optic nerve: Blindness on side of lesion with normal contralateral field.
Chiasm: Bitemporal hemianopia.
Optic tract: Contralateral incongruous homonymous hemianopia.
Optic Nerve and Chiasmal junction: Blindness on side of lesion with contralateral temporal hemianopia or hemianoptic scotoma.
Posterior optic tract, external geniculate ganglion, posterior limb of internal capsule: Complete contra lateral homonymous hemianopsia or incomplete incongruous contralateral homonymous hemianopsia.

Optic radiation: Anterior loop in temporal lobe- incongruous contralateral homonymous hemianopia or superior quardantanopia.
Medulated fibers of optic radiation: Contralateral incongruous inferior homonymous quadrantanopsia.
Optic radiation in parietal lobe: Contralateral homonymous hemianopia sometimes slightly incongruous with minimal macular sparing.
Optic radiation in posterior parietal lobe and occipital lobe: Contralateral congruous homonymous hemianopia with macular sparing.
Mid portion of calcarine cortex: Contralateral congruous homonymous hemianopia with macular sparing and sparing of contralateral temporal crescent.
Tip of occipital lobe: Contralateral congruous homonymous hemianoptic scotoma.
Anterior tip of Calcarine fissure: Contralateral loss of temporal cresent with otherwise normal visual fields.
Glaucoma fields
More specific defects of glaucoma are,
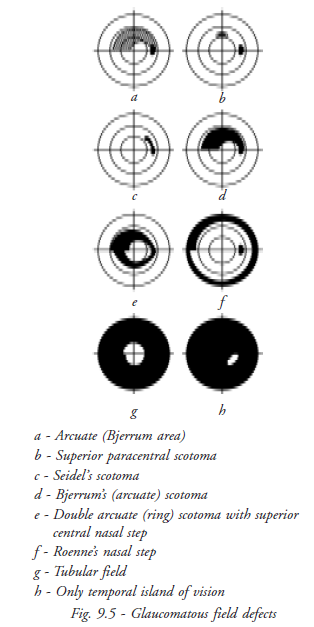
Isopter contraction: Peripheral isopter contraction may be significantly smaller prior to any field loss
Baring of the blind spot: (exclusion of the blind spot) is also considered to be an early field defect in glaucoma.
Angio-scotoma: Long, branching scotoma, above or below the blind spot, which are presumed to be the result of shadows created by large vessels, and are felt to be an early change.
Isolated paracentral scotoma: One or more isolated paracentral scotoma develop in the Bjerrum or arcuate area.
Seidel's scotoma: A sickle-shaped defect arises from the blind spot and tapers to a point in a curved course with concavity towards the fixation point.
Bjerrum's or arcuate scotoma: A relatively larger area of defect in the form of arching scotoma, which eventually fills the entire arcuate area, from blind spot to the horizontal median. With further progression, a double arcuate (ring or annular) scotoma will develop.
Roenne's nasal step: The arcuate defects may not proceed at the same rate in the upper and lower portions of the eye. Consequently, a step-like defect is frequently created where the arcuate defects meet at the median. This is called Ronne’s nasal step and it is mostly a superior nasal step, as the superior field is involved more frequently.
Generalised constriction of peripheral field: Double arcuate scotoma leads to tubular field of vision (tubular vision) in which only the central vision remains clear.
Lastly, only a paracentral temporal island of vision persists, central vision being destroyed.
Ultimately, all the nerve-fibres are eventually destroyed with no perception of light.
Field examination
Perimetry
Perimetry is the procedure of estimating the extent of visual fields. Several types are available;
Kinetic perimetry
In this the stimulus of known size and luminance is moved from periphery towards the centre to establish isopters. Various methods of kinetic perimetry are: confrontation method, tangent screen scotometry, Lister’s perimetry and Goldmann’s perimetry.
Static perimetry
The visual field can be plotted by using a stationary light target of variable brightness and size against a background whose luminance may be similarly adjusted (either photopic or scotopic conditions).
Example: Humphrey Visual Field Analyzer
In general, static perimetry is superior to the kinetic method for glaucoma patients, as it is more accurate and reproducible.
Methods of estimating Visual Field
Confrontation method
The confrontation field test compares the boundaries of the patient’s field of vision with that of the examiner, who is presumed to have a normal field. It is a rough, but very useful clinical test, which should be applied in every case, if there is any suspicion of a defect in visual field.
Performing the confrontation test
- Seat the patient at a distance of 2 to 3 feet from you. Confront (face) the patient, cover or close your left eye, and have the patient cover the right eye. You and the patient should fixate on each other's uncovered eye
- Extend your arm to the side at shoulder height and slowly bring two fingers from beyond
your peripheral vision toward your nose into the field of vision midway between the
patient and yourself. Ask the patient to state when the fingers are visible
Repeat the process of moving fingers into the visual field from four different directions. If you picture a clock face in front of the patient's eyes, you perform the hand movement from about 2 O'clock, 4 O'clock, 8 O'clock, and 10 O'clock, each time bringing the fingers toward the center of the clock face - The patient should see the fingers at the same moment you do in each of the four quadrants (upper-left, upper-right, lower-right and lower-left quarters) of the visual field. (Note: A quadrant of vision described from the patient's point of view). If the patient does not see your fingers at the same time you do, the breadth of patient's visual field in that quadrant is considered to be smaller than normal and additional perimetric studies are performed
- Record the patient's responses in the patient's chart by indicating simply that the visual field is comparable to yours or that it is reduced in any of the four quadrants for that eye
- Repeat the procedure as described with the patient's other eye and record the results similarly
Tangent Screen (Bjerrum screen)
Estimation of defects of central fields using tangent screen is termed as campimetry or scotometry. It is done to evaluate the central and para central area (30 degree) of the visual field. The tangent screen is 1 metre or 2 metres square. Accordingly the patient is seated at a distance of 1m or 2m respectively.
The screen has a white object for fixation in its centre, around which are marked concentric circles from 5 degree to 30 degree. The patient fixates on the central dot with one eye occluded.
A white target (1-10 mm diameter) is brought in from the periphery towards the centre in various meridians. Initially, the blind spot is charted, which is normally located about 15 degree temporal to the fixation point on a 1 m tangent screen. It will fall outside the 1m tangent screen at 2m. Doubling the testing distance and doubling the target size will double the scotoma size.
Note
Fixation targets should be capable of variation from 1 to 100 mm. Circles of varying size are used for fixation when testing for small central scotomas
White tape may be attached to the two upper corners of the screen so that they cross in the centre when testing the large, dense, central scotomas. The patient fixates where they think the tapes will cross even though they cannot see the actual crossing point
Performing the tangent screen examination
- For a tangent screen examination, it is essential that the patient wears his glasses if he has a refractive error. This is not essential in perimetric examinations
- The examiner usually stands to one side and keeps his/her eye on the patient's eye to ensure that the fixation is absolutely maintained
- The test object, the size of which is correlated with the patient's visual acuity, is moved from the periphery towards the centre
- The patient indicates when they see the test object either by making a verbal response, such as ''yes'', or by tapping a coin
- At all times the fixation of the patient should be checked
- The easiest way is to map out the patient's blind spot first, which is smaller and closer to the fixation point
- Check the patient's responses by rotating the test object out of view so that it is not visible to the patient at all
- Be careful when transferring the information from the felt screen to the chart because errors can occur
- Make sure you understand the proper degree of eccentricities and meridian placements on the stitched chart and the recording diagrams
- Mark the areas of scatter with a cross hatch and record the target size
- Evaluate each scotoma for depth with smaller and larger targets
Amsler grid test
The Amsler grid test determines the presence and location of defects in the central portion of the visual field. The Amsler grid is a printed square of evenly spaced horizontal and vertical lines in a grid pattern, with a dot in the centre. The chart grid and dot may be either white on a black background or black on a white background.
Performing the amsler grid test
- Have the patient hold a white-on-black test card about 16 inches away with one hand and cover one eye with the other hand, an occluder, or a patch
- Direct the patient to stare at the centre dot and to report if any portions of the grid are blurred, distorted, or absent. The patient should not move the gaze from the centre dot, so that the presence of any distortion can be assessed
- If they answer yes, you may repeat the test with black-on-white Amsler recording chart, on which you ask the patient to mark the location of visual difficulties.
- If test results are normal, state so in the patient's record. If abnormal, state so, and include the Amsler recording chart in patient's record. The patient with abnormal findings is a likely candidate for further studies. The patient may also repeat this convenient procedure independently at home and report changes to the ophthalmologist's office (the patient should perform the test monocularly, always at the same 16-inch distance and under the same illumination)
Perimeters
The screen may be either an arc or a bowl of a radius of 330 mm.
Lister's perimeter: A rotatable arc, capable of being revolved round a pivot, and along which a test object can be moved
Goldmann perimeter: A hemispherical bowl over which a target (a spot of light of adjustable size and illumination) can be directed.
The Goldmann perimeter is more standardised and preferable for glaucoma examinations, as, both the central and peripheral visual fields can be recorded.
The targets of the perimeter consists of circular white discs (or a spot of light) of diameters ranging from 1-10 mm. The isopters represent the limits of the field of vision with each target, and are accordingly labeled 1/330 (1 mm target at 330 mm distance, the radius of perimeter), 2/330. 10/330, etc.
Coloured discs or coloured spots of light are especially used for estimation of a differential field loss to colour. In normal conditions, the blue field is largest, slightly smaller is the white, and then followed by the yellow, red and green.
Automated perimeter
Automated perimetry was developed to standardize visual field testing and to increase the reliability of visual tests. Various manufacturers make automated perimeters based upon computerized projection systems and a LED (light emitting diodes) system. Automated perimeters can perform screening and diagnostic field tests and can use kinetic and static methods. These perimeters are most often used for static threshold testing.
The most widely used automated perimeter is the Humphrey Field Analyzer which has become the standard for visual field testing.
Demato campimeter
The demato campimeter is a recently developed visual field screening device that is non-automated but has the advantages of being relatively simple, portable and much less expensive than automated perimeters. It's low cost and simplicity makes it more likely to be used in visual screening than many current automated instruments.
The demato campimeter consists of a white test card on which there is a single central point that acts as the test stimulus. Around the central point are a series of numbers arranged in a certain sequence. The patient views each of the numbers in sequence and responds to whether the central point can be seen for each.
Because the patient's fixation shifts, this is also known as autokinetic campimetry. The size and contrast of the central test stimulus can be varied on some models. Clinical studies of the Demato campimeter have given generally positive results.
Student exercise
Fill in the blanks
- _____________is called absolute scotoma.
- Traquair's definition of visual field is __________.
- In visual field testing if the fixation point is not seen, it is called _____ scotoma.
- Optic disc corresponds to _________ of the visual field.
- The field defect close to but not involving fixation is called __________.
Match the following
- Central fields - Blind spot
- Retinitis pigmentosa - Central scotoma
- Amsler's grid - Bitemporal heminanopsia
- Optic disc - Humphrey Field Analyser
- Chiasmal defect - Tubular field
- Automated perimetry - Bjerrum's screen
Short answers
- Define visual field
- Discuss visual field parameters
- Explain -blind spot
- Explain about central and peripheral field of vision
- Define scotoma and its types
- Explain kinetic and static perimetry with examples
- What do you mean by depression of visual field?
Short notes
- Discuss Traquair's concept of visual field
- Draw the structure of visual pathway and explain
- Discuss the field defects in glaucoma
- Discuss the types of visual field testing methods
- Tangent screen and testing procedures